14_Neonatal
advertisement

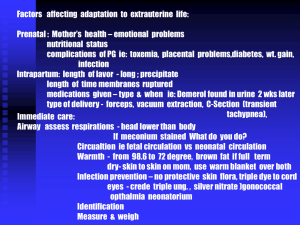
Neonatal Emergencies Objectives • Relate the history of resuscitation. • Outline the sequence of care in the resuscitation of a newborn. • Describe the difference between the newly born and newborn, and the common reasons they may require or seek emergency care. Introduction • Neonate: 0-28 days • Newly born: Immediately at birth when fetus is physiologically converting to newborn life Case Study 1: “Abdominal Pain” • A 16-year-old girl arrives in your ED with abdominal pain. • She states she is pregnant and is having abdominal pain about every 1 to 2 minutes. • Her appearance is anxious but alert; she breathes rapidly with pain but then slows her rate between episodes of pain. • There are no retractions, and her skin color is normal. Initial Assessment PAT: – Normal appearance, normal breathing, normal circulation Vital signs: – HR 120, RR 22, BP 100/70, T 38°C Questions What three questions should the patient be asked to predict the need for resuscitation of the newborn? What priorities of care should be initiated to resuscitate the newborn? Brief Resuscitation-Oriented History Case Progression (1 of 2) • The patient states that: – She does not think she has twins. – Her due date is in 3 weeks. – The color of the fluid has been clear. Case Progression (2 of 2) • Exam shows baby’s head crowning. What priorities of care should be initiated to resuscitate the newly born? Preparation for Delivery • Assume that the infant will be depressed. • Locate all necessary equipment in advance. Equipment for Neonatal Resuscitation • • • • • • Manual resuscitator (infant) Masks (2 sizes, term and premature) Dry towels/blankets Suction equipment ET tubes (sizes 2.5, 3.0, 3.5) Laryngoscope and blades (sizes 0, 1) Newborn Resuscitation Priorities (1 of 11) • Clear meconium as needed when head delivers. Newborn Resuscitation Priorities (2 of 11) • Deliver baby. – Place your hand around neck posteriorly and one underneath head to control delivery. Newborn Resuscitation Priorities (3 of 11) • Deliver baby. – If baby’s anterior shoulder does not deliver, gently pull downward on head to allow shoulder to clear. Newborn Resuscitation Priorities (4 of 11) • Deliver baby. – Tie or clamp cord in two places and cut between ties/clamps. Newborn Resuscitation Priorities (5 of 11) Newborn Resuscitation Priorities (6 of 11) Newborn Resuscitation Priorities (7 of 11) Newborn Resuscitation Priorities (8 of 11) • Assess breathing, tone, and color. – If not normal, then warm, dry, position, stimulate, and give oxygen. Newborn Resuscitation Priorities (9 of 11) • Begin bag-mask ventilation if apneic or heart rate is less than 100 bpm. Newborn Resuscitation Priorities (10 of 11) • Assess heart rate. – If less than 60 bpm after 30 sec of bagmask ventilation, begin chest compressions and prepare medications. Newborn Resuscitation Priorities (11 of 11) • Epinephrine is indicated when HR is <60 bpm after 30 sec of assisted ventilation plus 30 sec of chest compressions. • Access may be difficult: – Tracheal – Umbilical vein Challenging Resuscitation Conditions • Technical problems: – Esophageal or mainstem intubation, hypoxia, hypoventilation • Unrecognized pulmonary problems: – Pneumothorax, meconium aspiration, diaphragmatic hernia • Severe metabolic problems: – Acidosis, hypoglycemia, hypothermia • Other: – Congenital anomalies, severe anemia Case Progression/Outcome • 16-year-old delivered a near-term infant. • Baby had poor tone and color initially, but with suctioning, drying, warming, and stimulation became vigorous with good cry, tone, and color. Case Study 2: “Fever” • Mother brings 3-week-old boy to private physician’s office with decreased feeding today and fever. • Infant is sleeping, has normal tone, no retractions, and color is normal. Initial Assessment (1 of 2) PAT: – Normal appearance, normal breathing, normal circulation Vital signs: – HR 120, RR 40, T 38.7°C, Wt 3.5 kg Initial Assessment (2 of 2) A: B: C: D: E: Open, no stridor Normal rate and depth Normal pulse quality and rate Good tone, nonfocal No trauma, no rash Focused History/ Detailed Physical Examination • SAMPLE: Fever, mild irritability, normal birth history, taking formula but less than previous • Physical exam: No meningismus, no rash, infant taking a bottle Question What is your general impression of this patient? How would you transport this infant to the ED? General Impression • Stable infant with fever: – Transport may be by private car or BLS transport. – Good communication must exist with parents and ED staff. ED Management Priorities • Thorough history, physical exam, and full sepsis evaluation to determine source of infection. – Bacteremia rates in neonates with fever are much higher (7%-12%) than in older infants with fever. Case Discussion: Fever • Infections occurring after 5 days of life are termed “late onset.” • Causes include: – Gram-negative organisms (e.g., E coli, Klebsiella, Enterobacter) – Gram-positive organisms (e.g., Staphylococcus aureus, group B strep, Streptococcus pneumoniae) – Other infections: Salmonella (infectious gastroenteritis), Listeria monocytogenes (meningitis), herpes simplex virus (meningitis, skin vesicles) Case Progression/Outcome • CBC, blood culture, urinalysis, urine culture, lumbar puncture, CSF culture, and chest radiograph were performed. • All were negative except the urine, which showed 20 WBCs. • Infant was admitted and treated with intravenous antibiotics. Case Study 3: “Not Acting Right” • 12-day-old girl is brought to the ED by her mother with a complaint of “not acting right.” • Mom states that the infant has