Free-Living-Amoeba
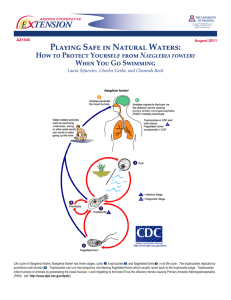
advertisement
free-living amoebae causing human infections _ are normal inhabitants of soil and water where they feed on bacteria. _ A few members have the ability to become facultative parasites when an opportunity to enter a vertebrate exists. _There are able to infect humans Naegleria fowleri Acanthamoeba spp. Naegleria fowleri When a victim swims or sinks into freshwater. - all victims have had a history of swimming in freshwater lakes or ponds or swimming pools a few days before the onset of symptoms Naegleria fowleri _ Naegleria fowleri is a free living brain-eating amoeba. _ Typically found in warm fresh water (thermo tolerant amoeba). _ worldwide distribution. _ It exists in trophozoite and cyst forms and in a transient flagellate stage. _ Naegleria fowleri is the causative agent of primary amebic meningoencephalitis (PAM). _ The period incubation is short, the symptoms are acute, and death is almost certain and rapid. _Naegleria fowleri invades the C.N.S. via penetration of the olfactory mucosa and nasal tissues (nose). _ Since Naegleria fowleri trophozoites and cysts are susceptible to chlorine, swimming pools should be adequately chlorinated. Naegleria fowleri Naegleria fowleri • Structures of the amoeba form are : Trophozoit and flagellate . • The infective stage is trophozoit stage • Method of transmission is by penetrate the mucosal layer of olfactory tissue and nasal cavity • Leads to Primary amebic meningoencephalitis • Most symptoms involving fever , headache, stiff neck and confusion. • Diagnosis with X-ray , IHAT in CSF. •Occasionally, a C.T scan may be ordered to rule out cerebral hematoma. culture media of CSF and PCR . Acanthamoeba culbertsoni Free-living trophozoites and cysts occur in both the soil and freshwater. Trophozoites occur only as amoeboid forms Acanthamoeba culbertsoni • Free-living amoeba • Lives in water have been found in soil; sea water; sewage; swimming pools; contact lens equipment; medicinal pools; dental treatment units and air conditioning systems • Contact lens wearers can get keratitis (infection of the cornea) by using tap water for lens disinfection or by swimming when wearing lenses Acanthamoe ba Acanthamoeba _ Acanthamoeba are ubiquitous organisms in nature. _ Most species are free-living. _ Cysts are common and are very resistant to chlorine. _ Some are opportunists that can cause infections in human. _ Infections with these amoebae are more common in immunocompromised patients. _ Amoebae can be introduced through environmental exposures, including swimming while wearing contact lenses or using contaminated contact lens solutions. _ Acanthamoeba genus causes 3 clinical syndromes: 1 - granulomatous amebic encephalitis (GAE). 2 - Disseminated granulomatous amebic disease (eg, skin, sinus, and pulmonary infections). 3 - Amebic keratitis: a sight-threatening disease. Most cases occur in people who wear contact lenses. Acanthamoeba results in lesions of the skin, eye, brain, etc. The symptoms of GAE including : Alter mental status, headache ,fever, neck stiffness, seizures, focal neurological signs and coma leading to death keratitis : corneal inflammation and corneal perforation often followed by blindness. Laboratory Diagnosis of infections with free-living amoebae: • Keratitis: • Acanthamoeba trophozoites or cysts can be demonstrated with corneal scrapings or a biopsy sample via wet mount, stains, histopathologic examination. • Granulomatous amebic encephalitis: _ This condition is diagnosed via brain biopsy. (cyst and trophozoit) Flagellate protozoa. • These organisms have more than one flagellum. These flagella enable them to move. • Flagellates inhabit reproductive tract, alimentary canal, tissue sites, blood stream, lymph vessels and cerebrospinal canal. Flagellate Protozoa Intestinal & urogenital Blood Flagellate flagellates Trichomonas. Giardia Chilomastix Giardia lamblia Malabsorption syndrome (Giardiasis) Most common intestinal flagellate of humans Most common water-borne and food-borne disease. Children worldwide Giardia lamblia • Also known as G. intestinalis or G. duodenalis. • Diseases: Giardiasis, lambliasis, flagellate diarrhea, (malabsorbtion syndrome) • Geographic distribution: world wide, more prevalence in warm climates. • Habitat: Upper portions of small intestine. • Infective state: Cyst Reservoirs: Men, dogs, cats, wild animals Mechanisms of Transmission: fecal contamination Contamination routes: Oral • • • • Incubation period bout 2-3 weeks Resistant to chlorine. Filtration is necessary to eliminate contamination Consist of 2 stages: 1)trophozoite 2)cyst Morphology • G. lamblia has two morphological stages: the trophozoite and the cyst. • Trophozoite: pear