Nocturnal Blood Pressure Dipping, Acculturation, and the
advertisement

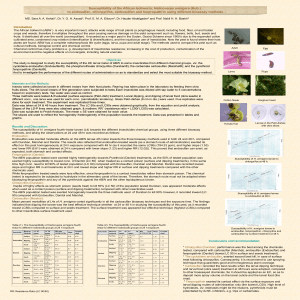
Nocturnal Blood Pressure Dipping, Acculturation, and the Metabolic Syndrome in Hispanic Women Smriti Shivpuri, M.S. Linda C. Gallo, Ph.D. San Diego State University/ University of California San Diego Joint Doctoral Program in Clinical Psychology Nocturnal Blood Pressure (NBP) Dipping NBP dipping defined as difference between diurnal and nocturnal levels of BP Typical NBP dipping in adults 10-20% Classification “Non-dippers” <10% “Dippers” >/= 10% “Extreme Dippers” >20% “Reverse Dippers” higher nocturnal BP NBP Dipping and Cardiovascular Disease (CVD) Outcomes Non-dipping linked to increased risk of a variety of CVD outcomes: Heart failure, Myocardial Infarction1 Stroke2 Sudden Death1 Target Organ damage3 Carotid IMT4 Left ventricular hypertrophy5 Mediating physiological mechanisms poorly understood Metabolic Syndrome (MetSyn) Syndrome characterized by constellation of risk factors of metabolic origin Defined by NCEP ATPIIIa as 3 of following (women): El eva te d B P A bdo m in al O b esity At h er o ge n ic Dysl ip id em ia In su li n Resist an ce aNational Syst o lic B P (S B P ) 130 OR D ia st o lic BP (D B P) 85 Wa ist Circ u m fere n ce > 88 cm (> 35 in ) HDL C ho lester o l < 50 m g /d L, T riglyceri d es 1 50 m g /d L F a sting g lu co se 110 m g/d L Cholesterol Education Program Adult Treatment Panel III Metabolic Syndrome MetSyn may be mediating mechanism between NBP dipping and CVD Associated with almost three-fold increased risk of CVD6 Research addressing association between NBP dipping and the MetSyn is limited Linked to NBP Dipping in some studies Greater prevalence of MetSyn in non-dippers versus dippers7,8, 9 Higher mean score of MetSyn (when measured continuously) in non-dippers than dippers10 No association in other studies11 NBP Dipping in Hispanics Evidence exists that NBP Dipping differs by race African-Americans more likely to have “blunted” NBP Dipping than non-Hispanic Whites, and be classified as non-dippers12,13 Little to no work to date on NBP Dipping and CVD outcomes in Hispanics Some evidence that Hispanic men may be more likely to be non-dippers than non-Hispanic Whites, but not true for Hispanic women14 One study found greater odds of stroke in nondippers versus dippers for African-Americans and non-Hispanic Whites, but not in Caribbean Hispanics15 NBP Dipping and MetSyn in Hispanics Among ethnic minority groups in U.S., Mexican-Americans have one of highest rates of MetSyn16 No studies have looked at link between NBP Dipping and MetSyn in Hispanics or nondiseased populations, or examined whether acculturation, which has been shown to affect the relationship between risk factors and CVD outcomes, moderates relationship Note. Image courtesy http://img.medscape.com/slide/migrated/editorial/cmecircle/2006/5186/images/caballero/slide032.gif Current Study Purpose: To examine relationship between NBP dipping and MetSyn in Mexican-American women and explore whether association is modified by acculturation level Sample: 277 middle-aged (M=49.56yrs) healthy Mexican-American women, recruited from South San Diego border community Inclusion criteria: age between 40-65 years, Mexican-American ethnicity, literate in English or Spanish, and free of major health conditions (e.g., CVD, cancer) and medications with autonomic effects Methods: Completed battery of questionnaires assessing sociodemographic, health history/behavior, and psychosocial factors, and next day underwent assessment of MetSyn components and completed 36hr ambulatory BP (AmBP) protocol Assessment NBP Dipping Acculturation AmBP monitor recorded participants’ BP every half hour during day, every hour during night Resulted in an average of 