Childhood Respiratory Infections
advertisement

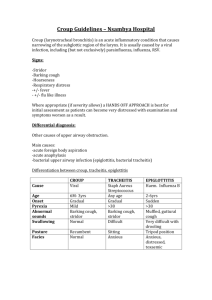
Dr. S. Benson GPSTI Infections URTI Croup Epiglottitis Whooping Cough Bronchiolitis Pneumonia TB URTI Coryza – Usually rhinovirus, coronavirus, RSV Pharyngitis – viral or Group A beta-haemolytic strep Tonsillitis – Group A beta-haemolytic strep and EBV Acute Otitis Media – viruses, pneumococcus, strep, haemophilus, moraxella catarrhalis Sinusitis – viral or bacterial URTI Children often present with: Sore throat Fever (inc febrile convulsions) Blocked Nose Nasal Discharge Earache Wheeze URTI Thorough examination is needed Exclude serious infections Address feeding and hydration Consider possible bacterial causes for: Otitis Media (discharge, ruptured drum, red and bulge) Tonsillitis (exudative with pus) Mainstay of treatment is paracetamol and ibuprofen URTI Antibiotics – to prescribe or not to prescribe? Recommend if tonsilitis or acute OM Tonsilitis – Give Penecillin V (avoid amoxicillin as maybe caused by EBV – rash) Acute OM – Coamoxiclav is a suitable choice Take throat swabs before treatment Most URTI are viral Croup Viral laryngotracheobronchitis Mucosal inflammation of respiratory tract Usually caused by RSV, parainfluenza and influenza Usually children are 6 months to 6 years old Presents as stridor and difficulty breathing Croup Can be managed at home if mild Give humidified air Give steroids (reduces severity and duration of croup) oral prednisolone (2mg/kg) for 3 days nebulised budesonide (2mg stat) Nebulised adrenaline provides transient relief If severe or desaturating will need admission Acute Epiglottitis Life threatening swelling of the epiglottis Can cause septicaemia Caused by haemophilus influenza type B Mostly in children 1-6yo DO NOT examine the throat Keep the child calm Acute Epiglottitis Management is in ITU ET intubation often required 7-10 days of 3rd gen cephalosporin Rifampicin prophylaxis for close contacts Croup vs Epiglottitis Croup Epiglottitis Time Course Days Hours Prodrome Coryza None Cough Barking None Feeding Can drink None Mouth Closed Drooling Toxic No Yes Fever <38.5 >38.5 Stridor Rasping Soft Voice Hoarse Weak / Silent Whooping Cough Caused by bordatella pertussis Three stages of illness Catarrhal (1-2 weeks) – fever, cough, coryza Paroxysmal (2-6 weeks) – barking cough Convalescent (2-4 weeks) – lesser symptoms which resolve The barking cough has a characteristic paroxysmal nature with an inspiratory whoop Whooping Cough Investigations: Eyes – Subconjunctival haemorrhages are indicated CXR FBC – Leucocytosis and lymphocytosis Nasal swab for pertussis As part of the work up, we need to ensure this is not pneumonia. Treatment is with erythromycin / clarythromycin These have limited effect on cough Whooping Cough Admission required if: Apnoeas Cyanosis Paroxysms Risk of seizures Patients should isolated for 5 days Immunize close contacts under the age of 7 Only 90% effective and wanes as child ages Prophylactic antibiotics to close contacts Bronchiolitis Most commonly due to RSV Also can be caused by influenza, parainfluenza, adenovirus, rhinovirus and C and M Pneumoniae Causes problems by: Invading nasal and pharyngeal epithelium Spreading to lower airways Increasing mucus production, desquamation and obstruction Net effect is hyperinflation and atelectasis Bronchiolitis History Winter months Coryzal illness Dry cough Worsening SOB Wheeze Feeding problems Apnoeic episodes Bronchiolitis Examination findings Cyanosis or pallor Dry cough Tachypnoea Subcostal and intercostal recession Chest hyperinflation Prolonged expiration Respiratory pauses Wheeze Crackles Bronchiolitis Treatment mainly supportive Keep oxygen saturations above 92% If tachypnoeic when feeding consider NG tube Bronchodilators (salbutamol, atrovent, adrenaline) Mechanical ventilation if severe Reserve antivirals for immunodeficient patients Prophylaxis is available for preterm or babies with chronic lung problems Pneumonia Lower respiratory tract infection Mostly bacterial Common pathogens shown below Age Pathogen Neonate Group B strep E. Coli Klebsiella Listeria Infants Strep pneumoniae Chlamydia School age Strep pneumoniae Staph aureus Group A strep Bordatella Mycoplasma pneumoniae Pneumonia Symptoms and Signs High temp Productive cough Tachypnoea (>50) Grunting Recession Cyanosis Lethargy Focal signs / bronchial breathing Pneumonia Investigations NPA FBC Microbiology CXR (not of mild and uncomplicated) Pleural fluid if effusion may be indicated Pneumonia Follow local guidelines for treatment Recommended treatments are Amoxicillin Coamoxiclav Cefuroxime Antipyretics can also be helpful IV fluids Oxygen as required Physiotherapy is not all that helpful in children Tuberculosis Consider in at risk groups Mantoux test CXR Specialist referral Summary URTI Croup Epiglottitis Whooping Cough Bronchiolitis Pneumonia TB