Slides - Projects In Knowledge
advertisement

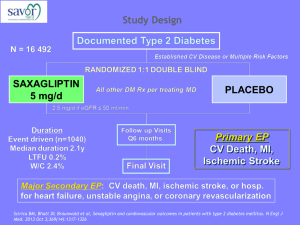
Type 2 Diabetes Treatment: Novel Therapies GLP-1 Receptor Agonists/Analogs and DPP-4 Inhibitors Jaime A. Davidson, MD, FACP, MACE Clinical Professor of Medicine Division of Endocrinology Touchstone Diabetes Center The University of Texas Southwestern Medical Center Dallas, Texas Major Therapeutic Targets in T2DM Liver Hepatic glucose overproduction Pancreas Sulfonylureas Meglitinides Beta-cell dysfunction GLP-1 agonists DPP-4 inhibitors Muscle and fat Metformin Thiazolidinediones GLP-1 agonists DPP-4 inhibitors Kidney Glucose reabsorption Glucose level Gut Glucose absorption Insulin resistance Thiazolidinediones Metformin Alpha-glucosidase inhibitors GLP-1 agonists SGLT-2 inhibitors Abbreviations: DPP-4, dipeptidyl peptidase-4; GLP-1, glucagon-like peptide-1; T2DM, type 2 diabetes mellitus. DeFronzo RA. Ann Intern Med. 1999;131:281-303. Buse JB, et al. In: Williams Textbook of Endocrinology. 10th ed. WB Saunders; 2003:1427-1483. Limitations of Older Agents for T2DM Agent Limitation Hypoglycemia Secretagogues, insulin Weight gain Secretagogues, glitazones, insulin Edema Glitazones, insulin GI side effects Metformin, alpha-glucosidase inhibitors Lactic acidosis (rare) Metformin Safety issues in elderly, renalimpaired, or CHF patients Glitazones, metformin, sulfonylureas Poor response rates All oral medications Lack of durable effect All oral monotherapy except glitazones Abbreviations: CHF, congestive heart failure; GI, gastrointestinal. Function of Incretins in Healthy Individuals Role of Incretins in Glucose Homeostasis Ingestion of food GI tract Glucose-dependent Increased insulin from beta cells (GLP-1 and GIP) Release of gut hormones — incretins Pancreas Active GLP-1 and GIP DPP-4 enzyme Glucose-dependent Decreased glucagon from alpha cells (GLP-1) Inactive Inactive GLP-1 GIP Abbreviations: DPP-4, dipeptidyl peptidase-4; GIP, gastric inhibitory polypeptide; GLP-1, glucagon-like peptide-1. Increased glucose uptake by muscles Decreased blood glucose Decreased glucose production by liver Kieffer TJ, Habener JF. Endocr Rev. 1999;20:876-913. Ahrén B. Curr Diab Rep. 2003;2:365-372. Drucker DJ. Diabetes Care. 2003;26:2929-2940. Holst JJ. Diabetes Metab Res Rev. 2002;18:430-441. Actions of GLP-1 Action GLP-1 Stimulation of insulin secretion √ Inhibition of glucagon secretion √ Reduction in circulating glucose √ Delayed gastric emptying √ Induction of satiety/reduction of food intake √ Potentially improved myocardial and endothelial function √ Possible neuroprotection √ Drucker DJ. Cell Metab. 2006;3:153-165. Grieve DJ, et al. Br J Pharmacol. 2009;157:1340-1351. Orskov C, et al. Endocrinology. 1988;123:2009-2013. Freeman JS. Cleve Clin J Med. 2009;76(suppl 5):S12-S19. DPP-4 • Transmembrane cell surface aminopeptidase expressed in liver, lungs, kidneys, intestines, lymphocytes, and endothelial cells1 – Active extracellular domain also circulates as free soluble DPP-4 in plasma1 • Active site is in a large “pocket”2 – Access limited to substrates with small side chains (eg, proline, alanine)2 – Active site cleaves to proline or alanine from 2nd aminoterminal position, inactivating its substrates1 • Key substrates: GLP-1 and GIP2 – Rapid and efficient metabolism by DPP-4 = short half-lives (~2 minutes for GLP-1)3 1. Drucker DJ, et al. Lancet. 2006;368:1696-1705. 2. Kirby M, et al. Clin Sci (Lond). 2009;118:31-41. 3. Chia CW, et al. Diabetes Metab Syndr Obes. 2009;2:37. Incretin Dysfunction in T2DM The Incretin Effect • Oral glucose vs IV glucose infusion: differences in insulin secretion – Insulin secretion is significantly higher with oral glucose vs IV glucose infusion (“incretin effect”) • Incretin effect is diminished in T2DM patients – Failure of insulin secretion Nauck M, et al. Diabetologia. 1986;29:46-52. Postprandial GLP-1 Levels in IGT and T2DM GLP-1 AUC Incremental from Basal (pmol/L• 240 min) 2500 2500 2000 2000 1927 1587 1587 1500 1500 P <.001 for T2DM vs NGT 907 1000 1000 500 500 00 NGT IGT T2DM Abbreviations: AUC, area under the curve; IGT, impaired glucose tolerance; NGT, normal glucose tolerance. Toft-Nielsen MB, et al. J Clin Endocrinol Metab. 2001;86:3717-3723. 2 Strategies for GLP-1 Enhancement GLP-1 analogs DPP-4 inhibitors • Chemically modified GLP-1, not susceptible to DPP-4 metabolism – Longer half-lives • FDA approved: exenatide BID and qwk and liraglutide • Investigational – Albiglutide – Lixisenatide – Dulaglutide • Block DPP-4 so that it blunts breakdown of GLP-1 – Raise endogenous GLP-1 levels; should also raise GIP • FDA approved: alogliptin, linagliptin, saxagliptin, and sitagliptin • Vildagliptin (approved outside United States) • Oral administration • Subcutaneous injection Drucker DJ, et al. Lancet. 2006;368:1696-1705. Gallwitz B. Pediatr Nephrol. 