Mitchell E. Daniels, Jr., Governor
State of Indiana
Indiana Family and Social Services Administration
2010 IHCP Annual Seminar
Indiana Care Select Program
Overview
Today’s Agenda
• October 1, 2010 Change in Scope
– Restructured Program Goals
– CMO’s, Member Eligibility & Opt-out Process
– Disease Management
– HP Continued Functions
– Disease Management
• Prior Authorization Process
• Certification Code Policy
• Right Choices Program Referral Process
• 2010 Care Select Quality Measures
• CMO Updates
• Q&A
2
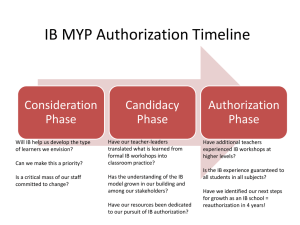
Indiana Care Select Program
Change in Scope
Restructured Program Goals
• Transition from a care management program to a disease
management program focusing on members with chronic
conditions
• Re-designed to help patients with chronic illnesses lead
healthier and more productive lives
• About 32,000 Medicaid members are eligible for the disease
management program
• Members no longer eligible for Care Select were sent a letter
in August 2010 informing them they are eligible for Traditional
Medicaid and that their benefits will remain the same.
3
Indiana Care Select Program
Change in Scope
• Care Select Care Management Organizations (CMO’s)
– ADVANTAGE Health Solutions, Inc.sm
– MDwise, Inc.
• Statewide Populations Served
– The aged, if not eligible for Medicare;
– Blind members;
– Physically and/or mentally disabled members (collectively known
as “the ABD population”);
– Wards of the court and foster children; or
– Children on adoption assistance
4
Indiana Care Select Program
Change in Scope
• Eligible Care Select Members (Conditions)
–
–
–
–
–
–
–
–
Asthma
Diabetes
Congestive Heart Failure
Coronary Heart Disease
Hypertension
Chronic Kidney Disease
Severe Mental Illness (SMI) and Depression
Serious Emotional Disturbance (SED)
5
Indiana Care Select Program
Change in Scope
• Statewide Populations not eligible for the Care Select
program
– Dual-eligible members
– The population on Home and Community Based Service (HCBS)
waivers
– MED Works participants
– Individuals receiving room and board assistance
– Breast and Cervical Cancer Group
– Individuals with QMB or SLMB only (not in combination with
another aid category)
6
Indiana Care Select Program
Change in Scope
Member Opt-out Process
• Members can opt-out if they are eligible to participate in
disease management programs that the Care Management
Organizations (CMOs) provide for their chronic conditions
• Members who opt-out will be enrolled in Traditional Medicaid
• HCBS waiver members will no longer be in Care Select and
continue to receive case management services through the
waiver
7
Care Select Member Opt-out
Process Overview
Member letter sent in
August
Member staying in Care
Select
Member no longer in
Care Select
Member new to Care
Select
Member
needs to do
nothing.
Can call
Maximus to
opt-out at
any time.
Call Maximus
Opt-Out
OR
8
Pick PMP &
CMO
Member needs to do
nothing; Moves back to
Traditional Medicaid
10-1-10
May call Maximus if
they have ?s.
Indiana Care Select Program
Change in Scope
Disease Management
• Members with a chronic condition will have access to
additional health education resources with the CMO
• Increased compliance with disease management treatment
plans including medication compliance and appropriate
preventative care visits
• Disease specific assessments and care plans
• Goals: individualized & preventative care
9
Indiana Care Select Program
Change in Scope
HP’s Continued Functions
• Process claims for all services provided to Care Select
Members
• Follow the IHCP Provider Manual
• The member must be eligible for Medicaid – check eligibility
prior to providing services
• Web InterChange administration & maintenance
• Remittance advices and claims adjudication
• Claims resolution
• IHCP Provider Enrollment
• PMP Quarterly Certification Code Distribution
10
Prior Authorization
• ADVANTAGE Health Solutions, Inc.sm
– www.advantageplan.com/advcareselect
– 1-800-784-3981 – Care Select PA
– 1-800-269-5720 – Traditional FFS & MRO PA
• ADVANTAGE was selected to function as the Traditional
Medicaid fee–for–service and MRO Transformation PA
administrator
• MDwise, Inc.
