Aiming for Excellence Expert Advisory Group
advertisement
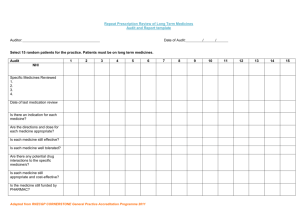
Aiming for Excellence RNZCGP Standard for NZ General Practice 2011 Dr Chris Fawcett Maureen Gillon Waveney Grennell Aiming for Excellence – what is it & who uses it? • RNZCGP Standard for NZ General Practice • Reinforces the unique character & contribution of general practice • Makes the values of general practice explicit • Provides a guide to building a platform to manage increasing diversity and complexity to facilitate a patients journey • Is the standard used by 800 practices in the CORNERSTONE programme • Increasingly used by other sector organisations as a benchmark Review of Aiming for Excellence RNZCGP Governance - RNZCGP Council RNZCGP Board RNZCGP Professional Practice Expert Advisory Group Aiming for Excellence Expert Advisory Group Sector interest • • • • • • • • • • • • • • • • General practices RNZCGP Programmes; CORNERSTONE, Education, MOPS CORNERSTONE Assessors NZ College of Practice Nurses NZNO PMAANZ – practice managers Wellington School of Medicine – clinical effectiveness work General Practice Networks Consumer/communities Health & Disability Commissioner PHOs DHBs NGO/Community sector, Te Wana MOH Health Quality & Safety Commission Health IT Board ACC The Development Team: Aiming for Excellence Expert Advisory Group • • • • • • • • • • • • • • • • • • Dr Chris Fawcett (Chair, CORNERSTONE Chief Censor) Dr Jane Burrell (Chair, Professional Practice Expert Advisory Group) Dr Tane Taylor (GP, Te Akoranga a Maui, CORNERSTONE Assessor) Dr Jim Vause (GP Te Akoranga a Maui, GP Assessor) Dr Jocelyn Tracey (GP, PHO Performance Programme) Dr Malcolm Dyer (GP, PHO Performance Programme) Dr Jane O’Hallahan (RNZCGP Group Manager Professional Practice) Dr Keri Ratima (GP, RNZCGP Tumauaki Maori Principal Advisor) Helen Bichan (Service User) Jane Ayling (CORNERSTONE Assessor, Practice Nurse, NZNO) Rosemary Gordon (CORNERSTONE Assessor, ProCare Quality Manager) Hayley Lord (Quality Manager, Midlands Health Network) Luis Villa (Advisor, Midlands Health Network) Kevin Rowlatt (Practice Manager) Waveney Grennell (RNZCGP CORNERSTONE Manager) Jeanette McKeogh (RNZCGP Senior Policy Advisor, legal) Madhukar Mel Pande (Advisor, Research) Helen Glasgow (RNZCGP CORNERSTONE QI Coordinator) • • • • Dr Roshan Perera (Academic Advisor) Dr John Wellingham (Peer reviewer) Stella McFarlane (Peer reviewer) Maureen Gillon (Project Lead) Method • • • • • • • • • • • • First consultation phase – 6mths Review of quality landscape & literature Feedback from CORNERSTONE practices & assessors on 2009 version Legal, safety and risk criteria updated Other criteria reviewed A4E working group – rebuild Testing for SMART – specific, measurable, achievable, relevant, timely: – Notified general practices, networks and sector organisations – Consumer workshops – Practice visits – Sector workshops – Targeted organisations Second consultation phase Refinement by A4E Working Group Peer review A4E Expert Advisory Group Handover & recommendation Signoff by College Board & Council Result of feedback on previous version Improved relevance and acceptability: – Legal safety & risk measurements were revised and updated – Duplication stripped out – Reduced number of indicators and criteria – Clarity was improved – More emphasis on the patient journey – integration, continuity, transfer of care – Emphasis on results – Greater emphasis on clinical effectiveness – Standards ratified by College A new structure was developed to reflect current thinking by the College 4 areas: – Patient experience – Practice Environment & Safety – Clinical Effectiveness Processes – Professional Development Purpose: – Focus on improving outcomes for patients Improving outcomes for patients Improved understanding about the intent of criteria – Needed to improve specificity of each criterion – Removal of the guide to interpretation to improve understanding and enable the CORNERSTONE programme to provide better advice to practices – Introduction of a rationale Indicator 16 The practice ensures effective infection control to protect the safety of patients and team members Criteria 16.1 Rationale The practice can demonstrate that its infection control policies and procedures align with the AS/NZS 4815: 2006 Standard Effective infection control measures protect the health and safety of people using and working in the practice, and implementing them is a prudent risk management activity A focus on supporting the patient journey Supported by the findings from the Voyage to