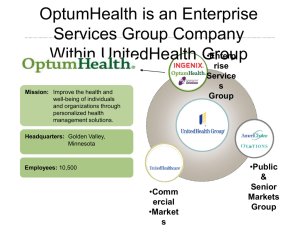
QUEST Integration Training & Education
for Medical Providers
Who is UnitedHealthcare?
Introductions
In Hawaii since 1992
Medicare and Commercial products
QExA program began in February 2009
QUEST program began in July 2012
QUEST Integration program begins January 2015
Over 180 employees statewide
Office: 1132 Bishop Street in Honolulu, Suite 400
Future office opening in Hilo in Jan 2015
6,500 Medicare Members on Oahu
41,000+ QUEST Expanded Access members statewide
14,000+ QUEST members statewide
United Health Group, Inc. and
its partners in Hawaii
UnitedHealthcare Community and State: Includes Medicaid, TANF, CHIP,
ABD, long term care, Medicare Dual SNP programs
UnitedHealthcare Medicare and Retirement: Includes Medicare and
retirement plans
UnitedHealthcare Employer and Individual: Includes commercial group and
individual plans
UnitedHealthcare Military and Veterans: Tricare Program
OptumHealth: Includes OptumHealth Care Solutions, Optum Behavioral
Health, Nurseline
OptumInsight: Provides consulting, health information systems and data
management
OptumRx: pharmacy benefit manager
Logisticare: transportation services
Important Highlights
• UnitedHealthcare is accredited by the National Committee
for Quality Assurance (NCQA) for its Medicaid programs
• Local Member/Provider Call Center for Hawaii Medicare
and Medicaid programs
• Local Provider Services Team, lead by Julie Cooper,
Director of Network Strategy & Relationship Building
• Medical Director, Ronald Fujimoto, DO
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Learning Objectives
Today’s topics will leave you with an understanding of the:
• Updates and changes at UHC
• Overview of QUEST Integration
• Health Plan Roles and Responsibilities
•
•
•
•
•
•
Health Plan Accreditation
Our Commitment to you
Care/Case Management Model
Roles of UHC Support Team
Quality Initiatives
Disease Management
• Provider Roles and Responsibilities
•
•
•
•
•
•
PCP Role and PCP Assignment
EPSDT
Access to Care Standards
Provider Complaint, Grievance and Appeals
Process
Regulatory Requirements
Credentialing and ReCredentialing
•
•
•
•
•
•
•
•
Fraud, Waste and Abuse
Member Rights and Responsibilities
Cultural Competency
Member Grievance and Appeals
Referrals, Notifications and Prior
Authorizations
Billing/Claims Submission and
Reimbursements
Balance Billing
Reporting and Record Keeping
• Member Medical Records
• Reporting and Data Collection
• How to Access Program Services
• Provider Resources
•
•
•
•
Clinical Practice Guidelines
External Resources
Provider Websites
UHC Contact information
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
UnitedHealthcare
Community Plan QUEST Integration
Program
Member Enrollment and Eligibility
•
Program offered by the State of Hawaii Department of Human Services and
administered by the Med-QUEST Division.
•
The QUEST Integration replaces the QExA program (serving the Medicaid
Aged (Age 65 and over), Blind and Disabled (all ages) population in a
mandatory managed care system) and the QUEST program (covering qualified
individuals who are not aged, blind or disabled) effective 1/1/15.
•
Enrollment is determined by the DHS
– Eligibility status may change from month to month and member may be retro enrolled into or
dis-enrolled out of the UHC QUEST Integration program
• To ensure timely reimbursement, Providers must check Member eligibility:
– When scheduling each appointment
– On the day of each appointment
– At the time of claim(s) submission
• You may check member eligibility (including TPL carrier name) via:
– www.unitedhealthcareonline.com
– https://hiweb.statemediciad.us/home.asp
– Our local Call Center toll free at 1-888-980-8728
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Health Plan Roles and
Responsibilities
Health Plan Roles and Responsibilities
• We will comply with all contractual requirements with DHS, which includes
the following:
• We will not prohibit healthcare professionals, acting within the lawful scope of his or her
license or certification under applicable State law, solely on that license or certification
from advising their patients about their medical conditions or diseases and the care or
treatment required, regardless of whether the care or treatment is a covered benefit or
whether or not the services or benefits are provided by United.
• We will not discriminate against providers serving high-risk populations or those that
specialize in conditions requiring costly treatments.