– www.mdwise.org
– 1-866-440-2449 – Care Select PA
Note: All PA’s for prescription drugs are processed
11
by ACS and not the CMOs
Prior Authorization
General Information
• The STATE plan requirements for Prior Authorization are the
same for both Indiana Care Select and Traditional Medicaid
(FFS)
• The CMO’s PA departments use OMPP approved criteria in
addition to the Indiana Administrative Code (IAC), PA
guidelines, and Indiana Health Coverage Programs (IHCP)
bulletins, banner pages, and newsletters when considering PA
requests
• The CMO’s PA Departments review all medical, facility, or
dental PA requests
12
Prior Authorization
General Information
• Decisions to authorize, modify, or deny a PA is based on
medical reasonableness, necessity, and other criteria outlined
in 405 IAC 5-3 and reflects the current standards of practice in
the provider community
• For a full detailed explanation of PA processes and
procedures, please refer to Chapter 6 of the IHCP Provider
Manual
• Out-of-state providers must obtain PA prior to performing
services (except emergencies & CMO contracted out-of-state
PMPs performing services that don’t require PA)
13
Prior Authorization
PA Helpful Tips
• All prior authorizations (PA) are submitted to the member’s health
plan on the date of request
• Fax the Indiana Prior Review and Authorization Request form along
with supporting documents
• Web InterChange allows providers to submit non-pharmacy PA
requests Note: Prior to contacting the CMO on PA status, providers
should verify PA status using web interChange first
• Mail – Written requests for PA are submitted using an Indiana Prior
Review and Authorization Request form along with supporting
documents
• View fee schedule at www.indianamedicaid.com to
see if a covered service requires 14PA
Prior Authorization
PA Helpful Tips (Cont.)
• New services require a new Prior Authorization request form
– Reminder: Providers may not add new services to an existing
PA request as this constitutes a new PA request
• Indiana Prior Review and Authorization Request Form, System
Update Form and Dental Prior Review and Authorization
Request Form
– These forms are available on the Forms page, under the
provider section of the IHCP Website at
www.indianamedicaid.com
– View PA form completion information in Chapter Six
of the IHCP Provider Manual at
www.indianamedicaid.com 15
Prior Authorization
PA Helpful Tips (Cont.)
• PA form information left open to interpretation
– Please submit legible forms if mailing or faxing
– Keep supporting documentation and PA request form
together
– If faxing, please consider volume and use direct mail as an
alternative (please do not batch faxes)
– Make sure PA request form is signed by appropriate
authorized provider
16
Prior Authorization
Web Interchange
• The following provider types can submit PA requests via Web interChange:
– Chiropractor
– Dentist
– Doctor of Medicine
– Doctor of Osteopathy
– Home Health Agency (authorized agent)
– Hospice
– Hospitals
– Optometrist
– Podiatrist
– Psychologist endorsed as a Health Service Practitioner in Psychology
(HSPP)
– Transportation providers
17
Prior Authorization
Top PA Suspension/Denied Reasons
•
•
•
•
•
•
Certificate of medical necessity missing/incomplete
Home health plan of care missing/incomplete
Incomplete PA form
Missing physician orders
Clinical documentation missing
Incorrect form submitted
18
Certification Code Policy
• The Care Select PMP is responsible for providing and/or
overseeing a member’s care during the time the member is
linked to that PMP through the PMP assignment process
• The PMP agrees to provide the necessary primary and
preventive health services directly to their assigned members
or agrees to refer the member to another health care provider
for those services undeliverable by the PMP
• Each Care Select PMP is assigned a cert code on a quarterly
basis
• This code, in addition to the PMP’s National Provider Identifier
(NPI) is needed to allow a specialist or another provider’s
claims to be paid when appropriate
19
Certification Code Policy
Policy Description Statements
• While it is always preferable that the assigned PMP authorize
treatment and provide their NPI and cert code, there may be
occasions when this is not possible
• Appropriate and designated CMO staff will need to provide
this information to another health care provider in order to
allow the Care Select member access to appropriate and
timely care
• The following are specific circumstances in which designated
CMO staff may release to another health care provider a
member’s PMP’s cert code and NPI before or after a service
has been rendered as approved by the State
20
Certification Code Policy
Exceptions
• PMP change is still pending after a member has selected a new
PMP
• Death of PMP
• PMP moves out of the region without proper notification to the
program
• Newly transitioned members into the program who are in need
of treatment (i.e. EPSDT) within the first sixty (60) days of
enrollment
• Member lives in an underserved area and is unable to select a
PMP from that area
• Other urgent, emergent, or ongoing issues (i.e. dialysis or
emergent ER admission) where the member is unable to access
necessary services and the assigned PMP is unwilling or
unable to provide services or the appropriate referral
21
Right Choices Program (RCP)
Referral Process
• ADVANTAGE Health Solutions identifies and monitors RCP
members in both ADVANTAGE Care Select and Traditional feefor-service Medicaid Programs
• MDwise Care Select identifies and monitors RCP members in
the MDwise Care Select Program
• RCP includes members who have shown a pattern of potential
mis-utilization or over-utilization of services (for example)
– Non-emergent use of the ER
– “drug seeking” behavior
– Resistance to PCP interventions
22
Right Choices Program (RCP)
Referral Process
The RCP is:
• Not a loss of benefits
• Not a reduction in benefits
• Not a punitive action, but is a legal action
Note: Members are still eligible for all medically necessary IHCP services.
