Terapia peptického vredu.
Peptic ulcer
• defects of mucosa of the stomach / duodenum
= mucosal damage through the lamina muscularis mucosae
Clinical presentation : stomach
– pain in the epigastrium shortly after meal
(the patient often looses weight), nausea, anorexia duodenum – pain later after meal (fasting), often during the night, gets better after eating, the patient can gain weight
Etiopatogenesis
imbalance: aggressive factors ↔ protective factors mostlyHCl, pepsin mostlymucus, bicarbonate, fast regeneration of the production ↑ - histamine, acetylcholine, gastrin, mucosa, adequate perfusion of the gastric wall protective factors ↑ - mostly the production of etc.
prostaglandins by cyklooxygenase
Etiopatogenesis - causes
•
Helicobacter pylori (Hp)
• drugs- most frequently NSAIDs , then corticoids etc.
• smoking
• dietary mistakes (questionable)
• psychosocial stress
• genetical factors
• conditions with shock, burns, head traumas
• Zollinger- Ellison sy.
• ..........
Diagnosis and
Nonpharmacologic treatment
• ezophagogastroduodenoscopia histologic check of nature of the ulcer lesions presence of Hp = microscopy histo-morfology rapid urease test breath test testing of Ab (in plasma and in stool)
• nonpharmacol. therapy : lifestyle (sleep, ↓ stress) diet (often in smaller amounts, ↓ spicy, ↓ caffeine) no smoking
Peptic ulcer in the stomach
Peptic ulcer in the duodenum
Peptic ulcer in the duodenum
Helicobacter pylori
– black bacteria on the surface of the gastric mucosa
Pharmacotherapy of peptic ulcer
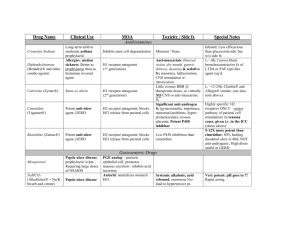
Antisecretory drugs (↓ production of HCl): proton pump inhibitors (PPI)- omeprazole
H
2 receptor antagonists - famotidine anticholinergics (Pslytics)- pirenzepine
Drugs neutralising HCl : coloidal antacids - compounds of Al a Mg reactive antacids - NaHCO
3 a CaCO
3
Mucoprotectives : prostaglandines, sucralfate, compounds of bismuth
ATBs : amoxicillin, claritromycin, metronidazole, doxycycline ; in case of failure of therapylevofloxacin, rifabutin
Antisecretory drugs
(↓ production of HCl)
Proton pump inhibitors
•
MA
– irreversible blockade of H/K-ATPase
(proton pump)
• most effective antisecretory drugs (inhibit the last phase of HCl secretion → effect independent from the stimulus for HCl secretion)
• elevated pH in the stomach decreases the conversion pepsinogen → pepsin
• “prodrugs“ - converted into active metabolite in the parietal cells of gastric mucosa
• good safety profile, good tolerance
• basic pharmacotherapy for peptic ulcer
Proton pump inhibitors
omeprazole : nearly complete blockade of HCl secretion at rest and after stimulus, high therapeutic effectivity drug interactions: diazepam, phenytoin, warfarin clopidogrel??- some studies- might ↓ effectivity of clopidogrel because of inhibition of CYP450- administer rather pantoprazole pantoprazole, lanzoprazole : less interactions, suitable in polymorbid and older patients esomeprazole : inovated omeprazole with faster onset and longer duration of action
Newer drugs: ilaprazol tenatoprazol: strongest effect, longest duration of effect
H
2
receptor antagonists
MA - selective blockade of H
2 histamine receptors → inhibition of histamine mediated HCl production (indirect effect on secretion mediated by Ach and gastrin)
- ↓ effectivity than proton pump inhibitors
Examples
– cimetidine, ranitidine, famotidine
(more effective) , nizatidine
- good safety profile, good tolerance
drugs of 2nd choice for treatment of peptic ulcer; loosing therapeutic role in most indications (↓ effectivity)
Anticholinergics
MA
– inhibition of M
1 receptors → inhibition of acetylcholine mediated HCl production
- ≈ same effectivity as H
2 antagonists
ADRs
– consequences of ↓activity of PS – for example dry mouth, problems with vision and urination, constipation
- examplepirenzepine
they lost their therapeutic role
– ADRs, ↓ effectivity than proton pump inhibitors
Drugs neutralising HCl :
(antacids)
• coloidal antacids: aluminum and magnesium hydroxide
MA: weak bases → bind HCl; slightly ↑ the production of prostaglandines
ADRs: - Al hydroxide: constipation, ↓ resorption of phosphates → osteomalacia; - Mg hydroxide: diarrhoea, hypermagnesemia; both- risk of interactions!!