• We will not control, nor direct the rendering of health care services or prohibit a provider
from discussing treatment or non-treatment options with members, including any
alternative treatment that may be self-administered as well as any information the
member needs in order to decide among all relevant treatment options. We will educate
and encourage our members to:
• Exercise their right to participate in decisions regarding his or her healthcare, including the
right to refuse treatment and to express preferences about future treatment
• Receive from their providers the full range of medical advice and counseling appropriate for
their condition
Health Plan Roles and Responsibilities
(Continued)
• We will not include in our network any providers when a person with an ownership or
controlling interest in the provider (an owner including the provider himself or herself),
or an agent or managing employee of the provider, has been excluded from
participation by the Department of Health and Human Services (DHHS), Office of
Inspector General (OIG) under Section 1128 of the Social Security Act, or has been
excluded by the DHS from participating in the Hawaii Medicaid program.
• We will immediately terminate any provider(s) or affiliated provider(s) whose owners,
agents, or managing employees are found to be excluded on the State or Federal
exclusion list(s).
• We will report application denials or terminations to the DHS where individuals were on
the exclusions list, including denial of credentialing for fraud-related concerns, as they
occur.
• We will immediately comply if the DHS requires that it remove a provider from its
network if:
• The provider fails to meet or violates any State or Federal laws, rules, or regulations; or
• The provider’s performance is deemed inadequate by the State based upon accepted
community or professional standards.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Health Plan Roles and Responsibilities
(Continued)
• We will keep providers informed of any program benefit updates and changes
via the following methods.
•
•
•
•
Special Written Communication
Provider Newsletters/Bulletins
Bi-Annual Provider Education & Training Sessions
One-on-One Training & Education Sessions (at the time of contract execution and
as identified by the Health Plan and/or Provider)
• Provider Conferences
• Provider Portal: www.UHCCommunityPlan.com/health-professionals
• We will maintain a Provider and Member Grievance & Appeals Program.
• We will maintain an adequate and comprehensive provider network.
• We will monitor PCP assignment reports, network reports, grievance and
appeals reports and feedback from providers, UHC staff and external partners to
determine necessary network adjustments and/or network expansion initiatives.
• We will process claims timely and accurately
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Network
• Our network consists of health care providers of all types and
specialties in the State of Hawaii to include:
–
–
–
–
–
–
–
–
–
–
Primary Care Physicians
Specialists
Hospitals
Skilled Nursing Facilities
Hospice Providers
Home and Community Based Service (HCBS) providers
Community Care Foster Family Home (CCFFH)
Behavioral Health providers
Transportation Providers
Durable Medical Equipment
Network expansion suggestions?
Call our local Provider Services Team toll free at 1-888-980-8728
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
UHC Support Team
• Local Member Services Team
• Local Provider Relations Team
• Local Claim Research Team
• Local Utilization Management Team
– Acute Care
– Home & Community Based Services (HCBS)
• Local Care Coordination Team
–
–
–
–
–
Service Coordinators (Field and Telephonic)
Clinical Managers
Community Case Management Agencies
Behavioral Health Care Advocates
Service Coordinator Assistants
Quality Initiatives
•
UHC's Medicaid Quality Improvement (QI) Program
encompasses all quality improvement activities within the
health plan, including programs / standards that focus on:
–
–
–
•
Clinical quality and excellence
Access and affordability
Customer service and operational excellence
Hawaii-specific and National Quality Committees
–
Develop and monitor Quality Management program activities
such as Clinical Practice Guidelines.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Disease Management
• Provide proactive coordination of care for:
– Asthma
– Congestive Heart Failure (CHF)
– Diabetes
• Practitioner and member compliance with HbA1C testing and
Diabetic Retinal Eye Exams
– Obesity
• Body Mass Index (BMI) documented during outpatient office visits
• Practitioner compliance in documenting height and weight as a
baseline in determining the need for interventions for maintaining
optimal weight.
