Brazilian health system - People`s Health Movement
advertisement

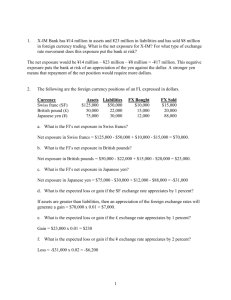
Brazilian health system Paulo M. Buss, MD, MPH Director, FIOCRUZ Center for Global Health Full Member, National Academy of Medicine Cape Town, PHA3, July 2012 1988 Constitution Since 1988, Brazil has been developing a dynamic, complex health system based on the principles of health as a citizen’s right and state’s duty. It strives to provide comprehensive, universal, preventive and curative care through decentralized management and provision of health services and promotion of community participation at all levels Infant Mortality and Income Ricos Pobres 2001-2 1991 0 20 40 60 80 100 Difference between richer and poorer quintiles Brazilian health system: complex network of complementary and competitive service providers and purchasers, forming a public–private mix Three subsectors: 1. Public subsector (SUS): services financed and provided by the state at the federal, state, and municipal levels 2. Private (for-profit and non-profit) subsector: services financed in various ways with public or private funds 3. Private health insurance subsector: different forms of health plans, varying insurance premiums and tax subsidies Public and private components distinct but interconnected Basic structure of the SUS • Three tiered system – Federal, 27 States, 5,562 Municipalities • Sharing in financing – Federal 58.0 % – States 24.7 % – Municipalities 17.3 % • Integrative Commissions at Federal and State level • Community involvement through health conferences and councils Financing • Taxes, social contributions, families and employers • 8,8% GDP in health (2009): – 43,6% public expenditure UK (82%), Italy (77,2%), Spain (71,8%), USA (45,5%), Mexico (46,9%) Primary Health Care (PHC) [Family Health Strategy] was the cornerstone to build an universal, accessible, integral, comprehensive and equitable Brazilian National Health System National Primary Health Care Policy Since March, 2006 PHC: group of health interventions, both at individual and collective levels, that include health promotion and protection, disease prevention, diagnosis, treatment, rehabilitation and health support Actions developed through a multidisciplinary work team, in a geographically defined territory and its correspondent population PHC: preferential and first contact point in the health system Principles: Universality, accessibility, coordination, vinculation, integration, responsibility, comprehensiveness, humanization, equity and social participation. Family Health Team At least: a physician, a nurse, a nurse assistant and 4 to 6 community health agents Most of the places include dental and social work professionals All of them work full time (40 hours per week) *** Salary is equal to having two or three different jobs for a physician Employment contracts under responsibility of municipalities Source:José Noronha, Icict/Fiocruz Family Health Team Community Health Agents To live in the same area where they work 240 thousands workers Must know their community’s problems To be able to facilitate and improve connections between primary care professionals and the community (cultural competency) They are one of the core members of the Brazilian primary health care strategy As a general health care professional focus on illnesses but also health promotion and prevention plus intersectoral connections Family Health Strategy Evolution of the coverage of Family Health Teams BRASIL, 1998/2010 1998 2002 2000 2006 0% 1 a 25% 2011 25 a 50% 50 a 75% 75 a 100% Family health teams: Evolution 1994-2011 Coverage of population (1994-2011) FHP figures (2012) 32,080 teams 5,284 municipalities Coverture: 52% Brazilian population; 98 million people Oral health teams: 21,038; 4,850 municipalities Communitarian agents: 240 thousands Expenditures: around USD 35 per person covered per year; no drugs included SUCESS, INSUCESS, CHALLENGES The expansion of the Family Health Strategy has improved the access to integral and permanent care, creating a platform for the prevention and management of the non-communicable diseases . For each 10% coverture raises, 4.5% of infant mortality falling. + Vulneráveis Média – Vulneráveis Schilling CM et al. Health Policy and Planning 2011 (no prelo) The National Immunisation Programme set up in 1973 stands out as one of Brazil’s most successful public health programmes, as reflected in its high vaccination coverage and sustainability, the latter guaranteed in part by the National Self-Sufficiency Programme in Immunobiologicals There have been no cases of poliomyelitis in Brazil since 1989, nor measles since 2000 Immunization • Between 1980 and 2007 the number of deaths due to tetanus falls 81% and for coqueluche 95% • In2007, no deaths due to diphtheria, poliomyelitis or measles • The incidence and lethality due to meningitis caused by HiB in children under 5 reduced dramatically after the introduction of HiB vaccine into de Brazilian vaccination program in 1999 Family Health and Family Subsidies Intersectoral action Bolsa Família Brazilian Cash Transfer Programme 7 years of evolution Reducing extreme poverty Reducing inequalities in wealth distribution Very important complement to the universal health system Better access to food and other fundamental goods Health condicionalities Dynamic intern market http://www.mds.gov.br/bolsafamilia/mural/es pecial-bolsa-familia-7-anos-1 Social participation SUS built during the re-democratization process and was its central political and ideological component (Health is democracy and democracy is health) Nest of SUS: VIII National Conference of Health (around 5,000 participants from all levels; social movements – academic sector – politicians – managers – private sector) National, ‘provincial’ and municipal (local) Councils of Health Fragmentation of the social movement: ‘Social’ councils vs. ‘health’ or other sectorial councils? No connections (competition) among councils Final remarks • The main strategy for improving healthcare should be through the strengthening of health system and services provided in an integrated manner • Healthcare systems should be strongly anchored on a sound primary care strategy • Healthcare networks, with well-defined lines of care and appropriate disease management protocols are essential to good healthcare delivery • Disease specific programmes can only succeed when supported by healthy healthcare systems • Targeted programmes should be directed to specific populations rather than to specific diseases • For good health outcomes it is crucial articulate health to other social policies