shaped, with a broad anterior 10-12µm long and 5-7µm wide It is also relatively flattened, with a large sucking disk on the anterior ventral side, which serves as the parasite’s method of attachment to the mucosa of the host. The trophozoite also has two median bodies and four pairs of flagella (anterior, caudal, posterior and ventral) Cyst: • egg-shaped, and measures 814µm by 7-10µm • After encystation, each organelle duplicates, so each cyst contains four nuclei, four median bodies, eight pairs of flagella--although these organelles are not arraigned in any clear pattern. Upon excystation, each cyst produces two trophozoites. • The flagella and adhesive disk are lost as the cyst matures but median bodies and axoneme persist. Giardia Life Cycle Pathogenesis • The clinical features associated with Giardia infection range from total latency (ie, asymptomatic), to acute self-resolving diarrhea, to chronic syndromes associated with nutritional disorders, weight loss and failure to thrive. • The specific mechanisms of Giardia pathogenesis leading to diarrhea and intestinal malabsorption are not completely understood and no specific virulence factors have been identified. • Attachment of trophozoites to the brush border could produce a mechanical irritation or mucosal injury. • In addition, normal villus structure is affected in some patients. For example, villus atrophy and crypt cell hypertrophy and an increase in crypt depth have been observed to varying degrees.. • Giardia infection can also lead to lactase deficiency as well as other enzyme deficiencies in the microvilli. • This reduced digestion and absorption of solutes may lead to an osmotic diarrhea. • asymptomatic group : • Well-nourished children with adequate immune response and adults who harborfew parasites and / or less virulent . symptomatic group : Generally children under six months, with some degree of malnutrition or poorimmune response. Characterized by the large number of parasites present. Clinical signs The clinical features associated with Giardiasis watery foul-smelling diarrhea, abdominal cramps, flatulence, anorexia, and nausea. are additional frequent complaints during chronic infections. In the majority of chronic cases the parasites and symptoms spontaneously disappear. Also have fat-soluble deficiencies, folic acid deficiencies, and structural changes in intestinal villi. Children exhibit clinical symptoms more frequently that adults Diagnosis Stool Examination: Stool examination is the preferred method for Giardia diagnosis. Diagnosis is confirmed by finding cysts or trophozoites in feces. Serology /ELISA to detect IgM in serum provides evidences of current infection Examination of duodenal fluid or duodenal biopsy:To identify Giardia lamblia and other enteric pathogens. To visualize changes in histologic features. Factors that promote infection • Poor quality of the means of disposal of garbage and excreta. Swarm of flies. • Fecal contamination of drinking water and irrigation. • Poor health education of the population. • Artificial feeding of infants (carelessness in the preparation of bottles). • (homosexual). • The cyst is viable for two months in cold water and is resistant to water. • Sometimes this infection is a family, and parents with symptomatic children infected but asymptomatic . Chilomastix mesnili – Non-pathogenic; endocommensal. – Trophs and cysts in the life cycle. – The cyst stage is resistant to environmental pressures and is responsible for transmission of Chilomastix – Cysts and trophozoites can be found in the feces (diagnostic stages). – Worldwide. – Habitat : the cecum. – Water borne parasite infected by contaminated water. C. mesnili • Even though they are not pathogenic and endocommensal, their presence indicates poor hygiene practices and sanitation. • Because of this need to be able to distinguish these from pathogenic organisms. Chilomastix mesnili • TROPHOZOITE - 6-24 µm long by 3-20 µm wide. • 4 flagella arise from kinetosomes at anterior end; 3 flagella extend anteriorly, 1 extends into the cytostome (flagella are difficult to see in stained trophozoites). Chilomastix mesnili • CYST is lemon-shaped; 6 to 10 µm in diameter. • Contains single nucleus, cytosome, and retracted flagella. Non-Pathogenic Intestinal Flagellates Chilomastix mesnili Life cycle of Chilomastix mesnili Infection occurs by the ingestion of cysts in contaminated water, food, . In the large (and possibly small) intestine, excystation releases trophozoites. Chilomastix resides in the cecum and/or colon; considered a commensal organism Laboratory diagnosis Pathogenicity: none (if present with large numbers, may be result in some disturbance). Microscopic examination: Stool examination for trophozoites or cysts