– Poly-Substance Abuse
– Hypertension
– High Risk Pregnancy
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Provider Roles and
Responsibilities
Provider Roles and Responsibilities
– Administrative/Contractual
• Comply with all applicable federal, state, and local laws
• Comply with the Health Insurance Portability and Accountability Act of 1996
(HIPAA) regulations
• Comply with the Medicare and Medicaid Anti-Fraud Act and the State
Medicaid Fraud Act
• Re-credentialing Requirements (every 3 years)
• Provide an updated Provider Disclosure Form (Form in the packet)
– At the time of initial credentialing
– Upon execution of a provider contract
– At the time of recredentialing
– Within 35 days after any change in ownership of the disclosing entity
information
– Upon request from the United or the DHS
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Roles and Responsibilities (continued)
– Member-Related
• Verify member eligibility
• Accept new members for treatment unless a waiver has been obtained from
the Plan
• Not intentionally segregate members in any way from other persons
receiving services, except for health and safety reasons
• Deliver services to members without regard to race, color, creed, ancestry,
sex, including gender identity or expression, sexual orientation, religion,
health status, income status, or physical or mental disability
• Offers hours of operation that are no less than the hours of operation offered
to commercial members or comparable to hours offered to members under
Medicaid fee-for-service, if the provider has no commercial members
• Assist members in accessing interpreting and auxiliary services by
contacting the Health Plan toll free at 1-888-980-8728 or TTY: 711 (for the
hearing impaired) on the availability of these services
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Roles and Responsibilities (Continued)
– Reporting
–
–
–
–
Submit claims in a timely and complete manner
Maintain member medical records and other record keeping systems
Report any known or suspected cases of fraud, waste and abuse
Report all cases of suspected child abuse to the Child Protective Services
Section of the DHS such as:
–
–
–
–
–
–
–
–
Substantial or multiple skin bruising or any other internal bleeding
Any injury to skin causing substantial bleeding
Malnutrition
Failure to thrive
Burn or burns
Poisoning
Fracture of any bone
Subdural hematoma, etc.
Note: To make a report call the Child Protective Services 24 hours at:
• Oahu: 808-832-5300
• Neighbor Islands: 1-800-494-3991
Or, visit: http://humanservices.hawaii.gov/ssd/files/2013/01/MANDATED-REPORTER-HANDBOOK.pdf
19
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Roles and Responsibilities (Continued)
• Report all suspected dependent adult abuse to the Adult Protective Services
Section of the DHS such as:
• Physical Abuse: non-accidental injury, pain, or impairment such as from hitting,
slapping, improper physical restraint or poisoning.
• Psychological Abuse: threats, insults, harassment, humiliation, intimidation, or other
means that profoundly confuse or frighten the vulnerable adult.
• Sexual Abuse: sexual contact or conduct including pornographic photographing without
consent.
• Financial Exploitation: wrongful taking, withholding, appropriation, or use of the adult’s
money, real property, or personal property.
• Caregiver Neglect: failure to provide adequate food, shelter, clothing, timely health
care, personal hygiene, supervision, protection from abandonment or an assumed, legal
or contractual caregiver.
• Self-neglect: failure to care for one’s self thereby exposing one’s self to a condition that
poses an immediate risk of health or serious physical harm.
Note: To make a report, call the office of Adult Protective Service at 808-832-5115, between
7:45 AM and 4:30 PM (HST), Monday through Friday, except state holidays
Or, visit: http://humanservices.hawaii.gov/ssd/files/2013/01/APS-Guidelines.pdf
20
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Primary Care Provider (PCP)
Role
• PCPs play a central role in the member’s care.
Some responsibilities include:
– Supervise, coordinate and provide all primary care
– Conduct face-to-face initial and ongoing assessments
– Collaborate with member’s Service Coordinator or Care Manager
– Coordinate and initiate referrals for specialty care (for both in-network and
out-of-network)
– Coordinate and initiate prior authorization requests for out-of-network
providers
– When appropriate, enroll, provide appropriate forms or conduct screening
for special programs (e.g. VFC program, EPSDT program, etc.)
