Team Care at The Cleveland Clinic
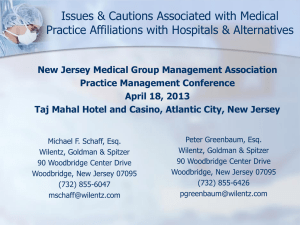
advertisement
Team Care at The Cleveland Clinic Kevin D. Hopkins, MD Section Head-Family Medicine Strongsville Family Health Center Cleveland Clinic Agenda • Planning for Change • Program Overview & Structure • Outcomes • Taking it to “the next level” It’s All About Increasing Value The Right Thing to Do in Any Payment Methodology Quality Value = Cost • • • Focus on maximizing value delivered to patients Explore strategies that increase value Enter into contracts that share in value created Introduction to Value-Based Operations: The Industry is Changing Cost • Fragmented • Fee-for-service VolumeDriven Healthcare • Connected • Bundled • Accountable VALUEDriven Healthcare Quality Managing Population Health Today: The FFS model Tomorrow: The Value-Based model Care of the individual Care of a population Payment for each service we provide Payment based on the quality and efficiency of our care Predictability! Uncertainty and risk! “Care Transformation” is Critical • Transform clinical operations • Assemble the right care team • Reward added value with sustainable payment models • Support with the correct Analytics 6 17 Patient-Centered Medical Home The Key to Success “Patient-centered medical home (PCMH) is a model of care where patients have a direct relationship with a provider who coordinates a cooperative team of healthcare professionals, takes collective responsibility for the care provided to the patient and arranges for appropriate care with other qualified providers as needed.” NCQA There’s No Place Like a “Medical Home” Patient Engagement Treatment of Patient as a “Whole” Comprehensive and Coordinated Care Enhanced Access Safety and Quality Physician Directed Practice Payment for Added Value Transform Clinical Operations Patient follow-up & engagement Proactive, targeted outreach Engage other providers Enhanced access Chronic disease management Pre-visit planning Standardized Care Paths The Time Problem Based on various analyses: • Time needed for chronic illness care for 2,500 patients1 • Time needed for preventive care for 2,500 patients2 • Time needed for acute care1 1. Østbye TH, et al. Ann Fam Med. 2005;(3)209–214. 2. Yarnall KS, et al. Am J Pub Health. 2003;93(4)635–641. • 10.6 hours/d • 7.4 hours/d • 4.6 hours/d Assemble the Right Team MD Medical Assistant Patient Care Coordinator Pharmacist Strongsville FHC Background • There are many factors exerting considerable pressure on our healthcare system: - Reimbursement for care is static and uncompensated care is increasing - Increased level of acuity of outpatient office visits - Primary Care Physician utilization rates are 90-95% - Healthcare Reform-ACA provisions Background • Press Ganey data for appointment convenience - 50% “very good” (median: 51%, 90th percentile: 59%) • Leakage - This is lost-opportunity for higher-quality care for the patient, and revenue for the organization. Team Care “Team Care” is a higher-efficiency practice style designed to: • • • • Increase accessibility Improve quality of clinical care Increase patient throughput Improve satisfaction at all levels (physician, employee, and patient) Team Care A “Team Care” model utilizes a teamapproach in caring for patients • Responsibilities are delegated and shared • Each individual in the chain of patient care functions to the highest level of their qualifications. Team Care • • • • Outpatient Visit: Stage 1: Gathering data Stage 2: Physical exam and synthesis of data Stage 3: Medical decision-making Stage 4: Patient education and plan-of-care implementation Team Care Workflow • With a “Team Care” model, the clinical assistant gathers and documents the data. • The clinical assistant: - Takes a competent history - Presents to the physician - Remains in the room with the physician and patient - Completes all documentation of the visit - Implements the treatment plan - Gives patient instructions (AVS), ensures understanding, and completes the visit Medical History Medication Review • Medication refill requests discussed • Allergies • Health Maintenance • Smoking/Substance abuse • Changes to medical/surgical history • Medical History • Reason for visit • Note template is loaded in the progress note • Collect and document the History of Present Illness and ROS Team Care Workflow • With a “Team Care” model, the clinical assistant gathers and documents the data. • The clinical assistant: - Takes a competent history - Presents to physician - Remains in the room with the physician and patient - Completes all documentation of the visit - Implements the treatment plan - Gives patient instructions (AVS), ensures understanding, and completes the visit Team Care Workflow The physician (with the assistant still in the room): • Confirms the history • Performs the physical exam • Makes medical management decisions • Articulates diagnostic/treatment plan Team Care Workflow • The physician leaves the exam room of the completed patient. • Orders pended by the clinical staff are filed by the physician. • The physician signs any prescriptions that are not electronically transmitted. • Physician starts the process with the next patient prepped by the other medical assistant Team Care Workflow • The medical assistant reviews the After Visit Summary with the patient along with any prescriptions or ordered tests. • Patient education is given and reviewed. • The patient is escorted to the appointment desk by the clinical staff. Care Coordination • RN Care Coordinator embedded • Hospital Discharges - DM-2 - CHF - COPD - Pneumonia - MI - CKD Clinical Pharmacist • Referrals for: - Polypharmacy - Medication compliance - Medical literacy Key Metrics • Increase volume of patients seen • Increase efficiency/decrease scheduling wait time • Increase accessibility to quality physician care • Increase patient satisfaction • Improve quality of patient care • Increase clinical employee satisfaction • Increase physician satisfaction Access – Patients Added May 2011 – August 2013 Ramp Up Team Care 140 137 130 130 123 116 113 106 106 104 97 100 101 98 94 85 83 80 72 66 53 100 99 66 Missing MA 32 30 24 32 Patient Satisfaction 20112013 (Q1) Sum of 2011 94 92 93 93 Sum of 2013 97 96 96 95 Sum of 2012 95 94 94 95 94 93 93 91 88 Care Provider CP respect for Likelihood of Patients' questions* recommending confidence in CP CP 88 Rating of CP* Time CP spent with patient Total Visits Normalized per Clinical FTE 2010-2013 (2013 Projection) 6000 4946 4761 5000 4382 4000 3894 3881 4058 3984 3633 3000 2000 1000 0 Total Visits Total Visits Hopkins Kaesgens WRVU’s normalized for Clinical FTE 2010-2013 (2013 Estimation) Sum of 2010 Norm Sum of 2012 Norm 5608 Sum of 2011 Norm Sum of 2013 Norm Est. 6649 6008 5074 4791 4869 4968 4970 WRVU's WRVU's Hopkins Kaesgens Productivity WRVU's 2010-2011-2012 619 576 570 569 554 536 526 519 539 522 510 505 494 488 WRVU's 469 466 432 406 460 488 474 470 440 438 419 489 414 400 424 414 407 2010 2011 383 369 371 370 2012 366 350 336 328 319 303 283 269 252 219 Month *Days not worked not considered Outcomes Quality Indicators Chosen for Improvement Q1 2011 Q2 2011 Q3 2011 Q4 2011 Q1 2012 Q2 2012 Q3 2012 Blood Pressure Control 74% 76% 81% 79% 79% 78% 78% A1c Diabetics 96% 96% 98% 96% 98% 97% 99% Diabetes Screening 89% 90% 90% 90% 91% 91% 93% Hyperlipidemia Screening 79% 80% 80% 74% 77% 79% 81% Mammogra m Completed 77% 78% 78% 75% 78% 79% 78% Team Care started 2Q 2011 Sensitivity Analysis Potential Financial Impact Per Day 6 8 10 1,338 1,784 2,230 Revenue $156,546 $219,024 $273,780 Expenses $61,992 $61,992 $61,992 EBIDA $94,554 $157,032 $211,788 Annual Add BIO Cards Bio Cards so Patients can put a face with a name and to promote our Team! Taking It to the Next Level • Expand Team Care at Strongsville to include 6 Family Medicine Physicians - 6 MA/MA/MD Teams - 1 more in 2014 • Transform 1 in 4 primary care practices to TeamCare to increase volume; fund care coordination and PreVisit MAs • Care coordinators and PreVisit MAs (pre-visit planning, health maintenance and wellness) support all providers