Phyllis Kanki, Harvard School of Public Health - I-Tech
advertisement

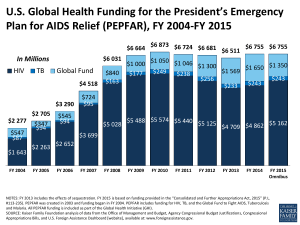
Phyllis Kanki Harvard School of Public Health VIIIth Annual Track 1.0 ART Meeting August 2010 Harvard PEPFAR program Nigeria 750,000 140 Million Tanzania 420,000 36 Million HIV Infection AIDS Cases Initiated on ART Botswana 100,000 2 Million 0.0 0.5 1.0 Million 1.5 2.0 2.5 3.0 HIV Care and Treatment Botswana Nigeria Tanzania Total Persons ever enrolled in HIV Care 18,975* 118,688 95,389 233,052 Persons ever initiated on ART 13,578* 76,166 61,433 151,177 154 26 50 230 --- 61 133 194 Number of ART Facilities Number of PMTCT Facilities •Clinical master trainers – adult patients only MDH supported sites in Dar es Salaam (n=50) PUBLIC PRIVATE Collaborating institutions (MDH): Muhimbili University of Health & Allied Sciences (MUHAS) Dar es Salaam City Council Harvard School of Public Health Ever initiated ARVs 61,433 (8% children) Total ever enrolled 95,389 (7.6 % children) Active on ARVs 45,699 ( 7.6 % children) June 2010 Patient retention 25.6% of patients ever initiated ARVs are not active Timely tracking of patients who missed their appointment dates at the clinic by phone calls or physical visits. Major reasons: Deaths Transfers Refusal to continue Unknowns 6035 (95.8%) of missing patients were tracked for the last quarter 73.4% of those tracked had their vital status ascertained Patients retention Future Plans to improve tracking Pairing of counselors/clinicians with a number of patients Improve understanding, communication and interaction with patients Create bond between patients and their counsellor/clinicians Counsellors/clinicians will be able to follow up patients development Make use of existing NGOs (Pathfinder) who work at community level Introduce electronic model of tracking, recording and reporting PMTCT Achievements (133 sites) OctDec 08 JanMar 09 AprJun 09 JulySept 09 OctDec 09 JanMar 10 AprJun10 Total tested 19,335 21,116 20,741 21,808 25,937 28,166 24,298 Overall prophylaxis 26.7% 33.7% 51.5% 69.6% 56.6% 61.2% 80.5% HIV exposed infants registered - 518 549 356 310 1357 1389 Confirmed +ve - 7 2 1 1 94 98 Cotrimoxazole Prophylaxis - 371 13 184 205 179 229 EID Sites - 13 13 14 42 58 65 7% infection Public – Private Partnership (PPP) There is significant contribution from private hospitals • 6.5% of patients from MDH supported sites are treated at private hospitals • Contribute in offloading patients from already overwhelmed public sites • Provide more options for the patients • Contribute towards “access to all strategy” Botswana’s Masa ART Program 121,644 patients on ART in the public sector at present (May 2010) 61.4% female; 6.3% children 14,995 patients out-sourced from the public to the private sector –(Public-Private-Partnership [PPP]) 13,394 patients in the private sector (Medical Aid Schemes and the Work-place Programs) TOTAL: 150,033 (92.8% of need for adults and children) BHP-PEPFAR ARV Site Support Program Masa Master Trainer/ARV Site Support Program Clinical Laboratory Monitoring & Evaluation Unit Linked to: • All ARV sites • Other MOH programs Clinical Master Trainer Program : ARV Sites Assessed and Supported Masunga Newxade Kalkfontein Palapye Werda Bokspit Goodhope Middlepit Mother Sites Each Mother Site has 3-4 Clinics Task Sharing Nurse Prescriber & Dispenser Training to Date - 246 nurses trained in prescribing and dispensing ARVs - 680 nurses trained in ARV dispensing only Nurse training for Rapid HIV testing and Dried Blood Spot collection in collaboration with PMTCT (38 trained in 4 trainings this quarter) Laboratory Capacity Building At start of PEPFAR – 2004: 2 HIV reference labs performed all CD4 and Viral Load testing for the country In 2010: Botswana Lab Master Trainers have trained and supported ALL decentralized labs and private sector labs which run PPP specimens CD4s - 24 decentralized labs performing 62% VL – 10 decentralized labs performing 33% Reasons for Site Support Calls Analysis of 100 calls from BHP Master Trainers Telephone Site Support New Initiatives Patient Information Management System –currently developing integrated PIMS II system for PMTCT, HCT, ARV and planning roll-out Pharmacovigilance Failure Management Registries Adolescent –focused programs and training First data collection for Quality Improvement Updated analysis of integrated MASA dataset that now has records for over 110,000 patients Harvard PEPFAR Nigeria •Through Bill & Melinda Gates funding, Harvard has been working with multiple hospitals and prevention programs in