Chapter 8 - Psychology for you and me
advertisement
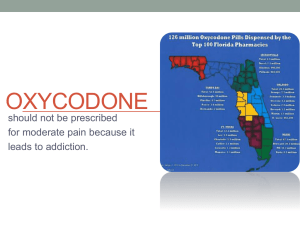
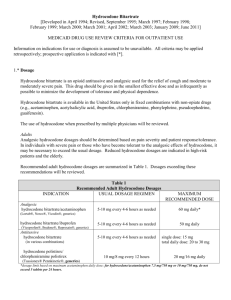
I. Medical Treatments for Stress and Pain Medical treatments for stress and pain are those treatments that follow conventional Western medicine, but many alternatives exist, which we explore in the next section. A. Medical Treatments for Stress-Related Disorders Stress does not typically warrant medical treatment, but treatment for stress-related disorders such as PTSD may include drugs such as a tranquilizers or antidepressants. B. Medical Treatments for Pain Acknowledging that treatment for pain is often inadequate, the U. S. Congress declared the years 20012011 to be the Decade of Pain Control and Research. Treatment of acute pain is easier than for chronic pain, but both present challenges. 1. Drugs Analgesic drugs are the most common treatment for acute pain. These drugs fall into two groups: opiates and non-narcotic analgesics. Opiate drugs have powerful analgesic effects but also produce tolerance and dependence. However, the fear of drug-related problems, such as addiction, leads to under-medication more often than to drug abuse. The recent increase in the use prescription analgesic drugs was due mostly for the demand for oxycodone and hydrocodone, both of which are opiates with a potential for abuse. FYI :Oxycodone vs Hydrocodone Oxycodone and hydrocodone are two highly debated drugs often prescribed to relieve extreme pain. They are classified as narcotic analgesics. Being such, they can lead to some health hazards when not used as prescribed. The two are chemically similar and they give off almost the same range of side effects. But surprisingly, they also have lots of differences. Hydrocodone is usually prescribed by the doctor as a remedy for minor to moderate degrees of pain and, at the same time, helps manage coughing. Oxycodone, on the other hand, is considered to be more potent than the former because it is about 5 times more effective in pain suppression. Therefore, oxycodone is given to patients suffering from more severe pain like those related to trauma, chronic pain injuries and even cancer-related pains. Although both hydrocodone and oxycodone have preparations that are classified as Schedule II narcotics, all other drugs that contain oxycodone like Tylox, Percocet and Roxilox are still placed under schedule II while the drugs that contain hydrocodone are only placed under Schedule III. Examples of such are Lortab, Lorcet and Vicodin. This means that Oxycodone has a higher potential for abuse compared to the former. Usually, acetaminophen is the other drug component added to the mixture to make the variety of branded hydrocodone and oxycodone medications. Due to the strength of oxycodone, the doctor can’t just do a ‘call in’ of the drug at the pharmacy. There must be a written prescription for someone to be able to buy such a controlled drug. For the case of hydrocodone, the doctor can simply make a ‘call in’ for the drug to be released. Lastly, both oxycodone and hydrocodone are available in their own generic forms. But it is only oxycodone which has a single ingredient preparation. This means that all hydrocodone medications are in combination with other drug components like (as mentioned) acetaminophen. With regard to the effectiveness in pain management, both can do the job although a lot of patients would testify that they were easily relieved by using oxycodone. Nevertheless, this is a case to case basis as some would claim otherwise. FYI:Oxycontin vs Oxycodone A number of people wonder if there is a difference between oxycontin and oxycodone. Are they the same medicines? Is oxycodone just a generic name for oxycontin? We’ll address these questions and other differences between the two: Oxycodone hydrochloride is an opioid painkiller. It can be found in a number of prescription medications. When it is available by itself, it is available in the form of oxycontin. Oxycodone is also found in combination with other ingredients on a number of prescription medications e.g. Percocet. The main difference between the two relates to the onset of action. Oxycontin is a time released drug. This means that it acts over a period of time. Usually, oxycodone medications need to be taken every four to six hours. However, Oxycontin continues acting for at least 12 hours. That is why it needs to be taken only twice a day. You may come across certain articles that categorize oxycodone as a generic name for oxycontin because it is the active substance in the medication. However, it would be incorrect to say that because oxycodone is an active ingredient in other medications also. Most experts prefer calling oxycontin ‘oxycodone extended release’. Oxycontin vs Oxycodone The two medications are prepared in a different manner. Though oxycontin contains more of oxycodone, it is also prepared in a manner that releases the medication gradually into the blood. So, even though the dosage is large, it is released slowly into the blood stream. Oxycodone is often used together with other chemicals in other medications like Percocet. The dangers of over dosage in oxycontin are more pronounced. Since the amount of oxycodone is large, lack of a sustained release may have severe effects on the patient. This is especially true for first time users. The danger becomes more apparent in the case of addicts who break open the capsule and snort it in. A common problem with quick acting painkillers is that they become nearly ineffective within a few hours. The action peaks within a few minutes, but falls within a few hours. Oxycontin aims at doing away with this problem by going for a sustained release. 