Medicaid Managed Care: How, why, and keeping
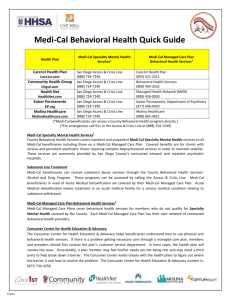
advertisement

Medicaid Managed Care: Keeping your clients connected to care in a changing environment Lessons, advice, and warnings from California Vanessa Cajina, Legislative Advocate Families USA, January 23, 2014 WESTERN CENTER ON LAW & POVERTY First things first: We made it! Happy January 2014! Okay, now down to business: Roadmap for today: California’s Medicaid program (Medi-Cal), and our historic managed care populations Other California laws and protections for health care consumers How our state managed to get pretty much all of our populations into managed care How we fought back, and continue to do so: tips, tricks, and flashpoints Resources and state laws and regulations A little background: Population-wise, the largest state in the nation: 38 million We’re officially a “majority-minority” state: 2/3s people of color & almost 40% Latino in 2012 43% of us speak a language other than English at home We have the highest poverty rate in the US - almost 25% Our state budget: Back in black We were the 1st to start an Exchange, & one of the 1st to enact the full Medicaid expansion Medi-Cal: At a glance US’ largest Medicaid program: about 7.6 million people Medi-Cal provides free, comprehensive coverage for: 1 in 5 Californians under age 65 1 in 3 of our kids Most people living with AIDS We also cover: Low-income parents People with disabilities Pregnant women Seniors about age 65 And we’re excited that we NOW cover childless adults from age 19 up to age 65! A brief history of Medi-Cal 1966 – California creates Medi-Cal following Title XIX of Social Security Act created Medicaid 1973 – first Medi-Cal managed care plans established 1982 – state creates 3 County Organized Health Systems (COHS). A COHS is the health plan for ALL Medi-Cal beneficiaries in that county; 3 more added in 1990 1992-96 – Additional managed care models adopted throughout California 1993 – State required most children and parents with MediCal to enroll in managed care 2011 – Feds ok’d move of Seniors and Persons with Disabilities & Duals into managed care, expansion into rural areas The pros & cons of managed care Managed care can be a good fit, particularly for people with lower health needs or those in good overall health However, it can be very hard to navigate for people with multiple providers, specialists, subspecialists, or those who use non-medical services like durable medical equipment, pharmacies, other long-term services These navigation problems are especially prevalent during transitions between traditional Medicaid to managed care And what do provider contracts look like? How are your medical groups regulated – how much risk do they bear and does that impact treatment decisions? Can the health plan guarantee that their networks are adequate for the population they serve, including specialist access, subspecialists, hospital contracts, etc… From the County of Los Angeles, with a total population of 9.9 million *About 2.39 million Angelenos will be Medi-Cal-eligible with the ACA expansion To Rural California For example, Mono County has a population of under 15,000 and a population density of 4 people per square mile California currently has 6 models of managed care delivery, with each of 58 counties choosing which model to employ – each with its own regulations and sets of operations California Protections Under CA law, most Medi-Cal managed care plans are treated like commercial managed care plans, meaning they have to follow certain laws in providing and helping patients access care Some of our tools include: Knox-Keene Act – the granddaddy of California health consumer protections Continuity of care Medical Exemption Requests Contract language, health plan oversight Knox Keene – CA Health & Safety Code § 1340-1399.818 The big law in California that regulates managed care plans, including most Medi-Cal plans Passed in 1975 with subsequent amendments, includes: Services covered Access standards Consumer protections Quality assurance Grievances & dispute resolution Financial protections & solvency for plans, contracts & licensure Knox Keene cont’d Since enacted, great provisions added on requiring plans to provide language assistance and interpretation to consumers Provides for Continuity of Care – we’ll discuss in a moment More information available at: http://www.healthconsumer.org/cs016knoxkeene.pdf http://www.leginfo.ca.gov/cgibin/calawquery?codesection=hsc&codebody=&hits=20 Medical Exemption Requests An existing policy within our Medi-Cal program The use of MERs was expanded when SPDs were required to enroll in managed care Permits a beneficiary to opt out of managed care if s/he has a relationship with a doctor/nurse midwife/licensed midwife who is not part of a health plan In California, this is a narrow document and the MER only lasts 12 months When new populations are added to mandatory managed care, MERs are typically added to legislative language Continuity of Care Beneficiaries have the right to completion of certain covered services they were getting from a nonparticipating or terminated provider, under some conditions Services for an acute condition, serious chronic condition, pregnancy, terminal illness, newborn care, and some planned surgeries must be provided for up to 12 months Medi-Cal enrollees newly enrolled in a plan can continue RX as long as RX was in effect when the beneficiary moved into the plan. An underused protection, and subject to a health plan negotiation with the non-participating provider Continuity of Care for special populations 1. SPDs: FFS to managed care -Additional RX authorizations if their MER was denied, plus other protections. -New enrollees can request to see FFS provider for up to 12 months – must have seen the provider in the last 12 months – provider must accept the higher of the plan’s rate or the Medi-Cal FFS rate. Plan must notify SPD within 30 days of request. 2. Duals: FFS to managed care -Duals in certain counties may request treatment with out-of-network providers for 6 months if they have seen provider twice in last 12 months. 3. Children shifting from CHIP to Medi-Cal: managed care to managed care -Kids going to a new health plan will get preference in keeping their PCP -If child’s PCP isn’t in new plan, the child may keep that provider for 12 months Administrative Advocacy Medi-Cal is administered by the state’s Department of Health Care Services, but participating plans are regulated by the Department of Managed Health Care Demand that contracts be public, as well as correspondence and directives from the plan’s regulator or contract manager including subregulatory guidance Establish relationships with health plans and provider organizations Is your state considering expanding managed care? Draft and advocate for model language if the transition is a foregone conclusion – even piecemeal fixes can help Start with gradual additions of types of beneficiaries – perhaps children & families, or adult expansion Medicaid population Your state has a D majority? Talk to labor – some home care unions have found that managed care could be better for their members Your state has an R majority? Pit health plans against providers and choose your friends and battles wisely For more information and model language: Western Center on Law and Poverty www.wclp.org – vcajina@wclp.org National Health Law Program www.healthlaw.org & http://www.healthlaw.org/issues/medicaid/managedcare/continuity-of-care-in-medi-cal#.UtcYWLRXL5M