60 BP readings per person over 36 hours Calculated as : (average diurnal BP - average NBP)/ average diurnal BP*100 Measured using preferred language version of survey (commonly used proxy) Low Acculturated (Spanish) = 0; High Acculturated (English) = 1 MetSyn (defined using NCEP ATP III criteria) Waist circumference, height, weight measured by trained assessors Average SBP, DBP recorded as mean of 3 measurements while seated Glucose, HDL, triglycerides obtained through fasting blood draw Analyses Hierarchical Linear Modeling (HLM) used to obtain average diurnal and nocturnal BP levels across repeated measurements while accounting for nesting of measurements within individuals Logistic Regression used to test effects of NBP dipping (SBP and DBP), acculturation, and their interaction on probability of MetSyn Covariates (identified from prior research) included: Average daytime BP Age Body Mass Index Socioeconomic status (measured by educational attainment) Results No significant association between Diastolic BP dipping or Diastolic NBP dipping*Acculturation interaction and MetSyn Significant Systolic NBP (NSBP) dipping*Acculturation interaction B Age Educat ion Avg Da y SBP BMI NSBP D ipp ing Accu lturat ion Constant NSBP D ipp ing * Accu lturat ion S.E. 0.0 3 7 -0.0 5 1 0.0 3 5 0.1 8 7 0.0 1 2 0.0 4 7 -12. 4 71 0.1 6 3 0.0 0.0 0.0 0.0 0.0 0.3 2.3 Wald df Sig. 95% C.I. for EXP(B) Lower Upper Exp(B) 27 44 15 34 29 95 81 1.9 3 1 1.3 0 4 5.0 6 7 29. 7 69 0.1 7 7 0.0 1 4 27. 4 32 1 1 1 1 1 1 1 0.1 0.2 0.0 0.0 0.6 0.9 65 54 24 00 74 05 0 0.0 6 3 6.8 4 1 1 0.0 0 9 1.0 0.9 1.0 1.2 1.0 1.0 38 51 35 06 12 48 0 1.1 7 8 0.9 0.8 1.0 1.1 0.9 0.4 85 72 04 28 56 83 1.0 9 3 1.0 3 7 1.0 6 7 1.29 1.0 7 2 2.2 7 5 1.0 4 2 1.3 3 1 Results Decreased NSBP dipping associated with increased risk for MetSyn (i.e., increased NSBP dipping protective), but only for high acculturated women Association between Gradations of Systolic NBP (NSBP) Dipping and Odds of MetSyn in High Acculturated women § * * * p < .05 § Odds Ratios p<.10 Conclusions Systolic NBP dipping associated with MetSyn in high-acculturated but not low-acculturated Mexican-American women Each 10% decrease in dipping associated with 3.67 increased odds of MetSyn Trend for non-dippers having three fold greater odds of MetSyn as compared to dippers (p=.06) Diastolic NBP dipping not associated with MetSyn Finding suggests mechanisms by which NBP dipping relate to MetSyn may differ by acculturation Less acculturated, more traditional women may be buffered against harmful metabolic effects of increased blood pressure load Potential Buffering Mechanisms Sociodemographic Factors Psychosocial Factors Marital Status, Income Social support, Anger, Hostility, Chronic Stress, Racism Behavioral Factors Smoking, alcohol consumption, physical activity Addition of these factors in exploratory follow-up analyses attenuated interaction effect, but it remained statistically significant Interestingly, for high-acculturated women NSBP dipping associated with DBP, waist circumference and HDL components of MetSyn; for low-acculturated, only waist circumference Limitations/Future Directions Limitations Cross-sectional study Ambulatory BP measurement for dipping only 36 hour cycle No gender or ethnic comparisons possible Future directions Explore whether NBP dipping association with CVD outcomes varies by acculturation status in Hispanics Determine whether NBP dipping is related to other, non-metabolic factors in low-acculturated Hispanics (e.g., serum uric acid levels, hyperthyroidism, hyperaldosteronism)17 Cross-gender and cross-ethnic comparisons with Hispanics on association between NBP dipping and CVD outcomes References 1. Staessen, J., Thijs, L., Fagard, R., O'Brien, E., Clement, D., de Leeuw, P., & …Webster, J. (1999). Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA: The Journal Of The American Medical Association, 282(6), 539-546 2. Kabutoya, T., Hoshide, S., Ishikawa, J., Eguchi, K., Shimada, K., & Kario, K. (2010). The effect of pulse rate and blood pressure dipping status on the risk of stroke and cardiovascular disease in Japanese hypertensive patients. American Journal Of Hypertension, 23(7), 749755 3. Sega, R., Facchetti, R., Bombelli, M., Cesana, G., Corrao, G., Grassi, G., & Mancia, G. (2005). Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation, 111(14), 1777-1783 4. Alioglu, E., Turk, U., Bicak, F., Tengiz, I., Atila, D., Barisik, V., & ... Akin, M. (2008). Vascular endothelial functions, carotid intima-media thickness, and soluble CD40 ligand levels in dipper and nondipper essential hypertensive patients. Clinical Research In Cardiology: Official Journal Of The German Cardiac Society, 97(7), 457-462 References 5. Cuspidi, C., Giudici, V., Negri, F., & Sala, C. (2010). Nocturnal nondipping and left ventricular hypertrophy in hypertension: an updated review. Expert Review Of Cardiovascular Therapy, 8(6), 781-792. 6. Wilson, P., D'Agostino, R., Parise, H., Sullivan, L., & Meigs, J. (2005). Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation, 112(20), 3066-3072. 7. Ayala, D., Hermida, R., Chayan, L., Mojón, A., Fontao, M., & Fernández, J. (2009). Circadian pattern of ambulatory blood pressure in untreated hypertensive patients with and without metabolic syndrome. Chronobiology International, 26(6), 1189-1205. 8. Hassan, M., Jaju, D., Albarwani, S., Al-Yahyaee, S., Al-Hadabi, S., Lopez-Alvarenga, J., & ... Bayoumi, R. (2007). Non-dipping blood pressure in the metabolic syndrome among Arabs of the Oman family study. Obesity (Silver Spring, Md.), 15(10), 2445-2453. 9. Hermida, R., Chayán, L., Ayala, D., Mojón, A., Domínguez, M., Fontao, M., & ... Fernández, J. (2009). Association of metabolic syndrome and blood pressure nondipping profile in untreated hypertension. American Journal Of Hypertension, 22(3), 307-313. References 10. Tartan, Z., Uyarel, H., Kasikcioglu, H., Alper, A., Ozay, B., Bilsel, T., & ... Cam, N. (2006). Metabolic syndrome as a predictor of non-dipping hypertension. The Tohoku Journal Of Experimental Medicine, 210(1), 57-66. 11. Cuspidi, C., Meani, S., Fusi, V., Severgnini, B., Valerio, C., Catini, E., & ... Zanchetti, A. (2004). Is the nocturnal fall in blood pressure reduced in essential hypertensive patients with metabolic syndrome?. Blood Pressure, 13(4), 230-235. 12. Ancoli-Israel, S., Stepnowsky, C., Dimsdale, J., Marler, M., Cohen-Zion, M., & Johnson, S. (2002). The effect of race and sleep-disordered breathing on nocturnal BP "dipping": analysis in an older population. Chest, 122(4), 1148-1155 13. Sherwood, A., Thurston, R., Steffen, P., Blumenthal, J., Waugh, R., & Hinderliter, A. (2001). Blunted nighttime blood pressure dipping in postmenopausal women. American Journal Of Hypertension, 14(8 Pt 1), 749-754. 14. Hyman, D., Ogbonnaya, K., Taylor, A., Ho, K., & Pavlik, V. (2000). Ethnic differences in nocturnal blood pressure decline in treated hypertensives. American Journal Of Hypertension, 13(8), 884-891 References 15. Phillips, R., Sheinart, K., Godbold, J., Mahboob, R., & Tuhrim, S. (2000). The association of blunted nocturnal blood pressure dip and stroke in a multiethnic population. American Journal Of Hypertension, 13(12), 1250-1255. 16. Ford, E., Giles, W., & Dietz, W. (2002). Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA: The Journal Of The American Medical Association, 287(3), 356-359. 17. Kanbay, M., Turgut, F., Uyar, M., Akcay, A., & Covic, A. (2008). Causes and mechanisms of nondipping hypertension. Clinical And Experimental Hypertension (New York, N.Y.: 1993), 30(7), 585-597