1. Drugs Aspirin and the other non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen sodium, as well as acetaminophen drugs, are all useful in managing minor pain, especially pain due to injury. Antidepressant drugs and anti-seizure drugs also affect pain perception and may be useful in pain management for some people. 2. Surgery Surgery may be directed either to repairing damage that causes pain or to altering the nervous system to change pain perception. 2. Surgery Surgery is an attempt to control low back pain more often than other pain syndromes, and specific nerves or the spinal cord may be targets. 2. Surgery Surgery may also be used to implant devices to stimulate the spinal cord to decrease pain, and a related technique is transcutaneous electrical nerve stimulation (TENS), which uses electrical impulses to stimulate skin stimulation to block pain messages. Spinal cord stimulation is more effective than TENS. 3. Limitations of Physical Treatment Medical treatments are typically the first choice for acute pain, but they are less successful with chronic pain. Opiate drugs, the most effective analgesic drugs, have the potential to produce tolerance and dependence, making health care professionals reluctant to prescribe adequate doses. 3. Limitations of Physical Treatment Surgery is not always effective, either in repairing damage or in producing pain relief, especially for people with low back pain. II. Alternative and Complementary Medicine Both the biomedical and biopsychosocial models of medicine arose within Western medicine, but other cultures hold different views of health and disease and alternative treatments. Alternative medicine may come from other cultures or from practices that are not well accepted by conventional practitioners. II. Alternative and Complementary Medicine When people combine these alternative treatments with conventional approaches, the term complementary medicine is appropriate. II. Alternative and Complementary Medicine Treatments that are alternative may become part of conventional medicine over time and with evidence for their effectiveness. The U. S. National Center for Complementary and Alternative Medicine is an agency created to prompt evaluation of alternative treatments. A. Complementary and Alternative Treatments for Stress and Pain A wide range of techniques from complementary and alternative medicine (CAM) is available for managing stress and pain. These techniques include manipulation techniques and movement-based therapies. A. Complementary and Alternative Treatments for Stress and Pain 1. Manipulation Techniques Manipulation techniques include massage, chiropractic manipulation, and acupuncture. Massage involves manipulation of the soft tissue and can be therapeutic for either stress or pain. A. Complementary and Alternative Treatments for Stress and Pain Chiropractic manipulation of the spine can be as effective as analgesics in controlling back and neck pain. Acupuncture is an ancient Chinese form of analgesia that consists of inserting needles into the skin and stimulating or manipulating the needles. The effects are not due to the placebo effect but are rarely sufficient to produce a high degree of analgesia. However, acupuncture can be effective in helping people with back, neck, or joint pain. Acupressure is the application of pressure rather than needles to the points used in acupuncture. 2. Movement-Based Therapies Two movement-based therapies have come from traditional Chinese medicine, qi gong and tai chi chuan. Both include a set of movements and exercises that are intended to balance the body’s energy and restore health. Both promote relaxation, flexibility, and balance and thus can be helpful in managing stress and some types of pain such as arthritis pain. B. Who Uses Complementary and Alternative Medicine? The prevalence of CAM varies, depending on what is included in the definition. When prayers for health are included, 63% of people in the U. S. used some type of CAM in the year before the survey. Excluding prayer, 36% used some CAM approach. Most people use these techniques as complementary and not as alternative medicine. Well-educated Whites are most likely to be users, but some immigrants who hold to the traditions of their native culture continue with these approaches. Women are more likely than men