Nigeria since 2000 •Started PEPFAR ART activities at 6 tertiary hospitals in 2004 and expanded to a total of 26 sites. •Transitioned 14,100 ART current patients to APIN Ltd Year 1 Year 2 Year 3 Year 4 Year 5 Year 6 18,518 36,504 59,051 75,512 113,567 449 1,132 2,167 3,060 5121 12,165 23,108 38,050 55,793 72,906 97 485 1,284 1,951 3,260 Cumulative in Palliative Care Adults 6,151 Pediatrics Cumulative on ART Adults Pediatrics 2,760 Time-to-failure: Patients identified by both criteria Median time to % Treatment Success 11.1 mo. virologic failure 11.1 months Virologic Failure 15.3 mo. Immunologic Failure Median time to CD4 failure 15.3 months Viral load monitoring identified failure significantly earlier than CD4 criteria (p<0.0001) Patients maintained on virologically non-suppressive ART over a median of 6 months developed an average of 1.96 IAS-mutations with a loss of 1.25 active drugs (Cozzi-Lepri et al. AIDS 2007; 21:721.) TDF-3TC-NVP (n=813) is Inferior to AZT-3TC-NVP multivariate analysis on virologic failure Failure at 12 months was 16.1% for TDF-3TC-NVP versus 9.5% AZT-3TC-NVP K.Scarsi et al. Vienna, 2010 PMTCT Transmission Rates (n=5320) No statistically significant difference between ART and mono or bi-ART prophylaxis Meloni et al, 2010 Patient Monitoring: Pharmacy Database Adherence Utility -------------------------------------BLANKED OUT----------------------------- • Assess adherence to treatment based on timeliness of drug pick-ups • Use calculation of average percent adherence • Setting up networks so that pharmacists can cross-check prescriptions Ahmadu Bello University Teaching Hospital Loss to Follow up Rate Lower in ARV Experienced vs. Naïve Patients n= 3001 100% Cohort 1 Naïve Cohort 1 Experienced Cohort 2 Naïve Cohort 2 Experienced Cohort 3 Naïve Cohort 3 Experienced % Lost to Follow-Up 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 1 2-3 4-6 7-9 10-12 Months on ART 13-18 19-24 25-30 31-36 Comparison of LTFU among Large Treatment Programs in Africa Country # Patients Analyzed Duration of Follow-up LTFU rate Comments: LTFU definition South Africa CID 2006; 43:770. 1235 pts (Sep 02 -Aug 05) 35 months 33.3% early mortality (2.3% LTFU) LTFU: >4 weeks late for scheduled visits and were not deaths or transfers South Africa JAIDS 2008; 47(1):101. 1631 pts (Apr 04 - Jun 05) 15 months 16.4% LTFU during 15 mo F/u LTFU: >6 weeks with no visit or pharmacy pick-up Nigeria PLoS 2010; 5(5):e10584. 5760 pts (Mar 05 - Jul 06) 16 months 26% lost at any time during 16 month follow-up LTFU: Did not return >60 days from expected visit Risk factors: CD4>350 or <100, etc. Nigeria ABUTH LTFU Data 3001 pts (Jun 06 May 09) 35 months 22.6% LTFU at 12 months of follow-up LTFU: >2 months since missed visit or pick-up Assessment of causes of early & late LTFU may elucidate potential interventions APIN/PEPFAR Sites: 2010 Federal Medical Centre Nguru University of Maiduguri Teaching Hospital State Specialist Hospital Maiduguri Nursing Home Maiduguri Ahmadu Bello University Teaching Hospital University of Ibadan College of Medicine 3 Satellites under UCH Adeoyo Maternity Hospital 43 Oyo DOTS Centres Sacred Heart Catholic Hospital Lantoro Jos University Teaching Hospital Our Lady of Apostles Hospital Jos 8 Satellite Hospitals, 44 PHCs Federal Medical Centre Makurdi University of Nigeria Teaching Hospital 68 Nigerian Military Hospital Creek Hospital Nigerian Institute for Medical Research University of Lagos, College of Medicine PHC-Iru Victoria Island Sites Under APIN Ltd Widowcare Abakiliki Ebonyi Lagos University Teaching Hospital Mushin General Hospital Onikan Women’s Hospital Sites Under Harvard PEPFAR APIN Program Office • Continual training is a critical foundation for optimal prevention, treatment and care programs and sustainability • Rigorous program evaluation is critical to inform national guidelines and insure optimal care. • Developing systems for program outcome and impact will facilitate country ownership and sustainability Botswana Tanzania R. Marlink W. Fawzie P. Burns G. Msamanga T. Gaoloathe D. Mtasiwa J. Mukhema G. Chalimilla N. Ndwapi S. Kaaya I. Thior C. Hawkins M. Mine S. Ismail C. Bussmann M. Mwanyika-Sando Nigeria P. Kanki R. Murphy J-L Sankalé B. Chaplin K. Scarsi B. Taiwo P. Okonkwo E. Ekong T. Jolayemi R. Olaitan S. Ochigbo O. Idigbe S. Ogunsola M. Garbati I. Adewole D. Olaleye D. Owujekwe O. Eberndu S.Meloni S. Hosseini H.Rawizza A. Ojesina K. Hurt A.Dieng Sarr J. Samuels P. Akande B. Aluko S. Sagay O. Agbaji S. Akanmu W. Gashau C. Okany R. Nkado H. Muktar J. Abah N. Nulenga