2010;25:1207-1217. ClinicalTrials.gov. 2013. Accessed 12/11/13 at: http://www.clinicaltrials.gov. DPP-4 Inhibitors MOA Meal Intestinal GLP-1 release Intestinal GIP release Active GIP Active GLP-1 DPP-4 inhibitor DPP-4 Inactive GLP-1 Incretin effects – Augments glucose-dependent insulin secretion – Inhibits glucagon secretion and hepatic glucose production – Improves hyperglycemia DPP-4 inhibitor DPP-4 Inactive GIP Selective inhibition of DPP-4 increases plasma GLP-1 levels, resulting in reduction in glycemia 12 DPP-4 Inhibition Improves Active GLP-1 Levels Single-Dose OGTT Study • 3 arms (N = 58) – Placebo – Sitagliptin 25 mg – Sitagliptin 200 mg • Increase in active GLP-1 with sitagliptin compared with placebo – Placebo: active GLP-1 increases to ~7 pM at 2−3 h – Sitagliptin: active GLP-1 increases to ~15−20 pM and remains higher than placebo for ~6 h Abbreviation: OGTT, oral glucose tolerance test. Herman GA, et al. J Clin Endocrinol Metab. 2006;91:4612-4619. Linagliptin Pharmacodynamics Effect on GLP-1 and Glucagon Change from baseline in intact GLP-1 AUEC0–2h: Linagliptin: 18.5 pmol/h/L Placebo: 0.4 pmol/h/L P <.0001 Change from baseline in glucagon AUEC0–2h: Linagliptin: -17.4 pg/h/L Placebo: 1.3 pg/h/L P = .0452 Statistically significant differences in postprandial intact GLP-1 (increased) and glucagon (decreased) vs placebo after 4 weeks of treatment in T2DM patients Rauch T, et al. Diabetes Ther. 2012;3:10. Therapeutic Effect of GLP-1 in T2DM 10 patients with unsatisfactory control of T2DM received infusions of GLP-1 or placebo GLP-1 significantly increased GLP-1 significantly reduced • Insulin (17.4 nmol x 1-1 x min)* • C-peptide (228 nmol x 1-1 x min)* • *Decreased again after plasma glucose normalized. Nauck MA, et al. Diabetologia. 1993;36:741-744. • • Fasting plasma glucose (normal levels reached in all patients) Pancreatic glucagon secretion (-1418 pmol x 1-1 x min) Plasma nonesterified fatty acids (-26.3 mmol x 1-1 x min) GLP-1 Receptor Agonists and DPP-4 Inhibitors Effects on HbA1c, Glucose, and Insulin Levels Exenatide Has Beneficial Effects on FPG and Insulin in T2DM Abbreviation: FPG, fasting plasma glucose. Kolterman OG, et al. J Clin Endocrinol Metab. 2003;88:3082-3089. Peak Mean Incremental Serum Insulin (µU/mL) Mean FPG (mg/dL) N = 13 Exenatide Has Beneficial Effects on Postprandial Glucose and Glucagon in T2DM Exenatide 0.1 μg/kg Placebo Postprandial glucose, day 5 (mean) Baseline 15.9 mg/dL Baseline 170.3 mg/dL 180 min (nadir) 126.4 mg/dL 120 min (peak) 289.0 mg/dL 300 min 177.8 mg/dL 300 min 175.5 mg/dL Postprandial glucagon, day 5 (mean) Baseline 98.9 pg/mL Baseline 94.9 pg/mL <5%–6% change over 180 min 60 min 173.9 pg/mL 180 min 122.7 pg/mL N = 24. Kolterman OG, et al. J Clin Endocrinol Metab. 2003;88:3082-3089. Exenatide at 3 Years of Therapy Provides Sustained Effects on HbA1c • 217 patients randomized to placebo, 5 µg exenatide, or 10 µg exenatide during prior 30-week placebo-controlled studies were transitioned to open-label exenatide treatment • All patients had a minimum of 3 years of exenatide exposure for this analysis • By week 12, exenatide reduced HbA1c by 1.1% • Reduction in HbA1c was sustained throughout 156 weeks of treatment – Change from baseline to week 156 = -1.0% (95% CI, -1.1 to -0.8); P <.0001 • 46% of patients achieved HbA1c ≤7%; 30% achieved HbA1c ≤6.5% Klonoff DC, et al. Curr Med Res Opin. 2008:24:275-286. Liraglutide 1-Year Monotherapy Reduces FPG and PPG Therapy Δ FPG (mg/dL) P Value for Liraglutide vs Glimepiride P Value for Liraglutide 1.8 vs 1.2 mg Glimepiride -5.2 Liraglutide 1.2 mg -15.1 .027 Liraglutide 1.8 mg -25.6 .0001 .0223 Δ PPG (mg/dL) P Value for Liraglutide vs Glimepiride P Value for Liraglutide 1.8 vs 1.2 mg Therapy Glimepiride -24.5 Liraglutide 1.2 mg -30.8 .1616 Liraglutide 1.8 mg -37.5 .0038 Abbreviations: FPG, fasting plasma glucose; PPG, postprandial glucose. Garber A, et al. Lancet. 2009;373:473-481. .1319 Liraglutide 1-Year Monotherapy Improves Glycemic Control • 52-week phase III study in 746 T2DM patients previously on diet and exercise or oral antidiabetic monotherapy • Baseline HbA1c was 8.3%–8.4% in all groups Liraglutide 1.2 mg (n = 251) Δ HbA1c (%) Glimepiride (n = 248) P = .0014 P = .0046 P <.0001 Garber A, et al. Lancet. 2009;373:473-481. Liraglutide 1.8 mg (n = 246) Effects of Liraglutide and Glimepiride Monotherapy on HbA1c Over 2 Years HbA1c Change (%) Disease duration: 0 ≥3 y <3 y -0.4 -0.5 (n = 55) Liraglutide 1.8 mg† Glimepiride -0.7 (n = 42) -1 -1* (n = 60) -1.5 -1.4* % achieving HbA1c <7% • 58% with liraglutide* • 37% with glimepiride (n = 54) * P <.05 vs glimepiride; † 73% completed 2-year extension. Garber AJ, et al. Diabetes. 2009;58(suppl 1):162-OR. Weight change • -2.7 kg with liraglutide* • 1.1 kg with glimepiride Effects of Exenatide qwk vs Exenatide BID on Glycemic Control Exenatide 10 mcg BID (n = 147) Baseline HbA1c: 8.3% 8.3% -0.5 -1 -1.5 -2 HbA1c < 7.0% (% of Patients) FPG Change (mg/dL) HbA1c Change (%) 0 -1.5 -1.9* 100 77* 80 61 0 -10 -20 -30 -25 -40 -50 -41* Similar cumulative incidences of nausea Exenatide BID, 35% of patients; Exenatide qwk, 26% of patients 60 40 Similar weight loss Approximately 4 kg in both groups 20 0 Approximately 90% of patients completed 30 weeks of treatment. * Exenatide 2.0 mg qwk (n = 148) P <.05 vs exenatide BID. Drucker DJ, et al. Lancet. 