– Follow Timely Access to Care Standards
– Follow medical record documentation and maintenance requirements
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
PCP Assignment
• All Members must select a PCP
• Members with QUEST Integration coverage only must select an InNetwork PCP within 10 calendar days of their enrollment otherwise they
will be auto assigned a PCP
• Members with other medical coverage that is primary to QUEST
Integration can choose an In-Network or Out-of-Network PCP
– Members have 10 calendar days to choose an In-Network PCP
– Members who elects to have an Out-of-Network PCP will have a “PCP Not
Selected” indicator on their QUEST Integration membership ID (we will work
with the provider to join our network)
• Members can contact Member Services for assistance with PCP
selection or assignment toll free at: 1-888-980-8728 or TTY: 711 for the
hearing impaired
• Network PCPs are sent a monthly Member Rosters for those members
that have chosen a UHC Network PCP
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Early Periodic Screening and
Diagnostic Testing (EPSDT)
• Federally mandated program
•
– Provides preventive and comprehensive health services
for Medicaid-eligible individuals under age 21
– Primary goal is to offer prevention, early diagnosis and
medically necessary treatment of conditions
• EPSDT Services include:
–
–
–
–
–
–
Comprehensive EPSDT Screenings from newborn
through age 20
Regular dental services every 6 months from age 12
months through age 20
Documentation/Reporting
Use DHS EPSDT Exam form 8015 and 8016
By PCP/other providers
Keep results of screenings or tests in child’s medical
record
• Forms must be complete and accurate for State
reporting, data collection and claims processing
–
–
Original signed EPSDT form must be attached to
each corresponding claim form to ensure payment
The modifier field in the claim form must have “EP”
Clearly documenting the following on
the EPSDT forms will decrease
medical record requests by UHC:
•
•
•
•
Height, Weight, BMI, BMI%
Immunizations given & status
Blood lead screening
Medicaid ID#
•
Contact XEROX State Healthcare
(formerly ACS) toll free at 808-9525570 (Oahu) or 1-800-235-4378 for
additional EPSDT forms
•
Instructions regarding EPSDT forms
can be found on the back of the form;
for more information about the
EPSDT can be found in the MedQUEST Provider Manual, Chapter-5
at: www.med-quest.us
•
For questions, call Evangeline
Apacible-Rivera, RN, EPSDT
Coordinator at 808-275-9216
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Early Periodic Screening and
Diagnostic Testing (EPSDT) (continued)
Screening
Age
Periodicity
Schedule**
Screening Age
Periodicity
Schedule**
14 days
1 visit
1 month
1 visit
3-5 years old
3 visits*
2 months
1 visit
6-9 years old
2 visits*
4 months
1 visit
10-14 years old
3 visits*
6 months
1 visit
15-18 years old
2 visits*
9 months
1 visit
12 months
1 visit
19-20 years old
1 visit
15 months
1 visit
18 months
1 visit
24 months
1 visit
*Visits must be approximately a year apart
**Center for Medicaid Services (CMS)
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
NurseLine and Nurse Chat Services
•Available to UnitedHealthcare QUEST Integration Members 24
Hours, 7 days a week
•Nurseline can help with minor injuries, common illnesses, self-care
tips and treatment options, recert diagnoses and chronic conditions
and much more
• Members may access the Nurseline by calling toll free at 1-888-9808728 or TTY: 711 (for the hearing impaired)
•Members may access the Nurse Chat at: www.myuhc.com
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Compliance with ADA
Providers must comply with the Americans with Disability Act
(ADA) and must assist members in accessing services such as:
– Oral interpreter services to ALL individuals with limited English proficiency
– Sign language interpreter and TTY/TDD services at no cost to the
individuals
– Auxiliary Aids
• Written translation services is also available to our members
• Providers must contact UHCCP by calling toll free at 1-888-9808728 or TTY: 711 (for the hearing impaired) for assistance in
accessing all of the services listed above
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Access to Care Standards
• Providers are required to comply with appointment and wait time standards as
follows:
• Quarterly accessibility member and provider telephone surveys will be conducted
to document provider compliance with Contractual and State requirements
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Referrals, Notifications and
Prior Authorizations
Notifications
For Non-Emergent (Medical and Behavioral Health) Facility
Admissions notify us:
• At or prior to admission
• When we are the secondary payer
• When the primary insurer’s benefits exhaust
• When a member is retro-enrolled into our plan
• When the level of care changes, e.g. to sub-acute
Notifications for services through the Emergency Room:
• When the member enters the into the Emergency Room at the time of each
episode (regardless of the number of episodes per day)
•When the member is placed in a Observation status within the ER setting at
the time of each episode
•When the member is admitted into the Hospital (within in 48 hours)
•Notifications must be faxed to 1-800-267-8328 or online at
https://www.unitedhealthcareonline.com
Referrals
• Referrals to In-Network Providers:
– PCP may call or fax a referral directly to an in-network provider (no form
required and providers do not have to ask the Plan for permission).
