Managed Care 101 - Health Alliance of Northern California
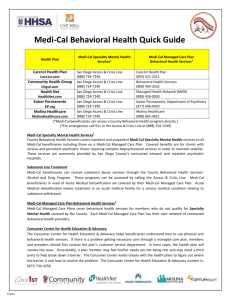
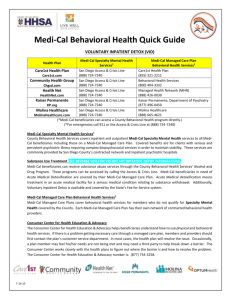
advertisement
Managed Care 101 Presented by Ralph Silber, CEO Community Health Center Network March 16, 2012 1 Fee-for Service In a FFS system, a health care provider receives an individual payment for each medical service delivered to a beneficiary. Beneficiaries generally may obtain services from any provider who has agreed to accept Medi-Cal payments. This model does not typically provide for the coordination of care for beneficiaries who have several medical providers. The FFS providers are reimbursed for each service after it is delivered. Managed Care Under this system, DHCS contracts with managed care plans, also known as health maintenance organizations, to provide health care coverage for Medi-Cal beneficiaries residing in certain counties. Managed care enrollees may obtain services from providers who accept payments from the health plan, also known as a plan’s “provider network”. The health plans are reimbursed on a “capitated” basis with a predetermined amount per person, per month regardless of the number of services an individual receives. Unlike FFS providers, the health plans assume financial risk, in that it may cost them more or less money than the capitated amount paid to them to deliver the necessary care. Medi-Cal Managed Care Medi-Cal Managed Care Beneficiaries Receive Coordinated Care. Managed care plans typically contract with health care providers, such as physicians and hospitals, to provide services to enrollees. Medi-Cal beneficiaries enrolled in a managed care plan select a primary care physician who provides their health care services on a regular basis. Managed care plans provide assistance to enrollees by coordinating care through referrals to specialist, telephone advice nurses, and customer care centers. Individual providers under managed care may be paid on a fee-forservice or capitation basis. Managed Care Definition: Health Maintenance Organization (HMO) AKA Managed Care Plan, Health Plan, Plan • Medi-Cal contracts with plans to provide defined set of covered benefits for a set per-member per-month amount. • The plans then contract with medical groups, hospitals, and other providers to provide a full range of health services for their enrollees. • Examples: Local initiatives, Health Net, Blue Cross, Molina 5 Managed Care Definition: Capitation or “per-member per-month” (PM PM) The fixed amount of money paid on a monthly basis to a health plan, an Independent Physician Association (IPA), or medical group for a defined set of medical services. 6 Medi-Cal Managed Care: • Medi-Cal beneficiaries are enrolled in managed care according to the model in their given county • Medi-Cal pays the managed care plan a set amount each month for each member (PM PM) • Beneficiaries select or are assigned a primary care physician who coordinates care 7 Medi-Cal Managed Care: • The state began enrolling large numbers of Medi-Cal beneficiaries in managed care in the 1990’s • Three main Medi-Cal managed care models in California: • County Organized Health Systems • Geographic managed Care • Two-Plan Model • Also limited number of special managed care projects (e.g., PACE) 8 County Organized Health Systems (COHS) A local agency created by a county board of supervisors to contract with the Medi-Cal program. • Enrolled recipients choose their health care provider from among all COHS providers. • COHS serves about 885,000 beneficiaries thru 6 health plans in 14 counties) • • • • • • CalOPTIMA (Orange) Central CA Alliance for Health (Merced, Monterey, Santa Cruz) Health Plan of San Mateo Partnership HealthPlan of California (PHC) (Marin, Mendocino, Napa, Solano, Sonoma, Yolo) CenCal Health (San Louis Obispo, Santa Barbara) Gold Coast health Plan (Ventura) 9 Geographic Managed Care (GMC) • Implemented to provide medical and dental care for Medi-Cal beneficiaries in San Diego and Sacramento Counties • The GMC model allows many plans to operate within a designated geographic region • GMC serves about 450,000 beneficiaries in the two counties 10 Two-Plan Model • In Two-Plan counties (with large Medi-Cal populations) MediCal contracts with two managed care plans. • One plan is commercial and the other plan is a locally organized “local initiative” sanctioned by the county’s board of supervisors. • Two-Plan serves about 3 million beneficiaries in 14 counties 11 12 Medi-Cal Eligibility Categories - Families with Children - Seniors & Persons of Disabilities (SPDs) – Medi-Cal only - Dual Eligibles (Medi-Cal & Medicare) - Pregnancy and Emergency Only Medi-Cal - Medi-Cal Share of Cost Carve Outs from Medi-Cal Managed Care Specialty Mental Health. CA Children’s Services (CCS) Long Term Care (?) How Does PPS Work Under Medi-Cal Managed Care FQHCs receive primary care payment from health plans based on “market rate” These payments may be fee-for-service or capitation Each FQHC gets a “wraparound” PPS rate (code18) from the state; estimate of difference between payment from the plan and PPS rate For each visit, an FQHC submits a “claim” to the plan and a code 18 claim to Medi-Cal Managed Care Reconciliation process Bonus payments outside of reconciliation Managed Care as A Solution Controls Costs Promotes Prevention Quality Focus 16 Managed Care – Solutions/Advantages Controlled Costs Reimbursement is fixed regardless of services offered - capitation At risk to lose money if costs are higher than expected Control costs by negotiating discounts Increased Access Management of costs creates greater access Build contracted specialty network-obligated to see patients Improve Quality Altering physician practice patterns Encourages coordination and integration of care – creating integrated health care delivery systems Members have access to protection by regulators 17 Care Management Populations Chronic conditions: asthma, diabetes, chronic renal failure, cardiovascular disease Severe or unusual medical conditions Frequent or inappropriate ER and Urgent Care Frequent or inappropriate hospitalizations Disabled with special needs Members with special needs homelessness, transportation, supplies, substance abuse, inability to understand or use managed care 18