Quality work – R. Perera, more emphasis on: • • • • • Clinical effectiveness Systems to manage patient care Robust information Transfer of care Continuity • Integration Next steps: Enabling clinical effectiveness • • • • • • • • • • • A General practice Quality System RNZCGP Quality Framework New three year structure incorporating clinical effectiveness requirements for CORNERSTONE Clinical Effectiveness Modules A CORNERSTONE resource library – practice access to modules Clinical outcome indicators The Healthcare Quality Measures NZ – library of indicators (Patients First) – practice access to clinical measures Clinical management tools – PHOs Patient self management Feedback loops – results Publish the Profile of CORNERSTONE General Practices 20092011 Principles Self directed PDSA cycle Based on quality framework Team process Years 2 and 3 Peer mediated Variety of modules and measures • National, local or individual practices Example Notes Area of interest Define the area of interest in broad terms initially. Prescribing analgesics Goal of activity What do you hope to achieve? Start with broad objectives and refine as required. The scope needs to be clear, sometimes working through the module development the scope will need to become more focussed but sometimes it may need to become broader. To ensure safe repeat prescribing of analgesics. Scope of activity All processes for repeat prescriptions of analgesics. Note: This could be widened to all prescribing (including first time prescriptions) or narrowed to repeat prescribing in the absence of a face to face consultation. Practice Environment Description of current situation. In what setting does this currently occur? Notes: Have you identified all possible settings? Patients ring for scripts from the nurse What is the system(s)? Scripts written at request of nurse. Perceived problems or questions about the current situation Not all patients have phones. Scripts needed very quickly – i.e. same day Receptionists take the notes. Potential solutions No checking of time since last prescribed, change of dose, other providers prescribing or interactions. Potential for abuse of drugs, escalating doses and short times between scripts. Protocol for the checking of scripts e.g. last time seen, last time prescribed, any visits to pain clinic, Oncology etc every time a script is requested by the nurse There is a mix of prescribing, both generic and by brand. The nurses don’t always understand the drugs. Education session about the drugs names and prescribing by the PHO pharmacist Practice Environment Notes: Identify all systems in all settings. Systems may be informal or formal – focus on what actually happens not what is meant to happen. What are the Nurse needs to competencies know drug names required? and details. Notes: Align with the problem definition and ensure competencies of all All requests to be left on a prescription phone line (answer phone) with a clear message that patients need to leave their details and the scripts will be available in one working day. Chosen solutions What are the organisation and practice supporting systems? Notes: Consider both formal and informal systems, i.e. what really happens? What are the IT systems? Notes: Consider the IT system in the practice but also systems in other organisations such as pharmacies, PHO, manual systems and gaps. Are their problems with practitioner knowledge? Notes: Ensure knowledge of all relevant practitioners is covered. What are the current educational activities which can provide input e.g. RNZCGP faculty, BMJ learning etc.? What are the important relationships within the practice? Notes: Consider There is online MIMS and a pharmacy website The information is not presented in a user friendly manner and it is difficult to identify the critical information. Identify a resource online for quick access by all clinical staff or develop one with the PHO pharmacist Scripts are written by hand in triplicate and also have to written into the paper notes Double handling and the risk of having a discrepancy between the hand written script and the computer records No clear solution – but lobby the MOH to change for computer generated scripts. Doctor has to understand the pain ladder and how to use the drugs appropriately. There has to be coordination between the doctors about the approach to pain. The doctors have a poor understanding of the pharmacology of the drugs, their interactions and the pain ladder. Each patient has a pain management plan clearly identified in the notes. Training from the PHO pharmacist