• Referrals to Out-of-Network Providers:
– PCP must obtain authorization from the Plan for referrals to out-of-network
providers. A prior authorization request form must be completed and faxed to
1-800-267-8328. You may also submit an electronic request through our
website at: https://www.unitedhealthcareonline.com
• No Referrals Required:
– For family planning providers or women’s routine and preventive health care
services.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Prior Authorization
• Prior Authorizations:
– Refer to the Notification and Prior Authorization Quick Reference Guide for a
list of services that require notification and/or prior authorization
– Request Form must be complete or the form will be returned
• Include diagnosis codes, procedure codes and clinical notes
• Rendering provider name on the authorization form must match the
contracted business name
– Follow instructions on the form
• An urgent fax should be submitted with a maximum of 3 requests per
fax transmission
• Prior Authorization Request Form samples are included in today’s
packet, for additional assistance call our local Provider Services staff
at 1-888-980-8728
• Authorizations must be faxed to 1-800-267-8328 or you may submit a
request online at https://www.unitedhealthcareonline.com
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Prior Authorization Reminder
Remember that as of June 1, 2013: Prior Authorization is NOT required for
incontinence supplies within the threshold (maximum limit) specified in the
following table:
Description
Incontinence Disposable
Supplies (Diapers)
Disposable Gloves
HCPC
T4521 through T4535, T4543
A4927
Threshold
(Maximum Limit)
200 pieces per month
1 box per month
Incontinence Disposable Underpads
T4541 & T4542
100 pieces per month
Washable Under-pads
T4540 & T4537
4 units per 180 days
Incontinence Washable
Underwear
T4536
12 pieces per a 12 month
period
• Exception: All incontinence supplies for children under the age of three (3) will still
require a prior authorization from the Health Plan.
32
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Off Island and Out-of-State Transportation
• All transportation services require a Prior Authorization from UnitedHealthcare.
33
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Online Prior Authorization Submission
Process
• You may also submit a Referral, Notification and/ or a Prior Authorization request through the
provider portal at: https://www.unitedhealthcareonline.com
• An online tutorial is available for the online submission process (including status) for your use
• You may also contact Provider Services for assistance on how you may schedule a one-on-one
in-service at 1-888-980-8728
Claim Submission and
Reimbursement
Claims Submission
• Participating physicians/providers must submit claims on the member’s behalf
• Claims filing timeline is one (1) year from the date of service or the receipt date of
the primary payer’s EOB
• Submitting claims online (1500 Billers Only)
– Submit via UnitedHealthcare Online at www.unitedhealthcareonline.com
– Free to participating network providers (single submissions only)
• To register, providers call 1-866-UHC-FAST (1-866-842-3278)
• For batch submissions you can utilize www.eprovidersolutions.com or www.officeally.com
• Using a clearing house or provider own Electronic Medical Record System
– Submission via Electronic Data Interchange (EDI) using a claims clearinghouse (there may be
costs associated, please check with the clearinghouse for details).
– Use Payer ID 87726.
• Paper Claim
– Use a UB04 for facility or hospital claims
– Use a CMS 1500 for physician and ancillary claims
UnitedHealthcare Community Plan
P.O. Box 31362
Salt Lake City, UT 84131-0362
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Claims Reconsideration
& Corrected Claims
• Claims Reconsideration – when a provider feels that the information on
the claim that was denied is correct.
• Claims reconsideration requests must be filed within one (1) year from
the date of service or sixty (60) days from notice of determination for the
claim, whichever is later.
– Claims reconsideration requests must be sent to the Provider dispute Unit (PDU) at:
UnitedHealthcare Community Plan
P.O. Box 31350
Salt Lake City, UT 84131-0350
– Claims reconsideration forms are located online at:
http://www.uhccommunityplan.com/health-professionals/hi.html
• A copy is also included in today’s packet
•
Corrected Claims must be sent to:
UnitedHealthcare Community Plan
P.O. Box 31362
Salt Lake City, UT 84131-0362
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Helpful Billing Tips
• CMS 1500 Forms
–
–
–
–
Provider name on the claim (box 33) must match the contracted business name
Bill for a span of time (max 1 month)
For dual eligible members, bill for gloves on a separate claim
Note correct place of service on claim (box 24b)
• UB Forms
– Include discharge status code (box 17)
– Refer to contract for specific billing requirements
– The ‘XX7’ bill type must be included with corrected claims
• NDC code information
– Required to accompany any claim when billing with HCPCS J codes (340(b)
participating entities are exempt from this requirement)
– Valid units of measure: F2 = International Unit; GR = Gram; ML = Milliliter; UN = Unit
(Each)
– Not valid units of measure: MG and CC
• Corrected claims
– Hard copy corrected claims must have ‘corrected claim’ written at the top of the claim
and all changes circled otherwise claim will be denied as a duplicate
– Electronic corrected claims may be submitted using bill type XX7
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Coordination of Benefits
• Providers must conduct appropriate coordination of benefits to ensure accurate primary
payer source (e.g. employer group health, Medicare Fee For Service/Managed Care, No-Fault,
Worker’s Comp, etc.). QUEST Integration is always the last payer resort. Providers may check
member TPL carrier name and other information via the UnitedHealthcareOnline.com. Use the
table below as a guide for when to submit a secondary claim to UnitedHealthcare.