• reactive antacids:
NaHCO
3 and CaCO
3
MA: reaction with HCl, during which CO
2 is formed
ADRs: - flatulence, ´milk-alkali´ syndrome
(hypercalcemia, nephrolithiasis, renal insufficiency, ...), in the case of NaHCO
3 metabolic alkalosis !!!!
Antacids – only for symptomatic treatment of dyspepsia!!!
Mucoprotectives
Prostaglandines
• misoprostol (analog of PGE
1 of PGE
2
)
) , enprostil (analog
cytoprotective and mucoprotective effect improve the microcirculation underneath the mucosa + ↑ production of mucus and bicarbonate + ↑ regenerationof defects
ADRs
– diarrhoea, stomach pain, abortion,
can be used in prevention of peptic ulcer formation during NSAID treatment (for that, we have other, in most cases better alternatives)
Sucralfate
• salt of sulfonated sucrose
•
MA : in an acidic environment it forms a protective layer on the surface of the mucus membrane and on the surface of the defect
• probably stimulates the formation of prostaglandines
• well tolerated
• !don´t administer after administration of antisecretory drugs!
• seldomly used
Bismuth
-
↑ secretion of mucus and bicarbonate,
↓ secretion of HCl, antibacterial effect
ADRs
– metallic taste in the mouth, black tongue and stool, !neurotoxicity (confusion, hallucinations...) nowadays used less frequently (risk of ADRs), part of 2nd line of H. pylori eradication therapy
Eradication of
Helicobacter pylori
(needed for long-term success of pharmacotherapy of peptic ulcer in Hp positive patients)
1st line treatment : triple therapy
7 or14 day treatment (14 days – better results)
• proton pump inhibitor
• claritromycin
• amoxicillin – if PNC allergy metronidazole problem – decreasing effectivity of the treatment (fails in approximately 25-30 % of patients)
2nd line treatment : quadruple therapy
(in case of failure of triple therapy; in patients treated with macrolides in the past; can be considered in patients with
PNC allergy)
7 or14 day treatment (14 days – better results)
• proton pump inhibitor
• bismuth
• metronidazole
• doxycycline problem – decreasing effectivity of the treatment
– possibility of ↓ compliance
(dosing scheme)
– ADRs (mostly bismuth)
New possibilities : sequential therapy
10 days (5 + 5), for example:
First 5 days
• proton pump inhibitor
• amoxicillin
Next 5 days
• proton pump inhibitor
• claritromycin
• tinidazole (possibly metronidazole ??)
Failure of the therapy:
Future?? :
Non-steroidal anti-inflammatory drugs (NSAIDs) and peptic ulcer
NSAIDs – one of the most widely used drug groups
– in roughly 25 % of chronic users can cause erosions and ulcerations in the GIT, in 2-4 % perforation or bleeding
Possibilities of prevention – proton pump inhibitors or misoprostol during NSAID treatment; use of NSAIDs selectively inhibiting COX-2
Strategy
– small risk of ulcer –
NSAID on its own
– moderate risk of ulcer – NSAID + PPI / misoprostol
– high risk of ulcer – a) administer other (non-NSAID) analgesics , or b) COX-2 selective NSAID + PPI / misoprostol