The Coleman Model Intervention - Wisconsin Institute for Healthy
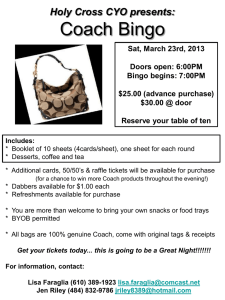
advertisement

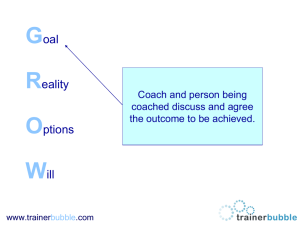
Care Transitions Intervention The Coleman Model Introduction • ADRC of Eau Claire County– 1st to implement this model in Wisconsin; evidence based model • Partner health care facilities: Mayo Clinic Health System, St. Joseph’s, Sacred Heart Hospital & Dove Healthcare • Collaborating with ADRC in Chippewa County to serve patients discharged to Chippewa County ---------------------------------------------------- • Lisa Riley, APSW – Certified Coach (1.0 FTE) • Miranda Hotter, CSW – Prevention Program Coordinator (.5 FTE)/Certified Coach (.5 FTE) • Emily Rogers, CSW- Certified Coach (.75 FTE) • Jennifer Owen, CSW – Supervisor Timeline • Hospitals worked to identify potential root cause(s) for readmission (Fall 2011) • Readmission data provided by Metastar (Fall 2011) • Coalition reviewed the data and intervention options • Identified the Care Transitions Intervention, Coleman Model, as the starting point • ADRCs in Eau Claire and Chippewa Counties are funding the project in 2012 • Began the intervention in February 2012 with Mayo Clinic Health System in Eau Claire • April 2012- expanded to Sacred Heart Hospital in Eau Claire • May 2012- expanding to St. Joseph’s Hospital and patients discharge to Chippewa County The Issue • When patients are inadequately prepared for the next setting (hospital to home) they or their caregivers act as default care coordinators • This can lead to med errors, postponed care, and re-hospitalization (which is defined as re-entering within 30 days, regardless of diagnoses or cause) • This re-hospitalization is costly in terms of quality of life for patients, and is financially costly for hospitals and usage of Medicare dollars • Hospitals will have financial repercussions from high rehospitalization rates The Goal “The transition coach’s role is based on teaching the skills, knowledge, and attitude necessary to empower patients to manage their own care.” Eligibility Criteria • Patients at high risk of readmission as identified by the hospital via their risk screening tool • Discharges to Eau Claire County & Chippewa County • Medicare beneficiary • Living independently (not in CBRF or long term SNF) • Diagnoses: CHF, COPD, coronary artery disease, diabetes, stroke, spinal stenosis, hip fracture, peripheral vascular disease, cardiac arrhythmias, pulmonary embolism, DVT, & individuals with dementia that have an active/able caregiver • Exclusions: Those on hospice, managed care, primary AODA or primary psych. diagnosis • Note: If the patient goes to short term rehab, the intervention will continue when they leave from the nursing home and return home Coaching Coaching is… Coaching is not… T EAC H I N G PAT I E N TS TO F I S H R AT H E R T H A N GIVING THEM A FISH D I R EC T PAT I E N T C A R E OR LO N G T E R M C A S E M A N AG E M E NT The Four Pillars • 1. Medication Self-management • 2. Patient Health Record (PHR) • 3. Timely Follow up with primary and/or specialist physician • 4. Red Flags Program Structure 5 contacts, designed to be a “catch & release” intervention -30 days • 1 Hospital visit – introduction of the program to the patient and/or family, rapport building, providing PHR (Done when patient is medically stable, prior to time of discharge) • 1 Home visit – patient engages in med. reconciliation with verbal cues from coach, encouragement to schedule to f/u appt with doctor. Patient centered agenda and pace (Ideally done 24-72 hours after d/c) • 3 Follow up phone calls – follow up regarding patient’s appt. with physician, discuss any of the 4 pillars that weren’t covered in the home visit, address needs identified by patient and family (These calls are done incrementally over the remaining 30 days) 1. Medication Self-Management • The goal is that the patient is knowledgeable about his/her medications and has a management system • The management system has to be realistic and individual to the person • Coach is non judgmental and realistic, i.e. Whatever the patient was doing before the Coach arrives is what they will continue to do when the Coach leaves 2. Patient Health Record (PHR) • A record of the patients health conditions, in his or her own words • List of medications (dose, frequency, & reason) how they actually take it, not necessarily as prescribed • Space for the patient’s self-identified goal • Space for patient’s concerns & questions for follow up visit with their physician or other provider (RN/PT/Pharmacist) • Space for Red Flags It is essential that the patient fill this out or has a consistent person to do it. The Coach will not be there in the future update it. 3. Patient Follow up with Physician • Coach will encourage and remind patient to schedule a follow up with their primary physician once out of the hospital. Many patients do not realize that their physician may not be aware they were in the hospital • Coach can role play this with patient to build skills in effectively getting a quick appointment, i.e. “I was just in the hospital for my CHF and have some questions about my medication” may be more effective than simply “I need an appointment.” • This follow up appointment is when the physician will look at PHR & learn about a possible med error or concern 4. Red Flags • Patients will identify and write down the indications that their condition is worsening… i.e. “what were you feeling before you went to the hospital?” • Along with that – they will identify what their plan is when they experience these red flags Coaching role • Coaching is not a replacement of any other current provider • It does not attempt to replace discharge planners or home health nurses • Coaching is intended to supplement any other service that a patient receives and enhance the patients effectiveness in utilizing these services and communicating with other providers • Coaching requires flexibility and letting go of rigid agendas Transitioning from this… To this How we are we measuring success? • Re-hospitalization rates will be monitored (QIO) • Patient activation scale – self care competencies are measured by the coach at first contact and after the last phone contact (simple 10 questions). Any positive movement is considered a success. • Follow up survey at 30, 60, 90, 180 days after intervention Note: It is to be expected that some patients will not progress in their skills, it requires a willingness to be empowered What we have seen so far… In the first 3 months of the program operating (February-May): • 140 referrals have been made to the program • 112 referrals accepted participation in the program (80%)- our goal is to have a 90%+ acceptance rate but this will take time • 39 have fully completed the program to date • Average increase in patient activation assessment score is 2 points • We are only aware of 2 readmissions that occurred within 30 days of completing the program; 0 readmissions within 60 days of completion • Medicare claims data will provide us with more concrete evidence, however, there is about a 3-6 month lag in data "My Transitions Coach® has helped me to feel more confident in managing my heart condition. I feel as though I am in charge of my health and I am less reliant on others.“ Contact info • ADRC of Eau Claire County 715.839.4735 • Lisa Riley 715.839.1870 lisa.riley@co.eau-claire.wi.us • Miranda Hotter 715.839.7998 miranda.hotter@co.eau-claire.wi.us • Emily Rogers 715.839.1272 emily.rogers@co.eau-claire.wi.us • Jennifer Owen 715.839.6713 jennifer.owen@co.eau-claire.wi.us www.caretransitions.org