Reimbursement
• UnitedHealthcare will reimburse for all medically necessary covered
services even if the contract between DHS and UHC is no longer in
effect providing that all of the following criteria have been met:
– The Member was covered at the time of service;
– All applicable UHC policies and procedures have been met; and
– The claim was filed within the 1-year filing timeline
• UnitedHealthcare will recoup or request for a refund from the
provider for any services previously paid as a result of:
– A Member retro-disenrollment from the UHC QUEST Integration plan
– A confirmed fraud, waste and/or abuse case
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Balance Billing of Members
• Provisions of when a provider may or may not bill a Member:
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Provider Inquiries, Grievances
and Appeals
Inquiries, Grievances and Appeals
Definitions
• Inquiry – Is a contact from a provider that questions any specific
aspect of a UnitedHealthcare, subcontractor or provider’s operations,
activities or behavior but does not express dissatisfaction.
• Grievance - An expression of dissatisfaction made by a provider in
regard to Benefits & limitations, eligibility and enrollment of a member
or provider, member issues or plan issues, availability of health
services for a member, delivery of health services or the quality of
service.
• Appeals (including expedited appeals) -A request for review of an
action. Examples include Bundling issues, Fee disputes, Unit
disputes, Retro/Denied Authorization Requests.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Inquiries
• Providers may contact Provider Services at 1-888-980-8728 with
questions related to but are not limited to:
– Contracting process
– Credentialing/Recredentialing process
– Claims process
– Referral, Notification, or Authorization process
– Status of a claim
– Filing a claims reconsideration, grievance or appeal
– How to reach a Service Coordinator
– How to request for an in-service for new office staff, etc.
Provider Grievances
• Grievances related to the decision making or processing of a
health plan appeal must be filed within thirty (30) days from
UnitedHealthcare’s decision.
• All other grievances may be filed at any time after the
dissatisfaction occurred and with no timeframe limitation.
• Grievances must include the provider’s name, address, telephone
number, member name, member ID#, description or explanation of
the grievance.
• To file a Grievance:
– You may call Provider Services toll free at 1-888-980-8728 or,
– Send written requests to (no special form required):
UnitedHealthcare Community Plan
Attention: Appeals Department
P.O. Box 2960, Honolulu, HI 96802
– You may also send an electronic request via email to: HI_AG@UHC.com
Provider Appeals
• Post Services
– Providers have 60 calendar days from the claims reconsideration decision
to file an appeal related to but are not limited to bundling issues, fee
disputes, unit disputes, retrospective and denied authorization requests
• Pre-Service and Concurrent Review Prior Authorization Denials
– Must be processed as a member appeal (see Member Appeals Section)
• Appeals may be submitted via:
– Phone at 1-888-980-8728
– Email at: HI_AG@UHC.com
– Mail at: UnitedHealthcare Community Plan, Attention: Appeals Department, P.O.
Box 2360, Honolulu, HI 96802
• Expedited Appeal
– If waiting up to 30 days to decide an appeal could seriously risk the
member’s life or health, including his/her ability to reach, keep or get back
to maximum function, Provider must call the Plan to request for an
expedited review (see Member Appeals Section)
NEW Local Appeals and Grievances
Department
47
Appeals and Grievances Contact Information
INQUIRY
Medicaid (QUEST and QExA)
Medicare Medical
Medicare Rx
QExA CALL: 1-888-980-8728 Calls to this number are free. Hours
of Operation: 7:45 a.m. to 4:30 p.m. local time, 5 days a week
CALL: 1-866-622-8054 Calls to this number are free.
Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a week
CALL: 1-866-622-8054 Calls to this number are free.
Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a week
Medicaid (QUEST and QExA)
GREIVANCES (Complaints)
Medicare Medical
Medicare Rx
CALL: 1-808-275-9215 Hours of Operation: 7:45 a.m. to 4:30 p.m.
local time, 5 days a week FAX: 1-855-392-0734
CALL: 1-866-622-8054 Calls to this number are free.
Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a week
WRITE: UnitedHealthcare Community Plan
Attention: Appeals Department P.O. Box 2960
Honolulu, HI 96802
For Fast/Expedited Appeals for Medical Care CALL: 1-877-2629203 Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a
week FAX For fast/expedited appeals only: 1-866-373-1081
EMAIL: HI_AG@UHC.com
WRITE: UnitedHealthcare Appeals and Grievances Department
PO Box 6106, MS CA124-0157, Cypress, CA 90630
QUEST CALL: 1-877-512-9357 Calls to this number are free.