2008;372:1240-1250. Similar rates of minor hypoglycemia Exenatide BID, 6.1% of patients; Exenatide qwk, 5.4% of patients Exenatide qwk Delivered Powerful HbA1c Reductions Baseline HbA1c: 8.5% Exenatide qwk (n = 129) Blevins T, et al. J Clin Endocrinol Metab. 2011;96:1301-1310. 8.4% Exenatide BID (n = 123) Improvements in HbA1c with Exenatide qwk Were Sustained at 1 Year DURATION-2 Open-Label Extension Completer Analysis Primary Endpoint: Change in HbA1c (%) 0.0 Open-label period2† (N = 249) Blinded period1* (N = 326) -0.5 -1.0 n = 130 -1.5 n = 119 -2.0 0 4 6 10 14 18 22 26 26 30 34 Time (wk) Exenatide qwk *ITT population. †52-week evaluable population. LS mean (SE). 1. Bergenstal RM, et al. Lancet. 2010;376:431-439. 2. Wysham C, et al. Diabet Med. 2011;28:705-714. Sitagliptin 40 46 52 Exenatide qwk Percent to Goal Compared to Sitagliptin or Pioglitazone • Diet and exercise background Exenatide qwk1 (n = 248) Sitagliptin1 (n = 163) Pioglitazone1 (n = 163) HbA1c <7.0% 63%* 43% 61% HbA1c ≤6.5% 49%* 26% 42% *P <.001 vs sitagliptin. • Metformin background – A significantly greater percentage of patients achieved HbA1c <7.0% and HbA1c ≤6.5% with exenatide qwk than with sitagliptin (P <.0001) or pioglitazone (P <.05)2 1. Russell-Jones D, et al. Diabetes Care. 2012;35:252-258. 2. Bergenstal RM, et al. Lancet. 2010;376:431-439. Overview of GLP-1 Receptor Agonist Safety Data Odds Ratio (95% confidence interval) P Value 2.92 (1.49, 5.75) .002 With SUs 4.62 (1.89, 11.21) .001 Without SUs 1.37 (0.72, 2.63) .34 Cardiovascular events 0.99 (0.52, 1.91) .98 Nausea 3.88 (2.79, 5.42) <.001 Exenatide BID 8.38 (4.27, 16.48) <.001 Liraglutide 3.48 (2.29, 5.28) <.001 Vomiting 4.23 (2.67, 6.13) <.001 Diarrhea 2.36 (1.67, 3.33) <.001 Event Hypoglycemia*† • Meta-analysis • Predominantly exenatide and liraglutide – n = 5429 receiving GLP-1 receptor agonists – n = 3053 receiving active comparators or placebo * † Odds ratio based on analysis of exenatide bid trials. Severe hypoglycemia reported for 19 patients in exenatide BID trials and 1 patient in liraglutide trials. Abbreviation: SU, sulfonylurea. Monami M, et al. Eur J Endocrinol. 2009;160:909-917. Current DPP-4 Inhibitors Sitagliptin Vildagliptin (approved outside United States) Alogliptin Linagliptin Saxagliptin Comparative Efficacies of DPP-4s Placebo-corrected change from baseline in HbA1c - Monotherapy Alogliptin1 12.5 mg 7.9% 25 mg 7.9% Linagliptin2 5 mg 8.1% 5 mg 8.0% Saxagliptin3 5 mg 7%-10% 5 mg 8.0% Sitagliptin4 100 mg 100 mg 8.0% 8.0% Vildagliptin5 50 mg BID 50 mg 8.6% 8.4% -0.1 -0.2 -0.3 ΔHbA1c (%) -0.4 -0.4 -0.5 -0.6 -0.7 -0.56 -0.5 -0.59 -0.6 -0.6 -0.6 -0.7 -0.8 -0.7 -0.8 -0.9 -1.0 -1.1 The current DPP-4s have comparative efficacy -1.2 1. DeFronzo R, et al. Diabetes Care 2008;31:2315-2317. 2. Linagliptin Prescribing Information. 3. Saxagliptin Prescribing Information. 4. Sitagliptin Prescribing Information. 5. Vildagliptin Summary of Product Characteristics. Alogliptin Phase III Trials: HbA1c Change from Baseline After 26 Weeks Alogliptin monotherapy1 Add-on therapy LS Mean Change HbA1c from Baseline (%) Baseline HbA1c: 8.0% Baseline HbA1c (%) Alogliptin 12.5 mg Aloglitpin 25 mg Control Add-on to SU2 8.1 -0.39* -0.53* 0.01 Add-on to MET3 7.9 -0.6* -0.6* -0.1 Add-on to PIO4 8.0–8.1 -0.66* -0.80* -0.19 Add-on to insulin5 9.3 -0.63* -0.71* -0.13 Abbreviations: MET, metformin; PIO, pioglitazone; SU, sulfonylurea. *P <.001 vs control. 1. DeFronzo RA, et al. Diabetes Care. 2008;31:2315-2317. 2. Pratley RE, et al. Diabetes Obes Metab. 2009;11:167-176. 3. Nauck MA, et al. Int J Clin Pract. 2009;63:46-55. 4. Pratley RE, et al. Curr Med Res Opin. 2009;25:2361-2371. 5. Rosenstock J, et al. Diabetes Obes Metab. 2009;11:1145-1152. Linagliptin Significantly Reduced HbA1c After 24 Weeks in Patients on a Stable Insulin Dose Baseline HbA1c (%): 8.29 8.31 Full analysis set (last observation carried forward). Change-from-baseline HbA1c at Week 24 is the primary endpoint. *Model includes treatment, baseline HbA1c, renal function, concomitant OADs. †Sensitivity analyses (FAS OC and PPS) revealed similar results. Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. HbA1c Reduction with Linagliptin in Elderly Patients Over 75 Years • In a prespecified subgroup analysis, there was no significant interaction according to patient age group (P = .1000) • The study had a high proportion of elderly patients – 65−74 years: 26.1% linagliptin, 28.7% placebo – ≥75 years: 5.5% linagliptin, 6.5% placebo Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin Reduced HbA1c After 24 Weeks (Primary Endpoint) and Maintained it in a 52Week Free Insulin Titration Period Stable insulin dose Baseline to week 24 Free insulin dose starting at week 24 • The difference in HbA1c reduction between linagliptin and placebo was maintained during a 52-week free insulin titration period starting at week 24 (out to week 76) Full analysis set (last observation carried forward). *Model includes treatment, baseline HbA1c, renal function, concomitant OADs. Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin Significantly Reduced FPG After 24 Weeks and Maintained it in 28-Week Free Insulin Titration Period Change in FPG from baseline Stable insulin dose baseline to week 24 Free insulin dose starting at week 24 Week 24 Week 52 Placebo-adjusted change with linagliptin: -10.81 mg/dL Placebo: -5.41 mg/dL Full analysis set (observed case set). Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin: -3.60 mg/dL Insulin Dose Stabilized in 1st 24 Weeks and Increased in Both Groups in 2nd 28-Week Free-Titration Period, but With Greater Extent in Placebo Group Stable insulin dose Baseline to week 24 Full analysis set, original analysis. Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Free insulin dose starting at week 24 Safety Profile of Linagliptin Compared with Placebo After 52 Weeks • The overall risk of adverse events (AEs) with linagliptin (n = 631) vs placebo (n = 630): – Patients with any AEs ■ 78.4% with linagliptin vs 81.4% with placebo – Patients with investigator-defined drug-related AEs ■ 18.7% with linagliptin vs 22.2% with placebo – Patients with AEs leading to discontinuation of trial drug ■ 3.3% with linagliptin vs 4.4% with placebo – Patients with serious AEs ■ 13.8% with linagliptin vs 13.2% with placebo Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin, When Added to Insulin, and Its Association with the Risk of Hypoglycemia Week 24 Week 52 Improved glycemic control with linagliptin added to insulin does not appear to increase the risk of hypoglycemia Treated set (all patients who were treated with at least 1 dose of study medication). Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin Shows Rates of Hypoglycemia Similar to Placebo The Majority of Hypoglycemia is Nonsevere Investigator-defined hypoglycemia AEs at week 24 by category Placebo All Hypoglycemia AEs Documented Symptomatic (≤72 mg/dL) Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Linagliptin Documented Symptomatic (<54 mg/dL) Severe Study Summary: Linagliptin as Add-On to Insulin Efficacy and safety of linagliptin as add-on therapy to insulin in type 2 diabetes •Linagliptin significantly reduced HbA1c after 24 weeks in patients on a stable insulin dose (placebo-corrected reduction after 24 weeks -0.65%) •The efficacy of linagliptin was reliable in different prespecified subgroups, such as – Elderly patients age ≥75 years – Different categories of renal function •HbA1c reductions were maintained over 52 weeks •Linagliptin significantly reduced fasting plasma glucose after 24 weeks and maintained it in 28-week free insulin titration period •Linagliptin has a safety profile comparable to placebo •Incidence of hypoglycemia with linagliptin was comparable to placebo Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Both Sitagliptin and Saxagliptin Produced Greatest Reductions in HbA1c in Patients with High Baseline HbA1c Sitagliptin-Treated Subgroup with Baseline HbA1c >9% 50 mg QD 100 mg QD 0 Open-Label Saxagliptin in 66 Patients with Baseline HbA1c >10% to ≤12% 10 mg QD 0 –0.2 –0.2 –0.4 –0.4 –0.6 –0.6 –0.8 –0.8 –1.0 –1.0 –1.2 –1.2 –1.15 –1.18 –1.4 –1.6 –1.8 –2.0 –1.87 Hanefeld M, et al. Curr Med Res Opin. 2007;23:1329-1339. Rosenstock J, et al. Curr Med Res Opin. 2009;25:2401-2411 Incretin-Based Therapy Improves Glycemic Control When Used in Combination With Metformin Initial Tx Added to Metformin Added to TZD Added to Sulfonylurea Exenatide ✔1,2 ✔3 ✔4 Liraglutide ✔5 ✔6* ✔5,7 Alogliptin ✔8 ✔9 ✔10 ✔11 Linagliptin ✔12 ✔13 ✔14 ✔15 Sitagliptin ✔16 ✔17,18 ✔19,20 ✔21 Saxagliptin ✔22 ✔23 ✔24 ✔25 Abbreviation: TZD, thiazolidinedione. *Added to thiazolidinedione plus metformin. 1. Bergenstal RM, et al. Lancet. 2010;376:431-439. 2. DeFronzo RA, et al. Diabetes Care. 2005;28:1092-1100. 3. DeFronzo RA, et al. Diabetes Care. 2010;33:951-957. 4. Buse JB, et al. Diabetes Care. 2004;27:2628-2635. 5. Buse JB, et al. Lancet. 2009;374:39-47. 6. Zinman B, et al. Diabetes Care. 2009;32:1224-1230. 7. Marre M, et al. Diabet Med. 2009;26:268-278. 8. Pratley R, et al. ADA 2012. Abstract 1158-P. 9. Nauck MA, et al. Int J Clin Pract. 2009;63:46-55. 10. Pratley RE, et al. Curr Med Res Opin. 2009;25:2361-2371. 11. Pratley RE, et al. Diabetes Obes Metab. 2009;11:167-176. 12. Haak T, et al. Diabetes Obes Metab. 2012;14:565-574. 13. Taskinen MR, et al. Diabetes Obes Metab. 2011;13:65-74. 14. Gomis R, et al. Diabetes Obes Metab. 2011;13:653-661. 15. Lewin AJ, et al. Clin Ther. 2012;34:1909-1919.e15. 16. Williams-Herman D, et al. Curr Med Res Opin. 2009;25:569-583. 17. Charbonnel B, et al. Diabetes Care. 2006;29:2638-2643. 18. Nauck M, et al. Diabetes Care. 2009;32:8490. 19. Derosa G, et al. Metabolism. 2010;59:887-895. 20. Rosenstock J, et al. Clin Ther. 2006;28:1556-1568. 21. Hermansen K, et al. Diabetes Obes Metab. 2007;9:733-745. 22. Jadzinsky M, et al. Diabetes Obes Metab. 2009;11:611-622. 23. DeFronzo RA, et al. Diabetes Care. 2009;32:1649-1655. 24. Hollander P, et al. J Clin Endocrinol Metab. 2009;94:4810-4819. 25. Chacra AR, et al. Int J Clin Pract. 2009;63:1395-1406. Exenatide qwk HbA1c Reduction Compared with Sitagliptin or Pioglitazone Diet and exercise background1 Baseline : 8.5% Exenatide qwk (n = 248) 8.5% 8.5% Metformin background2 8.6% 8.5% 8.5% Exenatide qwk (n = 160) LS Mean. ITT population. *P <.001 vs sitagliptin. †P <.0001 vs sitagliptin ‡P <.05 vs pioglitazone. 1. Russell-Jones D, et al. Diabetes Care. 2012;35:252-258. 