Vibrio - Pathology
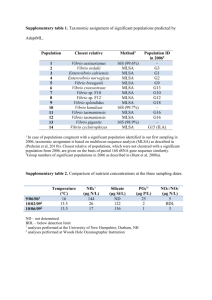
advertisement
Enterobacteriaceae A. General characteristics 1. Pathogenic genera: human colonizers or pathogens 2. Non-pathogenic genera: human colonizers or environmentals 3. Oxidase negative, glucose fermenters, grow on MAC B. Epidemiology 1. Reservoirs a. Inhabit human GI tract b. Inhabit GI tract of other animals c. Environmental organisms d. Zoonotic pathogens (cause disease in animals) e. Only present during disease 2. Transmission a. Endogenous infections from patient’s own strain b. Person to person c. Ingestion of contaminated food or water d. Vector-borne C. Pathogenesis and spectrum of disease 1. Overt pathogens a. Salmonella spp.: GI, bacteremia and extraintestinal infections, enteric fever (typhoid fever) b. Shigella spp.: dysentery c. Yersinia pestis: “black” plague 2. Opportunistic pathogens a. Citrobacter spp., Enterobacter spp., Klebsiella spp., Proteus spp., and Serratia spp. b. can be very pathogenic, but usually only in immunocompromised 3. Eschericia coli a. more pathogenic than opportunists; some strains are overt pathogens TABLE 25-2 D. Laboratory diagnosis 1. Specimen collection, transport, processing a. No special considerations for these organisms 2. Direct detection methods a. No specific procedures for routine enterics 3. Culture and identification a. Media i. BAP, CAP, Mac all support growth large gray smooth on BAP, CAP TABLE 25-3 ii. CIN agar for selection of Yersinia iii. Hektoen for Salmonella/Shigella iv. MacConkey-Sorbitol: E. coli O157 can’t ferment sorbitol Gram stain of enteric Gram-negative rods http://www.nirgal.net/life_nano.html D. Laboratory diagnosis 3. Culture and identification b. Colony appearance i. Swarming of Proteus indole + P. vulgaris, indole – P. mirabilis ii. Mucoid Klebsiella iii. H2S positive Salmonella on Hektoen iv. Serratia makes a red pigment v. Yersinia red center with clear border on CIN c. Identification i. API strips, automated systems ii. TSI slants iii. Salmonella antisera Enteric gram-negative rods on BAP E. coli Klebsiella sp. http://www.vetmed.wisc.edu/pbs/courses/bact/labmanual/c4klebsiella.html Enteric gram-negative rods on BAP Proteus sp. http://www.vetmed.wisc.edu/pbs/courses/bact/labmanual/c4klebsiella.html Identification of Salmonella and Shigella TSI slant Hektoen agar http://www.msu.edu/course/fsc/441/resulex14.html CIN agar for the recovery of Yersinia sp. http://www.troybio.com/images/Product_Images_BBL/BBL.htm D. Laboratory diagnosis 4. Antimicrobial susceptibility testing and therapy a. Susceptibility is unpredictable, so testing is warranted for extra-intestinal infections b. Treatment of GI disease with antibiotics is controversial Vibrio, Aeromonas, Plesiomonas A. General characteristics 1. Different from enterics: Oxidase-positive, glucoseferm, grow on Mac B. Epidemiology 1. Reservoirs a. Vibrio: brackish or salt water b. Aeromonas: various aquatic environments c. Plesiomonas: fresh water 2. Transmission a. Vibrio: fecal-oral, exposure to contaminated seafood or water b. Aeromonas: exp. to contam food or water; traumatic injury (fish hooks) c. Plesiomonas: exp to contam food or water; exp to reptiles C. Pathogenesis and spectrum of disease 1. V. cholerae a. cholera toxin causes mucosal cells to hypersecrete water and electrolytes b. profuse watery diarrhea, fluid loss, dehydration (ricewater stools: fluid and mucous flecks) c. somatic O1 and O139 are markers for epidemic/pandemic strains; non O1 or O139 do not produce toxin 2. Non-cholerae vibrio a. specific virulence factors undefined b. gastroenteritis from seafood, wound infections, septicemia 3. Aeromonas and Plesiomonas a. virulence factors unclear b. gastroenteritis, wound infections, septicemia D. Laboratory diagnosis 1. Specimen collection, transport, processing a. no unique requirements except that suspected Vibrio should only be transported in Cary-Blair, because glycerol in buffered glycerol saline is toxic to vibrios 2. Direct detection methods a. Vibrios: gnr, slightly curved b. Aeromonas: gnr, straight c. Plesiomonas: gnr, single, pairs, short chains, or long filaments Gram stain of Vibrio sp. http://www2.mf.uni-lj.si/~mil/bakt2/bakt2.htm D. Laboratory diagnosis 3. Culture and identification a. Media i. all grow on blood and Mac ii. may be LFs or NLFs iii. Thiosulfate citrate bile salts sucrose (TCBS); selective media for vibrio: ferments sucrose and makes yellow colonies on blue-green plate. b. Colony appearance i. look like gnrs, Aeromonas may be beta-heme ii. all are OXIDASE-POSITIVE; we look for ox+ positive that are not Pseudomonas c. Identification i. API strips or similar TCBS agar for the recovery of Vibrio sp. http://idsc.nih.go.jp/idwr/kansen/k01_g1/k01_12/k01_12.html D. Laboratory diagnosis 4. Antimicrobial susceptibility testing and therapy a. Tetracycline or doxy are first line drugs for cholera, but fluid management for this and other orgs in main therapy b. no standardized testing methods for any of these