File - Working Toward Zero HAIs
advertisement

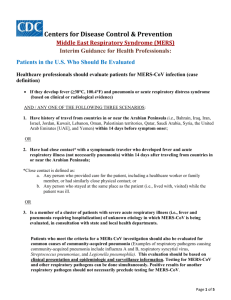
Unit Based Champions Infection Prevention eBug Bytes June 2013 Coronavirus:MERS-CoV • Globally, from September 2012 to date, WHO has been informed of a total of 53 laboratory-confirmed cases of infection with Middle East respiratory syndrome coronavirus (MERS-CoV), including 30 deaths. • WHO has received reports of laboratory-confirmed cases originating in the following countries in the Middle East to date: Jordan, Qatar, Saudi Arabia, and the United Arab Emirates (UAE). France, Germany, Italy, Tunisia and the United Kingdom also reported laboratory-confirmed cases; they were either transferred there for care of the disease or returned from the Middle East and subsequently became ill. In France, Italy, Tunisia and the United Kingdom, there has been limited local transmission among patients who had not been to the Middle East but had been in close contact with the laboratory-confirmed or probable cases. • Healthcare facilities are reminded of the importance of systematic implementation of infection prevention and control. Healthcare facilities that provide care for patients suspected or confirmed with MERS-CoV infection should take appropriate measures to decrease the risk of transmission of the virus to other patients, healthcare workers and visitors. MERS-CoV is Easily Transmitted in Healthcare • An investigative team of infectious disease experts who traveled to Saudi Arabia during an outbreak of the Middle East respiratory syndrome coronavirus (MERSCoV) reports that the virus poses a serious risk to hospitals because it is easily transmitted in healthcare settings. The team, from Johns Hopkins and elsewhere, investigated the spread of MERS-CoV in four local Saudi hospitals in May, and concluded that it is even more deadly than the related coronavirus responsible for the severe acute respiratory syndrome (SARS) outbreak in Toronto hospitals in 2003. The same team investigated that event, as well. Initially, 23 people in Saudi Arabia were infected with MERS at the time of the investigation, and 11 had died of the SARS-like virus. Saudi health officials now put the death toll at 32, with another 49 infected. • The experts, whose report on the outbreak is to be published in The New England Journal of Medicine online June 19, say that MERS is not only easily transmitted from patient to patient, but also from the transfer of sick patients to other hospitals. www.infectioncontroltoday.com Quebec hospital wants 1,000 patients to come in for HIV, hepatitis test due to equipment may not have been sterilized adequately • In mid-April hospital staff discovered a leak in one of its linear endoscopes, an instrument used to help diagnose cancer or gastroenterological malformations. Once tests were performed on the instrument, it was discovered hospital staff had not been properly disinfecting it for the past eight years. • During that period - from June 14, 2005, until May 1, 2013 - nearly 1,000 patients at Hôtel Dieu came into contact with that endoscope. The hospital has a record of each of those patients, and it is hoping that all will respond to an invitation to be tested for HIV as well as hepatitis B and C. • The hospital said it is launching an inquiry into how the problem occurred and who might have been responsible. • Hospital authorities said 70 percent of the affected patients are from the Quebec City area, and 30 percent are from other regions of the province • http://www.cbc.ca/news/canada/montreal/story/2013/06/03/quebec-levishotel-dieu-infection-risk-hiv-hepatitis-colonoscopy-endoscopy.html?autopla Multistate investigation of suspected infections following steroid injections • CDC is aware of reports of suspected infections among persons who received either 80mg/mL or 40mg/mL of preservative-free methylprednisolone acetate (MPA) produced by the Main Street Family Pharmacy in Newbern, Tennessee. As of June 3rd, CDC is aware of 24 reported cases from four states -Arkansas, Florida, Illinois, North Carolina. The majority of these persons developed skin and soft tissue infections of unclear etiology following intramuscular injection of this product. Additional clinical information is being gathered. • To date, no reports of meningitis or other life-threatening infections have been reported. All products labeled as sterile have been voluntarily recalled by the pharmacy. CDC is not aware of infections among persons who received products other than preservative-free MPA in the above formulation from this pharmacy. State and local health departments are working with CDC and FDA to evaluate this situation • www.cdc.gov/hai/outbreaks/TN-pharmacy/index.html Flu Vaccines Aimed at Younger Populations Could Break Annual Transmission Cycle • The key point: If you don't catch the flu, you can't die from it. • Centers for Disease Control and Prevention, researchers agree that almost everyone over the age of six months should get the flu vaccine, unless they were allergic to the shot or had other reasons not to take it. But in the US, only about one-third of the population actually gets a flu vaccine each year. Historic efforts have been focused on people at higher risk of death and severe disease -- often the elderly, and those with chronic illness, weakened immune systems, health care workers or others. With existing patterns of vaccine usage, the problem is enormous. Seasonal influenza in the U.S. results each year in an average of 36,000 deaths, more than 200,000 hospitalizations, an $87 billion economic burden, and millions of hours of lost time at school and work -- not to mention feeling sick and miserable. Vaccinating children could prevent a great deal of illness and save many lives at all ages. More aggressive educational campaigns to reach young adults would also be helpful. • Martial