2. Bergenstal RM, et al. Lancet. 2010;376:431-439. Fasting Plasma Glucose Improvement Was Greater with Exenatide qwk and Pioglitazone Diet and exercise background1 Exenatide qwk (n = 248) Metformin background2 Exenatide qwk (n = 160) LS Mean. ITT population. *P <.05 exenatide qwk vs sitagliptin. 1. Russell-Jones D, et al. Diabetes Care. 2012;35:252-258. 2. Bergenstal RM, et al. Lancet. 2010;376:431-439 GLP-1 Receptor Agonists and DPP-4 Inhibitors Effects on Weight Why Is Weight a Concern? • Most patients with T2DM are overweight/obese • Some currently available therapies cause weight gain – Secretagogues – Glitazones – Insulin Exenatide Open-Label Extension Study Continuous Loss of Body Weight Baseline BMI (kg/m2) Baseline 99.3 kg Klonoff DC, et al. Curr Med Res. 2008;24:275-286. Δ Body Weight from Baseline to Week 156 (kg) Δ Body Weight from Baseline (kg) <30 Exenatide qwk Weight Reduction Compared with Sitagliptin or Pioglitazone Diet and exercise background1 Baseline (kg) : 87.5 Exenatide qwk (n = 248) 88.7 86.1 Metformin background2 89 87 Exenatide qwk (n = 160) *P <.001 vs sitagliptin. †P <.001 vs pioglitazone. ‡P = .002 vs sitagliptin. §P <.0001 vs pioglitazone. 1. Russell-Jones D, et al. Diabetes Care. 2012;35:252-258. 2. Bergenstal RM, et al. Lancet. 2010;376:431-439. 88 Effect of Liraglutide vs Standard Therapy on Body Weight Weight Change from Baseline (kg) Liraglutide 1.2 mg Liraglutide 1.8 mg Comparator(s) -2 to -3* (approximate) -2 to -3* (approximate) 1−2 with glimepiride (approximate) Add-on to metformin2 -2.6† -2.8† -1.5 with placebo 1.0 with glimepiride Add-on to SU3 0.3† -0.2† -0.1 with placebo 2.1 with rosiglitazone Add-on to metformin + TZD4 -1‡ -2‡ 0.6 with glimepiride Add-on to metformin + SU5 -1.8‡ Monotherapy1 -0.42 with placebo 1.6 with glargine *P = .0001 vs glimepiride; †P <.05 vs placebo; ‡P ≤.0001 vs placebo. Abbreviations: SU, sulfonylurea; TZD, thiazolidinedione. 1. Garber A, et al. Lancet. 2009;373:473-481. 2. Nauck M, et al. Diabetes Care. 2009;32:84-90. 3. Marre M, et al. Diabetic Med. 2009;26:268-278. 4. Zinman B, et al. Diabetes Care. 2009;32:1224-1230. 5. Russell-Jones D, et al. Diabetologia. 2009;52:2046-2055. Liraglutide Delayed Gastric Emptying • Comparative trial: liraglutide, glimepiride, placebo in T2DM patients (N = 46) • Gastric emptying was slowed with liraglutide, mainly during the first postprandial hour – Mean estimated acetaminophen AUC0-60 min ratios ■ 0.62 with liraglutide vs placebo (P <.001) ■ 0.67 with liraglutide vs glimepiride (P <.001) – Mean estimated percentage of acetaminophen exposure during the first postprandial hour (AUC0-60 min/AUC0-300 min) ■ 30% less with liraglutide compared with placebo (P <.001) ■ 29% less with liraglutide compared with glimepiride (P <.001) – Acetominophen Cmax ■ 20% lower with liraglutide compared with placebo (P ≤.006) ■ 15% lower with liraglutide compared with glimepiride (P ≤.006) Horowitz M, et al. Diabetes Res Clin Pract. 2012;97:258-266. Neutral Effect of DPP-4 Inhibitors on Body Weight • Sitagliptin produced statistically significant (P <.05) decreases of 0.5–0.8 kg in body weight from baseline at week 12 at all doses1 – Not significantly different from weight loss seen with placebo (-0.5 kg) • Saxagliptin reduced body weight by -0.1 to -1.2 kg at week 24 compared with baseline2 – Weight loss was -1.4 kg with placebo • In a comparative trial, mean weight loss after 26 weeks was -0.96 kg with sitagliptin vs -3.38 kg with liraglutide 1.8 mg and -2.86 kg with liraglutide 1.2 mg3 • Linagliptin produced no significant difference in body weight from baseline4 – No significant difference in body weight from baseline with placebo 1. Hanefeld M, et al. Curr Res Med Opin. 2007;23:1329-1339. 2. Rosenstock J, et al. Curr Med Res Opin. 2009;25:2401-2411. 3. Pratley RE, et al. Lancet. 2010;375:1447-1456. 4. Del Prato S, et al. Diabetes Obes Metab. 2011;13:258-267. Effect of Alogliptin Monotherapy on Body Weight at 26 Weeks DeFronzo RA, et al. Diabetes Care. 2008;31:2315-2317. Effect of Linagliptin on Body Weight When Added to Insulin Week 24 Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. Week 52 GLP-1 Receptor Agonists and DPP-4 Inhibitors Effects on Lipids Mean Δ from Baseline (mg/dL) Exenatide Has Beneficial Effects on Lipids Trigs TC LDL-C HDL-C Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol; Trigs, triglycerides. Klonoff DC, et al. Curr Med Res Opin. 2008;24:275-286. Effect of Exenatide qwk and Exenatide BID on Lipids Change from Baseline Exenatide qwk (n = 106) Exenatide BID (n = 105) LDL-C (mg/dL) -2.70 0.39 HDL-C (mg/dL) 1.24 0.19 Triglycerides (mg/dL) -31.86* -30.09* VLDL-C (mg/dL) -12.74* -13.13* -3.32 0.58 Non-HDL-C (mg/dL) *P <.05 from baseline. Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; VLDL-C, very lowdensity lipoprotein cholesterol. Chiquette E, et al. Vasc Health Risk Manag. 2012;8:621-629. Liraglutide Reduces Triglycerides and CVD Inflammatory Biomarkers Difference from Placebo in Change from Baseline (%) Liraglutide 0.65 mg Liraglutide 1.25 mg Liraglutide 1.90 mg Triglycerides1 -19* -15 -22* PAI-12 -14 -29* -25* BNP2 -26 -30* -38* hs-CRP2 -3 -12 -20 *P <.05. Abbreviations: BNP, B-type natriuretic peptide; CVD, cardiovascular disease; hs-CRP, high-sensitivity C-reactive protein; PAI-1, plasminogen activator inhibitor 1. 