Hours of Operation: 7:45 a.m. to 4:30 p.m. local time, 5 days a
week
WEB SITE: www.UHCCommunityPlan.com
CALL: 1-866-622-8054 Calls to this number are free.
Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a week
FAX 1-866-308-6294
For Fast/Expedited Complaints for Part D Prescription Drugs
CALL: 1-800-595-9532 Hours of Operation: 8 a.m. to 8 p.m. local
time, 7 days a week FAX For fast/expedited Part D prescription
drug complaints: 1-866-308-6296
WRITE: UnitedHealthcare Part D Appeal and Grievance
Department PO Box 6106, MS CA124-0197, Cypress, CA 906309948
WEB SITE: www.UHCCommunityPlan.com
APPEALS
Medicaid (QUEST and QExA)
Medicare Medical
Medicare Rx
Standard or Expedited Appeal CALL: 1-808-275-9215 Hours of
Operation: 7:45 a.m. to 4:30 p.m. local time, 5 days a week FAX:
1-855-392-0734
Standard Appeal CALL: 1-866-622-8054 Calls to this number are
free. Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a
week
Standard Appeal CALL: 1-866-622-8054 Calls to this number are
free. Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a
week FAX For standard Part D prescription drug appeals: 1-866308-6294
WRITE: UnitedHealthcare Community Plan
Attention: Appeals Department P.O. Box 2960
Honolulu, HI 96802
For Fast/Expedited Appeals for Medical Care CALL: 1-877-2629203 Hours of Operation: 8 a.m. to 8 p.m. local time, 7 days a
week FAX For fast/expedited appeals only: 1-866-373-1081
EMAIL: HI_AG@UHC.com
WRITE: UnitedHealthcare Appeals and Grievances Department
PO Box 6106, MS CA124-0157, Cypress, CA 90630
WEB SITE: www.UHCCommunityPlan.com
For Fast/Expedited Appeals for Part D Prescription Drugs CALL:
1-800-595-9532 Hours of Operation: 8 a.m. to 8 p.m. local time, 7
days a week FAX For fast/expedited Part D prescription drug
appeals: 1-866-308-6296
WRITE: UnitedHealthcare Part D Appeal and Grievance
Department PO Box 6106, MS CA124-0197, Cypress, CA 906309948
WEB SITE: www.UHCCommunityPlan.com
48
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Member Grievances and
Appeals
Assisting Members
• Providers may assist UHCCP QUEST Integration Members in filing
and/or representing the member in the following:
– Grievances
– Standard Appeals
– Expedited Appeals (upon determination by UHCCP that taking the time for a standard
resolution could seriously jeopardize the member’s life, health or ability to attain, maintain, or
regain maximum function)
– State Administrative Hearings
• An Appointment of Representative (AOR) must be on file with UHCCP in
order for a provider to assist a member in filing a Grievance or
Standard Appeal and/or for representation in a State Administrative
Hearing.
• The next two slides provide a summary on the appeals and grievance
process. Additional/Detailed information is also provided within
Section-14 of the Provider Administrative Guide.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Member Grievances
The following table outlines a summary of the Member Grievance process:
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Member Appeals
• For assistance in filing an appeal, callers may contact the Health Plan via the toll free phone
number listed below.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
State Administrative Hearings
•
The Health Plan’s written response (denial) includes information on how the member, the
member’s provider or other authorized representative, or the legal representative of a deceased
estate may access the State Administrative Hearing process.