L. Ndeffo Mbah, Jan Medlock, Lauren Ancel Meyers, Alison P. Galvani, Jeffrey P. Townsend. Optimal targeting of seasonal influenza vaccination toward younger ages is robust to parameter uncertainty. Vaccine, 2013; DOI: 10.1016/j.vaccine.2013.04.052 NH report criticizes hospital in Hepatitis C outbreak • Exeter Hospital ignored employee concerns about a medical technician accused of infecting patients with hepatitis C, had an unreliable system for documenting their complaints and told at least one not to file a report. Kwiatkowski, a former medical technician who has been jailed since his arrest in July 2012, is accused of stealing painkiller syringes from the hospital's cardiac catheterization lab and replacing them with saline tainted with his blood. He has pleaded not guilty to 14 federal drug charges and is scheduled to go to trial in January. • Thirty-two Exeter Hospital patients have been diagnosed with the strain of hepatitis C that Kwiatkowski carries, along with an additional person who contracted the liver-destroying disease from one of them. In other states where Kwiatkowski worked, there have been seven confirmed cases in Maryland, six in Kansas and one in Pennsylvania. As outlined in earlier court documents, Kwiatkowski's co-workers raised concerns that he sometimes showed up for work with blood-shot eyes, was seen sweating profusely and foaming at the mouth and sometimes slurred his speech. But the hospital did not follow its own policy and re-test him for drugs, the report states. Chemical in antibacterial soaps may harm nursing babies • A mother's prolonged use of antibacterial soaps containing the chemical triclocarban may harm nursing babies, according to a recent study from the University of Tennessee, Knoxville. The study, which was conducted on rats, showed that exposure to the compound may reduce the survival rates of babies. The results were presented in June month at the Endocrine Society's 95th Annual Meeting and Expo in San Francisco. • Triclocarban, a bactericide, is found primarily in antibacterial bar soaps. The researchers noted that they were not condemning the use of antibacterial soaps. During research, pregnant rats fed with triclocarban through food had similar blood concentrations compared to human blood concentrations after a 15-minute shower using antibacterial soap. • The study found that triclocarban did not affect the post-birth survival rate of baby rats exposed to the compound in the womb. But baby rats nursed by mothers that were exposed to the compound did not survive beyond the sixth day after birth. • http://www.sciencecodex.com/ut_study_chemical_in_antibacterial_soaps_may_harm_nursing_ba bies-114845 Loyola Fights Healthcare Acquired Infections with Xenex Loyola University Health System is the first academic medical center in Illinois to take disinfection to futuristic levels. Nicknamed “Ralph” by the housekeeping staff at Gottlieb Memorial Hospital and “little Joe” at Loyola University Medical Center, 3-foot upright cylindrical robots provide the finishing touches to room sanitation. A rotating telescopic head emits germicidal ultraviolet (UV) rays for 15 minutes in closed, unoccupied rooms to systematically kill germs. According to studies, the disinfection robots eliminate Clostridium difficile (C. diff) in less than 4 minutes and Methicillin-resistant Staphylococcus Aureus (MRSA) in less than 2 minutes. “The robots are used for further disinfection in the operating suites and patient rooms including isolation, burn and transplant,” says Alex Tomich, DNP, RN, CIC, manager of infection prevention and control at Loyola. “Loyola takes very seriously its responsibility to protect patients, visitors and our hospital staff from infections and we are early adopters of proven technology as well as best practices.” The hospital housekeeping staff cleans the rooms and then uses the robots for additional sterilization. The pulsed UV light destroys viruses, bacteria and bacterial spores without human contact or use of chemicals Occupationally Acquired Salmonella Infection in a Phlebotomist — Minnesota, January 2013 MMWR, June 28 , 2013 / 62(25);525-525 • On January 25, 2013, the Minnesota Department of Health (MDH) was notified of two clinical cases of Salmonella I 4,12:i:1,2 infection with isolates that had indistinguishable pulsed-field gel electrophoresis (PFGE) patterns. Illness onset dates were January 3 and January 9, 2013. Patients A and B were hospitalized at the same hospital during January 12– 15 for dehydration. Investigations indicated that these cases were part of a multistate outbreak associated with frozen mice purchased to feed snakes. On January 25, the MDH Public Health Laboratory isolated Salmonella I 4,12:i:1,2 with an indistinguishable PFGE pattern from a third Minnesota resident, patient C. Patient C denied contact with frozen feeder mice or snakes, but was employed as a phlebotomist at the hospital where the two infected patients were hospitalized. Protocol at the hospital requires that each phlebotomist use a hand-held sample tracking device to scan the identification band of each patient from whom blood is drawn. Accessing these records, the infection prevention specialist at the hospital found that patient C drew blood from patient A on January 13 and from patients A and B on January 14, which was 3 days before onset of patient C's symptoms on January 17. Patient C reported use of gloves while drawing blood. In the absence of specific evidence for any other risk factor for Salmonella I 4,12:i:1,2 infection and considering the temporal relationship between exposure and symptom onset, occupational person-to-person contact with patients A or B likely was the source of patient C's infection. Salmonella transmission from infected patients to health-care workers, although rare, has been reported .