1. Vilsbøll T, et al. Diabetes Care. 2007;30:1608-1610. 2. Courrèges JP, et al. Diabet Med. 2008;25:1129-1131. Biomarkers of Cardiovascular Risk Were Reduced with Liraglutide vs SU Treatment difference -8.6 (95% CI -13.6 to -3.6) Treatment difference -0.065 (95% CI -0.106 to -0.025) Abbreviations: BNP, B-type natriuretic peptide; FFA, free fatty acids. Kaku K, et al. J Diabetes Invest. 2011;2:441-447. Δ from Baseline (mg/dL; mmol/L for FFA) Sitagliptin Has Mixed Effects on Lipids Trigs FFA Placebo Sit 25 mg qd Sit 50 mg qd Sit 100 mg qd TC LDL-C HDL-C Abbreviation: FFA, free fatty acids. Hanefeld M, et al. Curr Res Med Opin. 2007;23:1329-1339. Sit 50 mg BID Saxagliptin’s Effects on Lipids • Specific data were not provided in the published phase III trial • “Modest numerical improvements from baseline to week 24 in total cholesterol were demonstrated in the saxagliptin treatment groups.” • “There were no clear effects of saxagliptin on fasting lipid concentrations.” Rosenstock J, et al. Curr Med Res Opin. 2009;25:2401-2411. Effect of Linagliptin on Lipids in Patients at High Risk for Renal and CVD • Post-hoc pooled analysis of T2DM patients with hypertension and microalbuminuria from 6 phase III linagliptin trials (N = 512)* • No significant difference in lipid changes from baseline for linagliptin vs placebo *Study durations: 18–24 weeks. †Adjusted for baseline HbA1c, parameter measured, prior oral antidiabetic medications, study and treatment. Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol. von Eynatten M, et al. Cardiovasc Diabetol. 2013;12:60 GLP-1 Receptor Agonists and DPP-4 Inhibitors Effects on Blood Pressure and CVD Exenatide Reduced Systolic Blood Pressure in Clinical Trials ≥6 Months’ Duration Pooled data from 6 trials of exenatide in T2DM; N = 2171 Mean Change in Systolic Blood Pressure (mmHg) Exenatide -2.2 Placebo +0.6 Exenatide -4.5 Insulin -0.9 P Value .0002 <.0001 Mean Change in Diastolic Blood Pressure (mmHg) -0.7 -0.2 -1.6 -0.8 P Value .21 .16 • No differences between treatments in proportion of patients reducing number, type, or intensity of antihypertensive therapy • Reduction in blood pressure correlated only weakly with weight loss in exenatide-treated patients (r = 0.09; P = .002) Okerson T, et al. Am J Hypertens. 2010;23:334-339. Effect of Linagliptin on Blood Pressure in Patients at High Risk for Renal and CVD • Post-hoc pooled analysis of T2DM patients with hypertension and microalbuminuria from 6 phase III linagliptin trials (N = 512)* • No significant difference in blood pressure changes from baseline for linagliptin vs placebo *Study durations: 18–24 weeks. †Adjusted for baseline HbA1c, parameter measured, prior oral antidiabetic medications, study and treatment. Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure. von Eynatten M, et al. Cardiovasc Diabetol. 2013;12:60 CV Events with Incretin-Based Therapies Meta-analyses/Pooled Analyses Drug Name/Class Number of Studies Analyzed N CV Events Exenatide BID1 12 3945 (2316 exenatide BID; 1629 comparator) Risk ratio 0.70 (95% CI 0.38−1.31) Liraglutide2 15 6638 (4257 liraglutide; 2381 comparator) Incidence ratio 0.73 (95% CI 0.38−1.41) Linagliptin3 8 5239 (3319 linagliptin; 1920 comparator) Hazard ratio 0.34 (95% CI 0.16−0.70) Saxagliptin4 8 4607 (3356 saxagliptin; 1251 comparator) Relative risk 0.43 (95% CI 0.23−0.80) Sitagliptin5 25 14,611 (7726 sitagliptin; 6885 comparator) Incidence ratio 0.83 (95% CI 0.53−1.30) GLP-1 receptor agonists6 37* 15,398 (8619 GLP-1 RA; 6779 comparator) Odds ratio 0.78 (95% CI 0.54−1.13) DPP-4 inhibitors7 70† 41,959 Odds ratio 0.71 (95% CI 0.59−0.86) *25 trials reported ≥1 CV event and were included in the main analysis. †63 trials reported ≥1 CV event and were included in the main analysis. 1. Ratner R, et al. Cardiovasc Diabetol. 2011;10:22. 2. Marso SP, et al. Diab Vasc Dis Res. 2011;8:237-240. 3. Johansen OE, et al. Cardiovasc Diabetol. 2012;11:3. 4. Frederich R, et al. Postgrad Med. 2010;122:16-27. 5. Engel SS, et al. Cardiovasc Diabetol. 2013;12:3. 6. Monami M, et al. Diabetes Obes Metab. 2014;16:38-47. 7. Monami M, et al. Diabetes Obes Metab. 2013;15:112-120. CV Outcomes Trials with Incretin-Based Therapies Trial Name Estimated Primary Completion Date Comparators Population Saxagliptin vs placebo T2DM with history of CVD or CV risk Completed EXAMINE2 Alogliptin vs placebo T2DM with recent ACS Completed TECOS3 Sitagliptin vs placebo T2DM with preexisting CVD Dec 2014 ELIXA4 Lixisenatide vs placebo T2DM with ACS Jan 2015 LEADER5 Liraglutide vs placebo T2DM with CV risk Oct 2015 EXSCEL6 Exenatide ER vs placebo T2DM Dec 2017 Linagliptin vs placebo T2DM with CV risk Jan 2018 Linagliptin vs glimepiride T2DM with CV risk Sep 2018 SAVOR-TIMI 531 CARMELINA7 CAROLINA8 Abbreviations: ACS, acute coronary syndrome; CV, cardiovascular; CVD, cardiovascular disease. 1. http://www.clinicaltrials.gov/ct2/show/NCT01107886. 2. http://www.clinicaltrials.gov/ct2/show/NCT00968708. 