However, those services must be ordered or authorized in writing by the
member’s assigned PMP
23
Right Choices Program (RCP)
Referral Process
• The RCP identifies members appropriate for assignment and
subsequent “lock-in” to:
– one Primary Medical Provider (PMP)
– one pharmacy and
– one hospital
• The goal of “lock-in” is to ensure members receive
appropriate care and prevent members from mis-utilizing
services
• Specialty providers receive written authorization from the
PMP
• The CMO’s add those specialists to the member’s provider list
in order for the specialty provider to be reimbursed
Note: The RCP Program applies to both members
in Traditional Medicaid and Indiana Care Select
24
Right Choices Program (RCP)
Referral Process
• The PMP manages the member’s care and determines
whether a member requires evaluation or treatment by a
specialty provider
– Referrals are required by the PMP for most specialty
medical providers (except self referral services)
– Referrals should be based on medical necessity and not
solely on the desire of the member to see a specialist
– Emergency services for life threatening or life altering
conditions are available at any hospital, but nonemergency services require a referral from the PMP
25
Right Choices Program (RCP)
Referral Process
Adding Providers to a Right Choices Member’s
Lock In List
• Additional providers may be locked-in, either short-term or on
an ongoing basis, if the PMP sends a written referral
• Providers may be locked-in for one specified date of service or
for any defined duration of time, up to one year
26
Right Choices Program (RCP)
Referral Process
Self Referral
• Behavioral health (except
prescriptions)
• Chiropractic services
• Dental services (except
prescriptions)
• Diabetes self-management
services
• Family planning services
• HIV/AIDS targeted case
management
• Home health care
• Hospice
• Podiatric services (except
prescriptions)
• Transportation
• Vision care (except surgery)
• Waiver services
27
Right Choices Program (RCP)
Referral Process
Referral Guidelines for the PMP
• Referrals must be faxed or mailed
• Referrals may be handwritten on letterhead or a prescription
pad, however, they must include the following information:
– IHCP member’s name
– IHCP member’s RID
– First and last name and specialty of the physician to whom
the member is being referred
– Primary lock-in physician’s signature (not that of a staff
member)
– Date and duration of referral
28
Right Choices Program (RCP)
Referral Process
Contact Information
ADVANTAGE
MDwise
ADVANTAGE Health Solutions –
Traditional FFS
Attn: Right Choices Program
P.O. Box 40789
Indianapolis, IN 46240
1-800-784-3981
Fax: 1-800-689-2759
MDwise Care Select
Attn: Care Management
P.O. Box 44214
Indianapolis, Indiana 46244-0214
Phone: 1-800-356-1204 or
317-630-2831
Fax: 1-877-822-7187 or
317-822-7517
ADVANTAGE Health Solutions Care Select
Attn: Right Choices Program
P.O. Box 40789
Indianapolis, IN 46240
1-800-784-3981
Fax: 1-800-689-2759
29
2010 Care Select Quality Measures
The office of Medicaid Policy and Planning (OMPP) requires the
CMOs to report their PMP’s performance in preventative
service delivery.
• Annual HEDIS recommended preventative services are based
on age and/or sex of the member
• Examples of preventative services that OMPP measures the
CMOs on include:
– Adolescent Well child Visits
– Cholesterol Screening
– Diabetes Screening
– ER Bounce Back
30
2010 Care Select Quality Measures
Step 4.
Submit claim to HP
Step 1.
Identify care gap
Step 3.
Provide service to
member
Step 2.
Notify member
31
CMO Updates
• State Mandated Preventative Services Guidelines will
be made available at www.mdwise.org and
www.advantageplan.com
• To date ADVANTAGE and MDwise have paid out a
total of approx. $400,000 in P4P programs paid to the
PMP community for providing high quality
preventative care
32
CMO
Contact Information
ADVANTAGE Care Select:
1-800-784-3981
MDwise Care Select:
1-800-356-1204
33
Q&A
Thank you for attending!
34