Sedative-Hypnotic Drugs and Anxiety Disorders.
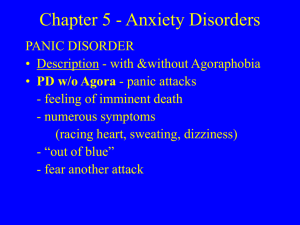
advertisement

Sedative-Hypnotic Drugs and Anxiety Disorders. Patrick T. Ronaldson, PhD Department of Medical Pharmacology University of Arizona Anxiety Term used to describe both symptoms and disorders Occurs normally as signal of impending danger or threat Very common, occurs in many disorders in addition to the anxiety disorders Differentiated from fear on basis of whether there is a clear source of danger i.e. “fight or flight” response Adaptive value : helps to plan and prepare for threat moderate levels enhance learning and performance Maladaptive when chronic / severe Anxiety Symptoms include : physiological symptoms of activated sympathetic nervous system (increased heart rate, increased respiration, sweating etc.) cognitive component (awareness of being frightened) behavioral components (urge to escape) Anxiety Disorders (DSM-IV) Panic disorder with or without agoraphobia Agoraphobia without panic disorder Specific phobias Social phobia Obsessive compulsive disorder Posttraumatic stress disorder Acute stress disorder Generalized anxiety disorder Anxiety disorder due to a general medical condition Substance-induced anxiety disorder Anxiety disorder not otherwise specified Anxiety Disorders: Prevalence 17% 13% Lifetime Prevalence of Anxiety Disorders: 25% 7.8% 5% 3.5% 2.5% Kessler RC, et al. Arch Gen Psychiatry 1994;51:8-19 Stein MB, et al. JAMA 1998;280:708-713 Kessler RC, et al. Arch Gen Psychiatry 1995;52:1048-1060 Spectrum of Depression and Anxiety Disorders Posttraumatic stress disorder Social anxiety disorder Depression Panic disorder Obsessive-compulsive disorder Generalized anxiety disorder Neurobiology of Anxiety Disorders CNS equilibrium is determined by a balance between excitatory and inhibitory neurotransmission Excitation -> Glutamate is prototypical NT. Inhibition -> GABA is prototypical NT. Inhibition via GABA is primarily mediated by the ionotropic GABA-A receptor. GABA binding to GABA-A results in an increase in neuronal Cl- conductance and subsequent neuronal hyperpolarization. Neurobiology of Anxiety Disorders Cl- - equilibrium potential is approximately -80 mV An increase in Cl- influx will decrease the resting potential of a neuron. Therefore, the post-synaptic neuron will require a greater excitatory stimulus to fire an action potential. Neurobiology of Anxiety Disorders GABA Receptor Benzodiazepines – major class of anxiolytic drugs. Act primarily via a selective binding sites on the GABA-A receptor. - high-affinity site. - low-affinity site. POTENTIATE the effects of GABA at the GABA-A receptor. Drugs useful in the treatment of anxiety disorders. Generic name Trade name Half-life (hrs) Dosage (mg/day) Long-acting benzodiazepines Diazepam Chlordiazepoxide Clorazepate Estazolam Prazepam Quazepam Halazepam Clonazepam* Flurazepam+ Valium Librium Tranxene ProSom Centrax Doral Paxipam Klonopin Dalmane 20-80 2-60 24-48 100 10-24 100 30-100 15-100 34 100 15-100 7.5-60 0.5-2.0 20-60 7.5-15 20-160 1.5-20 15-30 8 15 12 11 2 2 30-120 2-6 0.5-6 15-30 0.125-0.5 2-4 Short-acting benzodiazepines Oxazepam Lorazepam Alprazolam Temazepam+ Triazolam+ Midazolam# Serax Ativan Xanax Restoril Halcion Versed Non-benzodiazepine sedative/hypnotics Buspirone (BuSpar) Zolpidem (Ambien) Meprobamate (Miltown) Chloral hydrate (Noctec) Serotonin 1a agonist binds to benzodiazepine receptor * marketed as an anti-convulsant +marketed as a hypnotic #parenteral only Statement from the British Committee for the Review of Medicines. “All benzodiazepines are efficacious in the shortterm treatment of anxiety and insomnia. There is no evidence which can justify the particular use of any particular benzodiazepine in either anxiety or insomnia. The usual division of benzodiazepines into rigid treatment categories of antianxiety agents and hypnotics does not appear to be based on the known pharmacological or clinical properties of this group of compounds.” Caveat – different benzodiazepines have additional actions (i.e., muscle relaxants, anticonvulsants, anesthetics) and different half-lives. Benzodiazepines - Properties Prototypical Benzodiazepine = Diazepam (Valium). Highly lipophilic – well-absorbed orally and easily crosses the blood-brain and blood-placental barriers. Hepatic metabolism – converted to hydrophilic metabolites for renal elimination. Metabolite = desmethyldiazepam Same metabolite for diazepam, chlordiazepam, prazepam, and clorazepate. Desmethyldiazepam itself is pharmacologically active as an anxiolytic. Desmethyldiazepam is converted to oxazepam