Parasitology
Faculty: AGUAZIM SAMUEL M.D.
Lange chapter 51
1
Intestinal and Urogenital
Protozoa
2
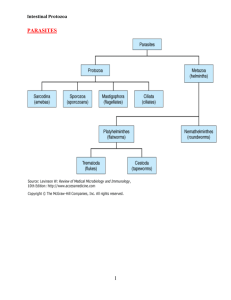
Parasites occur in two distinct forms:
• Single-cell called protozoa
• Multicellular metazoa called helminths
or worms.
3
Protozoa can be subdivided into four
groups:
•
•
•
•
Sarcodina (amebas),
Sporozoa (sporozoans),
Mastigophora (flagellates),
Ciliata (ciliates)
4
Metazoa are subdivided into two phyla:
•Platyhelminthes
(flatworms)
•Nemathelminthes(roundworms,
nematodes).
•Platyhelminthes
contains two medically
important classes:
•Cestoda
(tapeworms) (swimming in a cespool
of tapeworms)
•Trematoda
(flukes). (It is a fluke that you won a
million dollars and you are trembling with
5
excitement)
Intestinal Protozoa
•
Within the intestinal tract, three organisms:
- The ameba (Entamoeba histolytica)
- The flagellate (Giardia lamblia)
- The sporozoan (Cryptosporidium parvum)
6
Urogenital Protozoa
•
In the urogenital tract, one organism:
- The flagellate (Trichomonas vaginalis).
7
8
CASE
• 33 year old man, presenting with right
upper quadrant pain and fever of 4 days
duration; slight yellowing of skin.
• 1 week before, he had bloody stools,
about 3 or 4 times per day, but it resolved
9
Case: 5 cm hypoechoic liver
mass
10
CASE
• Metronidazole
• Significant improvement after 7 days
• Repeat UTZ: smaller mass
11
CASE
• Impression: Amebic liver abscess,
secondary to Entamoeba histolytica
12
Intestinal Protozoa
Entamoeba histolytica
• Diseases:Amebic dysentery and liver
abscess.
13
Entamoeba histolytica
Characteristics: Intestinal protozoan. The life
cycle consists of two stages:
(1) Motile ameba (trophozoite) consists of
one ingested red blood cell and one nucleus
(2) Non-motile cysts with four nuclei with no
internal fiber.
14
Trophozoite: one ingested red blood cell and one nucleus
15
Cysts: four nuclei with no internal fiber
16
Entamoeba histolytica trophozoites in section of intestine (H&E)
17
Entamoeba histolytica cyst and trophozoite, haematoxylin stained
18
Entamoeba histolytica
• Life cycle: Humans ingest cysts, which form excystation in
small intestine, which form trophozoites. Trophozoites pass to
the colon and multiply. Cyst form in the colon.
• Transmission and Epidemiology: Fecal-oral transmission of
cysts via water, fresh fruit and vegetables. Human reservoir.
Occurs worldwide, especially in tropics.
• Also: ano-genital or oro-anal sexual contact
•
Pathogenesis:
Trophozoites invade colon epithelium and produce “teardrop”
ulcer. Can spread to liver and lungs and cause abscess.
Excystation: the action of an encysted organism in escaping from its19
envelope
Life cycle of Entamoeba histolytica
20
Histopathology of a typical flask-shaped ulcer of intestinal amebiasis. CDC
21
Amebic dysentery
Acute amebiasis
frequent dysenteric stools of pus and
blood ; without feces
systemic toxicity: fever, dehydration,
electrolyte abnormalities
Tenesmus , abdominal tenderness
Chronic amebiasis
recurrent episodes of dysentery
intervening GIT disturbances, constipation
Invasive disease: liver, lung and brain
22
23
24
AMEBOMA
• proliferative
granulomatous
response at an ulcer
site
• infectious
pseudotumor
25
Ameboma
leading point of an
intussusception
or may cause intestinal
obstruction
26
Amebic liver abscess
• Most common extraintestinal form
• metastasis from intestinal infection
• Symptomatic intestinal infection need not be
present
• right upper quadrant pain
• right shoulder pain
• presses on the common bile duct : jaundice
• Lung atelectasis, consolidation, pleural effusion
27
28
Gross pathology of liver containing amebic abscessGross. CDC
29
RUPTURED AMEBIC LIVER ABSCESS WITH
“ANCHOVY PASTE”
Gross pathology of amebic abscess of liver. Tube of "chocolate" pus from
abscess.
CDC
30
Amebiasis cutis
31
Brain abscess
32
Entamoeba histolytica
Laboratory Diagnosis:
1. Trophozoites or cysts visible in stool.
2. Serologic testing (indirect hemagglutination test
positive with invasive disease).
Treatment:
- Metronidazole plus iodoquinol.
GET BAC on the Metro (Giardia, Entamoeba, Trichomonas,
Bacterial vaginitis, amoebic infection, C. difficile)
Prevention:
1- Proper disposal of human waste.
2- Water purification.
3- Hand washing.
33
Giardia lamblia
Most prevalence enteric parasite in the us
Leading in infectious agent in water borne
outbreaking diarrhea
Disease: Giardiasis, especially diarrhea
-Characteristics: Intestinal protozoan.
The life cycle consists of two stages:
(1) Trophozoite, Pear-shaped with two nuclei and four pairs of
flagella.
(2) The oval cyst with four nuclei and several internal fibers34.
35
Trophozoite: Pear-shaped with two nuclei and four pairs of flagella
Oval cyst: four nuclei and several internal fibers.