3. http://www.clinicaltrials.gov/ct2/show/NCT00790205. 4. http://www.clinicaltrials.gov/ct2/show/NCT01147250. 5. http://www.clinicaltrials.gov/ct2/show/NCT01179048. 6. http://www.clinicaltrials.gov/ct2/show/NCT01144338. 7. http://www.clinicaltrials.gov/ct2/show/NCT01897532. 8. http://www.clinicaltrials.gov/ct2/show/NCT01243424. SAVOR Trial: Study Design 16,492 T2DM patients with established CVD or multiple risk factors Randomized 1:1 Saxagliptin 5 mg/d (2.5 mg/d if eGFR ≤50 mL/min) Other therapy at the physician’s discretion Double-blind Placebo Primary endpoint: composite endpoint of CV death, non-fatal MI, or non-fatal ischemic stroke Scirica BM, et al. N Engl J Med. 2013 3;369:1317-1326. SAVOR Trial: Primary Endpoint HR 1.00 (95% CI 0.80−1.12) P <.001 (noninferiority) P = .99 (superiority) Scirica BM, et al. N Engl J Med. 2013 3;369:1317-1326. EXAMINE Trial: Study Design 5380 T2DM patients with recent ACS Randomized 1:1 Alogliptin (5 mg , 12.5 mg, or 6.25 mg once daily based on renal function) Plus standard of care Double-blind Placebo Primary endpoint: composite endpoint CV death, nonfatal Ml, or nonfatal stroke White WB, et al. N Engl J Med. 2013;369:1327-1335. EXAMINE Trial: Primary Endpoint HR 0.96 (95% CI ≤1.16) P <.001 (noninferiority) P = .32 (superiority) Placebo (n = 2679) White WB, et al. N Engl J Med. 2013;369:1327-1335. Study Design: SAVOR and EXAMINE SAVOR (N = 16,492) EXAMINE (N = 5380) Planned duration Event-driven until the occurrence of 1040 primary events Event driven with interim analyses after 80, 100, 125, 150, 550, 600, and 650 events (~5 yrs) Analysis Noninferiority/superiority Noninferiority/superiority Prevention 1° or 2° 2° Primary outcomes Efficacy and safety: time to confirmed CV event (composite of death, nonfatal MI, nonfatal ischemic stroke) Time to CV event (composite of CV death, nonfatal MI, nonfatal stroke) Secondary outcomes Time to first occurrence of primary outcome + hospitalization for HF, unstable angina, or coronary revascularization All-cause mortality Time to occurrence of any event in the secondary MACE composite of CV death, nonfatal MI, nonfatal stroke, and urgent revascularization for unstable angina Key inclusion ≥40 years, A1C ≥6.5% and ≤12.5% within 6 months Pre-existing CVD or high risk for CV or multiple CV risk factors ≥18 years, A1C 6.5%−11.0% while receiving monotherapy or combination antihyperglycemic therapy, or from 7.0%−11.0% if the regimen includes insulin Key exclusion Acute vascular event <2 months prior to randomization Treatment with DPP-4i or GLP-1 RA within 6 months Type 1 diabetes Treatment with GLP-1 RA at screening Treatment with DPP-4i within 3 months of screening or more than 14 days total ClinicalTrials.gov. 2013. Accessed 12/31/13 at: http://www.clinicaltrials.gov. 71 Baseline Characteristics: SAVOR and EXAMINE SAVOR Trial1 (N = 16,492) EXAMINE Trial2 (N = 5380) Saxagliptin (n = 8280) Mean age: 65 y Mean HbA1c: 8.0% Mean BMI: 31.1 kg/m2 Median duration of diabetes: 10.3 y Alogliptin (n = 2701) Mean age: 61 y Mean HbA1c: 8.0% Mean BMI: 28.7 kg/m2 Median duration of diabetes: 7.1 y Placebo (n = 8212) Mean age: 65 y Mean HbA1c: 8.0% Mean BMI: 31.2 kg/m2 Median duration of diabetes: 10.3 y Placebo (n = 2679) Mean age: 61 y Mean HbA1c: 8.0% Mean BMI: 28.7 kg/m2 Median duration of diabetes: 7.3 y 1. Scirica BM, et al. N Engl J Med. 2013 3;369:1317-1326. 2. White WB, et al. N Engl J Med. 2013;369:1327-1335. 72 GLP-1 Receptor Agonists and DPP-4 Inhibitors Effects on the Renally Impaired Dose Titration for Renally Impaired Patients Recommended Dose Exenatide1 5 mcg twice daily; increase to 10 mcg based on clinical response Exenatide qwk2 2 mg once weekly Dose Adjustment for Renal Impairment Moderate: Use with caution when initiating or escalating doses Severe/ESRD: Not recommended Moderate: Use with caution Severe/ESRD: Not recommended Liraglutide3 0.6 mg once daily for 1 week, then 1.2 mg; can be increased to 1.8 mg Aloglitpin4 25 mg once daily Moderate: 12.5 mg once daily Severe/ESRD: 6.25 mg once daily Linagliptin5 5 mg once daily No dose adjustment recommended for renal impairment Saxagliptin6 2.5 mg or 5 mg once daily Sitagliptin7 100 mg once daily Vildagliptin8 50 mg twice daily as monotherapy; 50 mg once daily in combination with SU Use with caution; no dose adjustment recommended for renal impairment Moderate or severe/ESRD: 2.5 mg once daily Moderate: 50 mg once daily Severe/ESRD: 25 mg once daily Moderate or severe/ESRD: 50 mg once daily 1. Exenatide Prescribing Information. 2. Exenatide QW Prescribing Information. 3. Liraglutide Prescribing Information. 4. Alogliptin Prescribing Information. 5. Linaglitpin Prescribing Information. 6. Saxagliptin Prescribing Information. 7. Sitagliptin Prescribing Information. 