been listless for the past day and now will not take a bottle. • Baby appears to be asleep and does not arouse with removal of her clothes. She has no retractions, and her color is pale. Initial Assessment PAT: – Abnormal appearance, normal breathing, abnormal circulation Vital signs: – HR 170, RR 40, BP 70/50, T 37°C, Wt 3 kg ABCDEs: – Normal except for tachycardia, pale skin, and poor tone Focused History/ Detailed Physical Examination Head: Fontanel flat Neck: Without meningismus Lungs: Clear Cardiac: No murmur Abdomen: Nondistended, nontender Neurologic: Poor tone and poorly arousable Extremities: No rash Question What is your general impression of this patient? General Impression • Shock or primary CNS/metabolic abnormality What are your initial management priorities? Management Priorities • • • • Monitor cardiorespiratory function. Place infant on oxygen. Establish intravenous access. Obtain rapid glucose test and draw samples for tests and cultures. • Obtain head CT. • Begin empiric antibiotic therapy for possible sepsis. Case Discussion: Lethargy • Lethargy in a neonate suggests life-threatening disease. • Main causes may include: – Infection – Metabolic disease – Sepsis – Anemia (severe) – Trauma Case Outcome • Rapid bedside glucose was 30 mg/dL, and serum ammonia was 400 µmoles. • D10W was administered. • Patient was admitted to PICU for care and hemodialysis for urea cycle defect. Case Study 4: “Jaundice” • 5-day-old boy is brought to the ED by his parents with the complaint of “appears yellow.” • Baby had vacuum delivery but otherwise is well. • Baby is alert, with good tone, no retractions, and color of skin is yellow. Initial Assessment PAT: – Normal appearance, normal breathing, normal circulation Vital signs: – HR 120, RR 36, T 37.8°C, Wt 3.3 kg ABCDEs: – Normal Focused History/ Detailed Physical Examination • Baby is breastfed and has good suck. • Birth weight was 3.3 kg. • Baby’s sleeping patterns have not changed since birth. • Physical exam reveals a jaundiced baby with a cephalohematoma. Question What is your general impression of this patient? General Impression • Stable patient with jaundice What are your initial management priorities? ED Management Priorities • Obtain blood for serum bilirubin measurement. – Determine total and direct bilirubin. • Consider ordering other laboratory tests, including blood typing and Coombs test, CBC, and reticulocyte count. Background: Jaundice • Bilirubin can exist in one of two forms: – Unconjugated (indirect-reacting) – Conjugated (direct-reacting) • Three fundamental causes of hyperbilirubinemia: – Increased heme degradation (indirect) – Delay in maturation or inhibition of conjugation mechanism (indirect) – Obstruction of excretion from the liver (direct) Common Causes of Jaundice • “Physiologic jaundice”: – Peaks at about 3 days of age – Multifactorial – may be due to immature conjugation mechanism in liver • “Breast milk jaundice”: – Peaks after 4 days of age – Results from breast milk inhibitors of conjugation Causes of Nonphysiologic Jaundice • Indirect hyperbilirubinemia: – Hemolysis – Extravasation of blood (cephalohematoma) – ABO incompatibility, Rh disease – Sepsis – Drugs • Direct hemolysis Hemolysis • Intrinsic: – Congenital defects of RBC membrane (hereditary spherocytosis), or RBC hemoglobin (thalassemia, sickle cell disease), or RBC enzyme deficiency (G6PD, pyruvate kinase) • Extrinsic: – Isoimmunization (ABO incompatibility, Rh disease), bacterial sepsis, or drugs Extravasation of Blood • Common causes include: – Cephalohematoma – Vacuum extractor hematoma – Bruising with breech presentation – Traumatic or premature delivery – Intraventricular hemorrhage Direct Hyperbilirubinemia • Occurs when >20% of total bilirubin is conjugated (direct-acting). • Always abnormal • Results from interference of excretion of bilirubin from liver: – Intrahepatic: Hepatitis (infections), metabolic disease (galactosemia) – Extrahepatic: Biliary atresia, choledochal cyst Case Progression • Total bilirubin level is 20 mg/dL; 19 mg/dL is indirect. • Cause is probably multifactorial: – Breast milk jaundice – Extravasation of blood with resolving cephalohematoma What are your management priorities now? Further Management Case Outcome • Baby was admitted for phototherapy. • Discharged 2 days later with a bilirubin of 14 mg/dL. Case Study 5: “Swollen Belly Button” • 6-day-old girl is brought in by father with 2-day history of increasing redness and swelling of the belly button. • Baby is irritable with increased respiratory rate without retractions; skin is normal in color. Initial Assessment PAT: – Abnormal appearance, normal breathing, normal circulation Vital signs: – HR 170, RR 48, T 39°C, Wt 3.5 kg Question What are your management priorities? ED Management Priorities • The concern is omphalitis, which is a lifethreatening infection of the umbilicus. • Place on cardiorespiratory monitor. • Obtain IV access and send blood samples for CBC and culture. • Begin fluid resuscitation with normal saline at 20 mL/kg. • Administer empiric antibiotics. Umbilical Problems • Delayed separation >3 weeks may be normal or due to immune deficiency or sepsis. • Bleeding due to irritation • Granulation tissue • Umbilical hernia • Discharge: Omphalomesenteric duct or patent urachus • Infection: Omphalitis Case Outcome • The baby was admitted. • Vancomycin and cefotaxime were administered. • Baby required three surgical debridements of necrotic tissue but survived. The Bottom Line • Resuscitation of the newly born requires preparation and skill. • Many life-threatening conditions in the newborn period may present with few signs or symptoms.