36
Giardiasis
Early symptoms:
flatulence
abdominal distension
nausea
foul-smelling bulky, often watery, diarrhea
explosive!!!
chronic stage
vitamin B12 malabsorption
disaccharidase deficiency
lactose intolerance
37
Diagnosis
Definitve tests:
Cysts in the stool
Trophozoites in the
duodenum
(Enterotest®)- string test
Endoscopy
Treatment
Metronidazole
4-6 hours
Bile-stained
38
39
Giardia lamblia
• Life cycle: Humans ingest cysts – form trophozoites in
duodenum which encyst and are passed in feces.
• Transmission and Epidemiology: Fecal-oral transmission of
cysts. Human and animal reservoir. Occurs worldwide.
• Pathogenesis: Trophozoites attach to wall with no invasion.
They interfere with absorption of fat and protein.
• Laboratory Diagnosis: Trophozoites or cysts visible in stool.
String test used if necessary.
• Treatment:
Quinacrine, with Metronidazole as an
acceptable alternative..
•
Prevention: Water purification. Handwashing.
40
41
42
Cryptosporidium parvum
• Disease: Cryptosporidiosis, especially
diarrhea.
• Characteristics: Intestinal protozoan.
• Life cycle: Oocysts release sporozoites; they
form trophozoites. After schizonts and
merozoites form, microgametes and
macrogametes are produced; they unite to
form a zygote and then an oocyst.
43
44
45
Cryptosporidium parvum
• Transmission and Epidemiology: Fecal-oral
transmission of cysts from undercook meat and
contaminated water. Human and animal reservoir.
Occurs worldwide.
• Pathogenesis: Trophozoites attach to wall of small
intestine but do not invade.
• Laboratory Diagnosis: (round) Oocysts visible in
stool with acid-fast stain.***
• Treatment and Prevention :
None.
46
47
CASE
• 23 year old female, with pain during sexual
contact, copious, malodorous vaginal
discharge of 3 days duration.
• Mild hypogastric pain, no vaginal bleeding
• Regular periods
• Multiple sexual partners, uses OCP
48
Case: Strawberry cervix, frothy
discharge,
49
Case: vaginal smear
50
Case: vaginal smear
• Impression: Trichomoniasis, secondary to
Trichomonas vaginalis
51
Urogenital Protozoa
Trichomonas vaginalis
• Disease: Trichomoniasis.
• Characteristics:
Urogenital protozoan. Pear-shaped,with a central
nucleus and four anterior flagella. It exists only as a
trophozoites. No cysts or other forms.
Mot : trophozoites, sexual, formites
• Laboratory Diagnosis: motile Trophozoites visible in
vaginal and prostate secretions.
• Clinical Finding: A watery, foul-smelling, yellowgreenish vaginal discharge accompanied by itching
52
and burning occurs.
53
Trophozoites: pear-shaped, a central nucleus and four flagella.
Trichomonas - Stained vaginal secretion
54
Trichomonas vaginalis
Trichomoniasis
55
Trichomoniasis
• Men: asymptomatic
OR
urethritis, prostatitis
• Women: asymptomatic
OR
mild to severe vaginitis
copious yellowish, frothy discharge
strawberry cervix “colpitis macularis”
56
Trichomoniasis
• Risk factors
– Infection with other STDs,
especially gonorrhea
– Four or more lifetime sex partners
– Sexual contact with an infected partner
– Not using barrier contraception
– Trading sex for money or drugs
57
T. vaginalis - Vaginal discharge
58
Trichomonas vaginalis
• Treatment: Metronidazole for both sexual
partners.
• Prevention: Condoms limit transmission
59
60
Isospora belli
ISOSPORIASIS
Transient diarrhea in healthy pts and
severe in IC
Forms and transmission
Fecal oral ingestion of oocysts.
Pathogenesis: The oocysts excyst in the
upper small intestine and invade the
mucosa, causing destruction of the
brush border.
Dx: ACID FAST & ELLIPTICAL
OOCYSTS
RX: TMP-SMX OR
PYRIMETHAMINE/SULFADIAZINE
Note: causes malabsoption similar to
giardia
61
CYCLOSPORA CAYETANENSIS
• MILD WATERY
DIARRHEA IN HEALTHY
AND SEVERE IN IC
• Member of
coccida(subtype of
sporozoa)
• TRANSMISSION: fecal
oral(via contaminated
water)
• Dx;spherical oocysts in
modified acid fast stain of a
stool sample
• Rx:trimethoprim
sulfamethoxazole.
62
MICROSPORIDIA
• Characterized by obligate
intracellular replication and
spore formation
• Persistent diarrhea in AIDS
pts(Enterocytozoon bieneusi
and Septata intestinalis)
• Tx: fecal oral
• Dx: spores in stool
• Rx: albendazole
• Others: no proven treatment
63
Balantidium coli
• only ciliated protozoan that
causes human disease, ie,
diarrhea.
• hosts: cows, pigs and horses
farm work, rural dwellers.
• MOT: ingestion of cysts
• similar to entamebiasis (extraintestinal
lesions do not occur)
• liver, lung and brain abscesses are not seen.
• Diagnosis is made by finding large ciliated
trophozoites or large cysts with a
characteristic V-shaped nucleus in the stool.
• The treatment of choice is tetracycline.
Prevention consists of avoiding
contamination of food and water by
64
Simply keep a place
within you where it is
welcomed, and happiness
will come and abide with
you forever.!!!!!!!!!!!!!
65

![[Type the document title] Kingdom: Phyla:](http://s2.studylib.net/store/data/012481522_1-94222f0fc30056e395d5b7a2bef31ebc-300x300.png)