in the liver. Short-acting metabolite. Directly glucuronidated (as is lorazepam and flurazepam) and excreted by the kidney. Benzodiazepines - Properties Pharmacological Effects: Reduction of anxiety. Induction of sleep. Anesthesia – some benzodiazepines. Respiratory depression not as great as observed with barbiturates. Adverse Effects – primarily observed at plasma concentrations exceeding anxiolytic range. Expected side effects: sedation, ataxia, dependence. Impaired cognition and motor function. Confusion. Amnesia. Fatal overdose is uncommon, except when taken with alcohol. Benzodiazepines - Properties Benzodiazepines may induce tolerance in some individuals. Discontinuation of benzodiazepine therapy in tolerant patients MUST be gradual. Avoid hyperexcitability and possible seizures (more common with short-acting benzodiazepines). Block sedative side-effects of benzodiazepines with flumazenil (benzodiazepine receptor antagonist). Precipitate withdrawal symptoms in patients dependent on benzodiazepines (i.e., anxiety, insomnia, convulsions). Benzodiazepines - Indications Anxiety and Insomnia Sedation Mania Drug-induced hyperexcitability – PCP intoxication. Spasticity Cerebral Palsy Tetanus toxin toxicity. Anesthesia Alcohol withdrawal syndrome. Seizures. Clonazepam in myoclonic disorders. Diazepam, midazolam, and lorazepam in status epilepticus. Only effective early during status epilepticus. Evidence for seizure-induced translation change in GABA-A subunit expression. Benzodiazepines – Mechanism of Action GABA Receptor GABA-A receptors – highly variable (i.e., consist of different complements of alpha, beta, and gamma subunits). = different sensitivities to benzodiazepines. = a2 subunit is critical in sedative effects. Benzodiazepines do NOT activate the receptor directly. = increase frequency of chloride-channel opening produced by GABA. Autoradiography of GABA-A Receptors. a2 subunit Data shows that a2 subunit is localized to limbic system = Sedation. a3 subunit Further evidence – sitedirected mutagenesis against a2 subunit eliminates sedative effects of benzodiazepines. Pharmacological Effects of Benzodiazepines are Concentration-Dependent. Nanomolar Concentrations sedation – via a2 subunit. Action effectively blocked by flumazenil. Anxiolytic Micromolar Concentrations – diazepam, midazolam, lorazepam. Activity due to binding of benzodiazepines to lowaffinity site on GABA-A receptor. Anesthesia Practical Points regarding Benzodiazepines. Lowest effective dose for the shortest possible time. Discontinuance withdrawal is most common with shortacting benzodiazepines. Minimizes dependence and withdrawal. Cessation of long-acting drugs produces a tapering effect due to long elimination half-life. Patients on short-acting benzodiazepines need weeks to months to be weaned. Generally, benzodiazepines are safe drugs with few medical complications and do not interact adversely with other medications. Newer sedative/hypnotic drugs. Different mechanisms of action as compared to benzodiazepines. Do not act on GABA-A receptors. May interact only with specific GABA-A receptor subunits. Designed to produce anxiolytic effects without undesirable side effects associated with benzodiazepines. Daytime sedation and drowsiness. CNS depression in combination with alcohol. Potential for dependence. Buspirone (BuSpar®) Partial agonist at the serotonin 1a receptor. Relieves anxiety without producing sedation, impairment of motor skills, or memory loss. Does not induce withdrawal symptoms upon discontinuation. Does not act immediately. Can take up to 1 week to become effective. Used for chronic anxiety states. Pharmacokinetics: Rapidly absorbed orally. Rapid first-pass effect. Elimination half-life = 2-4 hrs. Metabolism is primarily hepatic. Serotonin Pathways in the CNS Serotonin and Anxiety Serotonin supported by efficacy of SSRIs major nuclei: CRN limbic/ prefrontal cortex structures Mediates fear/ anticipatory anxiety RRN prefrontal cortex, basal ganglia, thalamus, limbic cortex, substantia nigra, periaqueductal grey Modulates cognitive/ behavioural components strong feedback relationship with limbic cortex. Zolpidem (Ambien®) Produces sedative properties by binding selectively to a1-subunit. Same site that also binds benzodiazepines. Evidence – pharmacological effects blocked by flumazenil. Structurally unrelated to benzodiazepines. Used clinically for treatment of insomnia. Minimal muscle relaxing and anticonvulsant effects. Less potential for dependence and withdrawal. Pharmacokinetics: Elimination half-life = 1.5-3.5 hrs. Largely metabolized in the liver.