Rwanda Health Sector Achievements
advertisement

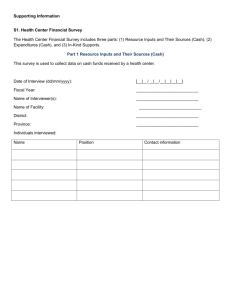
Republic of Rwanda Kivu 2010 Leadership Retreat Rwanda Health sector achievements Reporting on progress since the Leadership Retreat, and looking ahead to the next quarter (case scenario) Domestic Funding; Saving lives Building a Health System WHO-recommended health worker density: 2.3 per 1,000 pop. Rwanda’s health worker density: 0.84 per 1,000 pop. Referral Hospital (5) Physician Specialist (150) District Hospital (34 to 42) Health Center (234 to 469) New : 3 Referral 4 Provincial Physician Generalist (475) Nurse Generalist (8,273) Health post Community Level (0 to 14,837) ~80% of burden of disease addressed here Community Health Workers (45,011) 2 Health Financing system • Rwanda put together all collective effort aiming at increasing innovative domestic resource to finance in the health sector • In order to ensure long term sustainability of interventions, Rwanda has been ensuring increase in budgeting every year: e.g 2012-2013:16.05%, 2013-2014: 17.36% This is above the 2002 Abuja declaration set target of proportion of national budget used for Health. Why efficient management of funds • Comply with GOR Aid policy : Accountability for all • Ensure efficient use of GOR & Partners funds • Proceed with sub sector comprehensive planning process linked to the Sector Strategic Plan & Funds mobilisation : Synchronisation , synergy & sustainability • Set up an Implementation framework of health Subsector strategic plans : Define who is doing what ? , how? , when? With which Means/ressources ? Measurement of achievments(frequency, tools ,external verification ? Vaccination Coverage in Rwanda 100% 80% BCG DTP (3) 60% Measles Polio (3) 40% 20% 0% 1990 1995 2000 2005 Adapted from: World Health Organization. (2012). WHO-UNICEF vaccination coverage estimates time series for 2010 5 6 Child Mortality in Rwanda, 1990 – 2011 300 275 Rwanda Sub-Saharan Africa 250 200 World 183 178 170 154 Probability of child dying by age 5 per 150 156 1,000 live births 133 108 112 109 100 87 82 50 73 60 63 54 53 51 59 52 29 0 1990 1995 2000 2005 2010 2015 MDG Target Farmer PE, Nutt CT, Wagner CM, Sekabaraga C, Nuthulaganti T, et al. (2013). “Reduced Premature Mortality in Rwanda: Lessons from Success.” British Medical Journal 346(f65): [e-pub ahead of print]. Progress Against Child Mortality and Health Expenditure Per Capita Around the World* 12% Rwanda Botswana Estonia 10% Belarus Oman Cambodia 8% China Brazil Portugal Liberia Child mortality annual rate of 6% decline, 2000-2011 Malawi Ethiopia Ireland MDG 4 cutoff: 4.4% 4% 2% 0% $10 $100 $1,000 $10,000 Total health expenditure per capita, 2010 (log) *Only countries with populations greater than 500,000 included. Farmer PE, Nutt CT, Wagner CM, Sekabaraga C, Nuthulaganti T, et al. (2013). “Reduced Premature Mortality in Rwanda: Lessons 7 from Success.” British Medical Journal 346(f65): [e-pub ahead of print]. Annual Rates of Decline in Child Mortality by Wealth Quintile and Residence, DHS 2010 (measures 10 years preceding survey) 18.5% 15.1% 15.2% 15.1% 11.9% 5.7% 3.6% Lowest Second Middle Fourth Highest Rural Urban National Institute of Statistics of Rwanda, Macro International, Inc. (2012). Rwanda Demographic and Health Survey 2010. 8 Calverton, MD: Macro International, Inc. Towards reducing premature death in Rwanda Timeframe Decline in Mortality Malaria (reported deaths) 2005 – 11 85.3% HIV/AIDS (rate) 2000 – 09 78.4% Tuberculosis (rate) 2000 – 10 77.1% Child mortality (rate) 2000 – 11 70.4% Maternal mortality (ratio) 2000 – 10 60.0% All-cause mortality (rate) 2000 – 10 50.0% Cause Non Communicable diseases ???? Farmer PE, Nutt CT, Wagner CM, Sekabaraga C, Nuthulaganti T, et al. (2013). “Reduced Premature Mortality in Rwanda: Lessons 9 from Success.” British Medical Journal 346(f65): [e-pub ahead of print]. SAMU/PHECS (Pre-Hospital Emergency Care Service) • 912 – call center • 223 ground ambulances nationwide • 10 resuscitation ambulances in CoK • 1 water ambulance in Lake Kivu. Health Financing sustainability • Community based health insurance (CBHI) – Coverage rate of 90.7% in 2011/12, 78.55% in 2012-2013 • 16 billions contribution • National budget • Performance based financing (PBF) – Increased quality of care (hygiene, customer care and financial management) • Innovation in financial management – Equalization fund to incentive providers to work and stay in rural areas – Professional hospital managers – Self sustained community care PPCP (Public Private Community Partnership) • Health post – drugstores and paid for point of care • 420 CHWs Cooperatives 70% indivisible benefices paying for care Household and Out of Pocket Spending 1998 2000 2002 2003 2006 2009/10 32 % 26 % 31 % 20 % 26 % 15 % 33 % 25 % 25 % 17 % 23 % 11 % RWF 1,994 RWF 1,371 RWF 1,436 RWF 1,664 RWF 4,510 RWF 2,378 $3.43 $2.35 $2.47 $2.86 $7.75 $4.09 Household expenditures as % of Total Health Expenditures Household Out-of-Pocket as % of Total Health Expenditures OOP per capita (constant 2009/10) Figures from the 2010 DHS and the table below show that Rwanda has made tremendous progress in reducing out-of-pocket expenditure both as a percentage of total health expenditure and in absolute terms Household expenditures as % of Total Health Expenditures (as a source) 35% 30% 25% 20% Household expenditures as % of Total Health Expenditures (as a source) 15% 10% 5% 0% 1998 2000 2002 2003 2006 2009/10 Proportion of Co-payment on total healthcare expenditures for CBHI and RAMA patients 3,473,080,407.59 Paid by Insurance schemes/GoR/Donor s Copayment 25,851,707,360.70 • Under all health insurance schemes members are required to contribute to the cost of care by paying a co-payment • In 2011/12 the total amount of co-payment paid by CBHI members was RWF 1.851.275.515,30. • In the same year RSSB members paid RWF 1.621.804.892,29 in copayment Contribution to Global Fund. • As a country, we pledged and contributed to the third replenishment of the Global Fund equivalent amount of usd 1.000.000 I thank you for your kind attention.
![Government of [Rwanda] - UNDP-UNEP Poverty](http://s2.studylib.net/store/data/005359438_1-2c42f5844b4637cd375e392bd4b49b8d-300x300.png)