about the pain ladder and analgesic use. Education from the Hospice service. Education from the Pain Clinic The nurses and doctors have to have a common approach to repeat prescribing The scripts are often presented to the doctor at the end of the day and create frustration and tension in the Dedicate specific time i.e. block out an appointment for the doctor and nurse to review request for Relationships What are the important relationships within other providers? Notes: Consider formal and informal relationships and what actually happens. What are the important relationships with patients? Notes: Consider formal and informal relationships and what actually Are there other important community relationships? Notes: Consider formal and informal relationships and what actually The pharmacists need to have a clear understanding of the processes by which these drugs are prescribed and have a clear understanding of their role in communicating with the doctors about problems e.g. drug interactions, excess prescribing Patients and doctors must have a common understanding about how the prescriptions will be written , how long it will take and how often they need to be seen At times patients may need the pain clinic, drug and alcohol services or even the police. Lack of communication Invite pharmacist to be involved in reporting back problems with prescribing in a manner which is effective for the practice, the pharmacy and the patient. Patients expect to get the medications at short notice and not to have to attend for review. Communicate with the patients via a targeted newsletter and via the answerphone message about the process of getting repeat scripts Patients may abuse the drugs, be involved in drug seeking or need more specialised input into their pain management Meet with the pain clinic team about their services. Meet with the alcohol and drug team. If appropriate liaise about general issues with the community constable. Measuring change Notes: Measuring change is important, but measures must be focussed on information that is useful to the practice and is easy to collect as part of day to day activity. Measuring When will measure it? Baseline measures Notes: What do we know about the problem, both qualitative and quantitative information? How big is this problem? What information do we need to gather before we start? What will we monitor to determine if our changes have been effective? Notes: What can we measure as we go so that data analysis can be facilitated? What do we already know about this problem Now All patients have a clear pain management plan. 6 months When will we review this? Query build and check all patients have a Pain Management Plan Critical events Are there critical events to monitor? Notes: Do we have a significant events monitoring system in place for this particular problem. Are we currently using this? Does it need to be improved? Prescriptions not picked up. Patients not being reviewed. 6 months Pharmacist to notify of uncollected scripts every month. Query build to check all patients reviewed. Measuring user evaluation Notes: Do we have baseline measures about this? Do we need more information before we proceed? How can we find out what the patients think about this? What are the timeframes for measuring? How patients perceive 6 months the service Target short five point patient questionnaire about the service. What is the cost? Notes: Do we have baseline measures about this? What information can we gather as we go? Are their issues of equity and how can they be addressed? Notes: Do we have baseline measures about this? What information can we gather as we go? Will this service cost 6 months money for the practice or the patient. Evaluate time spent in scripts and script charges. As most patients on long term medication are on a benefit we could add this to their disability benefit Query build to identify patients on long term medication and whether a disability benefit has been completed 6 months CORNERSTONE • Practices in the CORNERSTONE programme use Aiming for Excellence standards to develop their practice systems • Total number of general practices in NZ – 1086 • Registered with programme – 757 (70%) • Accredited Cycle 1 – 640 (59%) • Accredited Cycle 2 – 81 (62%) • PHO – 69 (prior to amalgamations) • DHB – 21 Next • Continue to accept feedback on Aiming for Excellence • Establish closer links with general practices to identify clinical effectiveness opportunities • Work with other general practice and primary care organisations to support patient improvement opportunities