to use CAM. C. Limitations to Alternative Therapies The main limitation to CAM is the sparse research on its effectiveness, but that research is growing. Research indicates that massage is effective for pain and stress, but those benefits do not persist beyond the treatment. Similarly, chiropractic manipulation may be effective for back and neck pain, but the effectiveness does not persist once the treatments are discontinued. C. Limitations to Alternative Therapies Acupuncture does not work for everyone, even for the conditions for which it is effective for some people. The movement-based therapies of qi gong and tai chi chuan pose few hazards and offer benefits for stress; but their advantages are not specifically established, except for balance in older people. D. Integrative Medicine The movement toward integrative medicine comes from practitioners in both conventional and alternative medicine, who propose that an integration of these two treatment approaches would be beneficial to patients. This type of integration faces the challenge of melding very different philosophies of treatment but offers the promise of benefits from both approaches. Some pain clinics and wellness centers attempt this goal. III. Behavioral Techniques for Managing Stress and Pain Some people classify behavioral techniques as alternative treatments, but others consider these approaches within conventional medicine because of the research support for their effectiveness. A. Relaxation Training Modern uses of relaxation training can be traced to Edmond Jacobson who developed progressive muscle relaxation during the 1930s. 1. What Is Relaxation Training? Several forms of relaxation training exist, but the ones most frequently used to manage stress and pain are: (1) progressive muscle relaxation, (2) meditative relaxation, (3) mindfulness meditation, and (4) guided imagery. With progressive muscle relaxation, patients learn to relax the entire body, one muscle group at a time, and to breathe deeply and exhale slowly. Herbert Benson's meditative relaxation combines muscle relaxation with a quiet environment, a repetitive sound, and a passive attitude. 1. What Is Relaxation Training? Mindfulness meditation does not involve a focus on any specific thing but permits people to allow a flow of thoughts without evaluation or censoring and to gain insight into personal motivation and thoughts. Guided imagery asks patients to imagine a peaceful image and to concentrate on that image throughout the stressful or painful situation. 2. How Effective Is Relaxation Training? All four approaches have had some success in helping patients cope with stress and pain. Relaxation is an effective technique for coping with stress but probably not sufficient for pain management. Meditation, mindfulness meditation, and guided imagery can be effective for both stress management and pain control (see Table 8.2). B. Hypnotic Treatment Hypnotic treatment can be traced almost to the beginning of human history, but modern hypnosis is usually traced to Franz Mesmer during the last part of the 18th century. 1. What Is Hypnotic Treatment? Authorities disagree on a definition of hypnotic treatment, but most recognize its potential for controlling pain and reducing stress. 1. What Is Hypnotic Treatment? Joseph Barber and Ernest Hilgard see hypnosis as an altered state of consciousness, whereas Theodore X. Barber views hypnotizability as a generalized trait. Moreover, Hilgard believes that induction (being placed in a hypnotic state) is central to hypnotic treatment, but Barber holds that hypnosis can be effective without the trancelike state. Most authorities agree that hypnosis includes focused attention and that all hypnosis is self-hypnosis. 2. How Effective Is Hypnotic Treatment? Although hypnotic treatment is an important tool in the arsenal of the pain therapist, it is not effective for every pain or every patient. For suggestible subjects, hypnotic treatment works better than a placebo and provides high levels of relief from a variety of pains, especially acute pain. 2. How Effective Is Hypnotic Treatment? However, low suggestible subjects respond no better to hypnosis than to a placebo, and hypnosis is not very effective for chronic low back pain or headaches. Hypnosis could be more useful, but its use is limited by widespread misunderstandings among the general public and among health care professionals (see Table 8.3). C. Biofeedback Biofeedback is the process of providing feedback information about the status of biological systems. 1. What Is Biofeedback? Biofeedback techniques involve the electronic measurement of various biological responses and the immediate relaying of that information to the person being tested. This immediate feedback permits the person to alter physiological responses that could not have been voluntarily controlled without the feedback. 