8. Vildagliptin Summary of Product Characteristics. Linagliptin Added to Insulin: Renal Function vs Linagliptin’s Efficacy at Week 24 • In a prespecified subgroup analysis, there was no significant interaction according to patient renal function category (P = .5784) • The study had a high proportion of patients with renal impairment – Mild (EGFR 60 to <90 mL/min): 46.3% linagliptin, 44.9% placebo – Moderate (EGFR 30 to <60 mL/min): 9.4% linagliptin, 10.8% placebo – Severe to end-stage (EGFR <30 mL/min): 0.5% linagliptin, 0.6% placebo Abbreviation: EGFR, estimated glomerular filtration rate. Yki-Järvinen H, et al. Diabetes Care. 2013;36:3875-3881. GLP-1 Receptor Agonists and DPP-4 Inhibitors Safety and Tolerability Adverse Effects of GLP-1 Agonists and DPP-4 Inhibitors Nausea/ Vomiting Diarrhea Hypoglycemia Pancreatitis + Rare Exenatide1,2 ++++ Liraglutide3 +++ + + Rare Exenatide qwk4 ++ + + Rare Alogliptin5 + Rare Linagliptin6 + Rare Sitagliptin7,8 + Rare + Rare Saxagliptin9 +/- • In the first long-term clinical trials (EXAMINE and SAVOR), there was no difference in the rate of pancreatitis between the active drug and placebo10,11 1. Klonoff DC, et al. Curr Med Res Opin. 2008;24:275-286. 2. Kolterman OG, et al. J Clin Endocrinol Metab. 2003;88: 30823089. 3. Garber A, et al. Lancet. 2009;373:473-481. 4. Exenatide QW Prescribing Information. 5. Alogliptin Prescribing Information. 6. Linagliptin Prescribing Information. 7. Hanefeld M, et al. Curr Med Res Opin. 2007;23:1329-1339. 8. Sitagliptin Prescribing Information. 9. Rosenstock J, et al. Curr Med Res Opin. 2009;25:2401-2411. 10. White WB, et al. N Engl J Med. 2013;369:1327-1335. 11. Scirica BM, et al. N Engl J Med. 2013 3;369:1317-1326. Summary GLP-1 Agonists and DPP-4 Inhibitors Incretin-Based Therapy in T2DM Meta-analysis Achieved HbA1c <7% (risk ratio) HbA1c reduction (weighted mean difference in change in HbA1c percentage) FPG level, mg/dL (weighted mean difference in change from baseline) Weight, kg (weighted mean difference in change from baseline) GLP-1 Analogs vs Placebo*† DPP-4 Inhibitors vs Placebo* 4.19† (3.17 to 5.53) 2.47 (2.14 to 2.84) -0.97% (-1.13% to -0.81%) -0.74% (-0.85% to -0.62%) -27 (-33 to -21) -18 (-22 to -14) -2.37 (-3.95 to -0.78) 0.48 (0.30 to 0.66) *The values in parentheses represent 95% CIs. †This value represents only exenatide vs placebo. Amori RE, et al. JAMA. 2007;298:194-206. Slide courtesy of Dr. Jaime A. Davidson. Incretin-Based Therapy in T2DM Meta-analysis Mean Change from Baseline GLP-1 Receptor Agonists DPP-4 Inhibitors -1.10% to -1.59% -0.60% to -1.06% FPG (mg/dL) -20.90 to -32.79 -13.15 to -28.29 Weight (kg) -2.03 to -2.41 -0.16 to -0.64 HbA1c • Meta-analysis – GLP-1 receptor agonists ■ 19 studies with exenatide BID, 7 studies with exenatide qwk, 11 studies with liraglutide – DPP-4 inhibitors ■ 5 studies with alogliptin, 9 studies with linagliptin, 7 studies with saxagliptin, 23 studies with sitagliptin, 6 studies with vildagliptin Aroda VR, et al. Clin Ther. 2012;34:1247-1258.e22. Summary: DPP-4 Inhibitors and GLP-1 Receptor Agonists DPP-4 Inhibitors GLP-1 Receptor Agonists 0.5%−1.0% 0.8%−1.9% Orally Injected Neutral Weight loss Headache, infection Nausea, vomiting Hypersensitivity/ allergic reactions Symptoms of pancreatitis Low risk of hypoglycemia?1,2 Yes Yes Gastrointestinal adverse events?1,2 No Yes Improve postprandial glucose levels?1,2 Yes Yes* Included in ADA/EASD algorithm?1 Yes Yes Included in AACE algorithm?4 Yes Yes Characteristic Expected HbA1c decrease1,2 How administered1 Weight effect1,2 Common adverse events1-3 Rare serious adverse events1-3 *Greater effect for this class. Abbreviations: AACE, American Association of Clinical Endocrinologists; ADA, American Diabetes Association; EASD, European Association for the Study of Diabetes. 1. Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379. 2. Garber AJ, et al. Endocr Pract. 2013;19(suppl 2):1-48. 3. Dicker D. Diabetes Care. 2011;34(suppl 2):S276-S278. 4. Garber AJ, et al. Endocr Pract. 2013;19:327-336. Benefits and Advantages of Incretin-Based Therapies GLP-1 analogs • Lower HbA1c ~0.8%-1.1% from baseline • Promote satiety and weight loss • Beneficial effects on lipids • Beneficial effects on systolic blood pressure DPP-4 inhibitors • Lower HbA1c ~0.4%–0.9% from baseline • Weight neutral (do not promote weight gain) • Once-daily oral therapy – vs once daily, twice daily, or once weekly injections with GLP-1 analogs • Minimal GI side effects Investigational Incretin-Based Therapies • GLP-1 analogs – – – – Albiglutide Lixisenatide Dulaglutide Semaglutide • DPP-4 inhibitors – Vildagliptin (approved in Europe and Latin America) – Omarigliptin (MK3102) – Trelagliptin (SYR-472) ClinicalTrials.gov. 2013. Accessed 12/11/13 at: http://www.clinicaltrials.gov. Conclusion • Incretin-based therapies are welcome additions to treatment of T2DM • Both improve glycemic control • GLP-1 agonists have beneficial effects on lipids, blood pressure, and weight • DPP-4 inhibitors are convenient once-daily oral therapies with a good safety and tolerability profile • The first 2 long-term trials with DPP-4 inhibitors— SAVOR and EXAMINE—showed these therapies to be safe in T2DM patients at a high risk for cardiovascular disease Thank you for your participation. To earn CME/CE credit, please complete the posttest and evaluation. (Click link in the navigation bar above or to the left of the slide presentation.) Your feedback is appreciated and will help us continue to provide you with clinically relevant educational activities that meet your specific needs.