1. What Is Biofeedback? The two most frequently used biofeedback procedures for coping with stress and pain are the electromyograph (EMG), which measures electrical discharge in muscle fibers, and thermal (temperature) biofeedback, which uses a thermister to measure skin temperature. Raising skin temperature is a goal in treating Raynaud’s disease, a disorder involving peripheral vascular constriction. 2. How Effective Is Biofeedback? Because biofeedback requires expensive technology and trained personnel, it must be more effective than hypnosis and relaxation to warrant its expense. In general, biofeedback has failed to demonstrate this advantage. Studies have shown that biofeedback is as effective as relaxation or hypnosis, but few studies have indicated an advantage for biofeedback in controlling any stress or pain problem (see Table 8.4). D. Cognitive Behavioral Therapy Behavior modification techniques are based on the principles of operant conditioning and are used by health psychologists to help people cope with stress and pain. The goal of behavior modification is to shape behavior, not to alleviate feelings of stress or sensations of pain. 1. How Has Behavior Modification Contributed to Pain Management? People in pain usually communicate their pain to others by complaining, moaning, sighing, limping, rubbing, grimacing, or missing work, which are behaviors that may continue because they receive positive reinforcers such as attention, sympathy, financial compensation, relief from work, and other rewards. Positive reinforcers may create pain traps that turn acute pain into chronic pain. The rationale behind behavior modification is to train people in the pain patient’s environment to discontinue reinforcement for pain behaviors, thus avoid the pain trap. Progress is measured in terms of observable behavior, such as amount of medication, absences from work, physical activity, and so forth. Behavior modification does not address the cognitions that underlie behavior. 2. How Does Cognitive Therapy Help in Managing Stress and Pain? Cognitive therapy rests on the assumption that a change in the interpretation of an event can change people's emotional and physiological reaction to that event. Because pain and stress are at least partially due to psychological factors, cognitive therapy attempts to get patients to think differently about their stress or pain experiences and to increase their confidence that they can cope with them. 3. What Is Cognitive Behavioral Therapy? Cognitive behavioral therapy aims to develop beliefs, thoughts, and skills to make positive changes in behavior. Dennis Turk and Donald Meichenbaum have developed a cognitive behavioral program for pain management, and Meichenbaum and Roy Cameron have developed a parallel strategy for managing stress called stress inoculation training. 3. What Is Cognitive Behavioral Therapy? These inoculation techniques have a similar approach and include the same stages: (1) a re-conceptualization stage in which patients are encouraged to think differently about their stress or pain experiences, (2) an acquisition and rehearsal of skills stage when patients are taught relaxation and controlled breathing skills, and (3) a follow-through stage in which patients apply their coping skills to their daily environment. 4. How Effective Is Cognitive Behavioral Therapy? Research has supported the effectiveness of inoculation programs for managing stress and for managing pain. Other types of cognitive behavioral programs have demonstrated effectiveness in helping people manage a wide variety of problems, including rheumatoid arthritis, headache, cancer, AIDS, and low back pain (see Table 8. 5). E. Emotional Disclosure James Pennebaker and his associates have demonstrated the therapeutic value of catharsis, that is, expressing emotions through talking or writing about them. 1. What Is Emotional Disclosure? Emotional disclosure is a therapeutic technique whereby people express their strong emotions by talking or writing about the traumatic events that precipitated those emotions. The sessions typically last about 15 to 20 minutes, three or four times a week. Emotional disclosure is different from emotional expression, which involves emotional outbursts or emotional venting, such as crying, laughing, yelling, or throwing objects. Emotional disclosure, in contrast, involves the transfer of emotions into language and thus requires a measure of selfreflection. 1. What Is Emotional Disclosure? In an early study, Pennebaker and colleagues asked survivors of the Holocaust to talk for 1 to 2 hours about their war experiences. Those survivors who disclosed the most personally traumatic experiences had better subsequent health than survivors who expressed less painful experiences. 2. How Effective Is Emotional Disclosure? Emotional disclosure has brought about decreased distress and improvements in physical conditions such as asthma and arthritis. When people are urged to find a less negative interpretation for their trauma, they benefit additionally from the process of emotional disclosure (see Table 8.6 for a summary of research on emotional disclosure).