•
Members may have a provider, eligibility worker or any other authorized representative to represent
them at the State Administrative Hearing and are advised of these rights via the Member Handbook
•
Standard/Regular Appeals:
– Member has thirty (30) days to request a State Administrative Hearing following the date of the
Health Plan’s adverse decision
– Decision will be made within ninety (90) days from the date of the recorded request
•
Expedited Appeals:
– Member has thirty (30) days to request an Expedited State Administrative Hearing following the
adverse decision
– The State will reach a decision within three (3) business days after the date the member filed
the request with no opportunity for an extension
•
All State Administrative Hearings must be submitted to:
State of Hawaii Department of Human Services
Administrative Appeals Office
P.O. Box 339
Honolulu, HI 96809
Continuation of Benefits During Appeals
and/or Administrative Hearings
• During an appeal or Administrative Hearing, the Health Plan will
continue the member’s benefits if:
– The member requests an extension of benefits
– The appeal or request for State Administrative hearing is filed on or before the later
of the following:
• Within ten (10) days of the Health Plan mailing of the adverse action
• The intended effective date of the Health Plan’s proposed adverse action
– The appeal or request for State Administrative Hearing involves the termination,
suspension or reduction of a previously authorized course of treatment;
– The services were ordered by an authorized provider; and
– The original authorization period has not expired
• If services are continued during the appeal or State Administrative
Hearing and the decision is not in the member’s favor, the Health Plan
may recover the cost of the services provided to the member
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Fraud, Waste and Abuse
Fraud, Waste and Abuse
• Fraud
– Intentional deception or misrepresentation made by an entity or person
with knowledge that the deception could result in some unauthorized
benefit to entity, her/himself or to some other person
• Waste
– Overutilization of services (including DME products) or other practices
that do not improve health outcomes and result in unnecessary costs
whether it tangible or intangible
• Abuse
– Provider: Provider practices that are inconsistent with sound fiscal,
business, or medical practices, and result in an unnecessary cost to
the program, or in reimbursement for services not medically necessary
– Member: Intentional infliction of physical, harm, injury caused by
negligent acts or omissions, unreasonable confinement, sexual or
emotional abuse or sexual assault
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Fraud, Waste and Abuse (continued)
• Prevention
– Make a copy of the member’s ID card and photo ID before rendering
services
– Validate member’s current demographic information for each visit
– Provide staff and partners ongoing training on appropriate
documentation and billing practices
• Reporting
– Providers must report all suspected cases of fraud, waste or abuse to
Provider Services by calling 1-888-980-8728
– The health plan will report all suspected fraud, waste and abuse cases
to the Med-QUEST Division, Medical Standards and Medicaid Fraud
Control Unit of the Attorney General’s Office
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Member Rights and
Responsibilities
Member Rights & Responsibilities
• We are committed to promoting dignity, quality of life, and
appropriate standards for assuring quality care for our members.
• Members receive notice of their rights and responsibilities via the
Member Handbook, which is included in the New Member Packet
mailed to all new members.
• Included in today’s education and training packet is a copy of the
“Member Rights and Responsibilities Quick Reference Guide”
• Members are also notified of their rights and responsibilities via
the member newsletter and online at:
www.uhccommunityplan.com.
• Available in the Provider Administrative Guide under the Member
Rights and Responsibility section
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cultural Competency
• Cultural competency is a key component of the Health Plan’s continuous quality
improvement efforts and its goal is to ensure delivery of the highest quality of care
to every member in a manner that recognizes, affirms and respects the worth of
the individual and protects and preserves their dignity regardless of their race,
color, creed, ancestry, sex including gender identity/expression, sexual orientation,
religion, health/income status or physical/mental disability.
• Our goal is to engage members, providers, key stakeholders and the community to
continuously improve our cultural competency program, allowing our members:
•
•
•
•
Effective, understandable and respectful care
Sign language and language interpretation services other than English
– Contact us for assistance to ensure members have access to these services
Culturally sensitive and appropriate educational materials
To freely participate in their care planning
• Physicians, RNs and Pharmacists can register today to explore cultural
competency in health care while earning credit at:
https://ccnm.thinkculturalhealth.hhs.gov/default.asp
• You may obtain a copy of our cultural competency plan by contacting Provider
Services toll free at: 1-888-980-8728 or download a free copy by visiting:
www.uhccommunityplan.com
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Cover
area with cropped
image.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Do not overlap
blue bar.
Completely cover
gray area.
Cover
area with cropped
image.
Do not overlap
blue bar.
Completely cover
gray area.
Medical Record Keeping and
Documentation Requirements
Member Medical Record
• All network providers must follow the medical record requirements
– Two Vital Elements to a member’s individual paper or electronic
medical record:
•
•
Medical office recordkeeping system requirements
Procedural/Clinical documentation requirements
– Medical Record Keeping Reference Tool (included in today’s
packet) provides:
•
•
•
Record keeping systems
Chart documentation
A complete listing of the requirements/standards
– Requirements/standards are also found in the Provider
Administrative Guide
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Data Collection Requirements
• DHS requires the health plans to maintain a health information
system that integrates all data to evaluate and report statistical data
related to:
•
•
•
•
Quality
Utilization
Costs
Other matters (DHS may request from time to time)
• Providers are required to submit complete and accurate encounter
data or claims submission that must be tied to the medical record
documentation (i.e. claims billed must be based on what is documented
in the member's medical records).
• The Health Plan may request medical records for the purpose of
validating encounters or paying claims.
• Claims audits are conducted to ensure compliance.
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Resources
Clinical Practice Guidelines (CPG)
– Evidenced-based guidelines to monitor and improve the quality of care
provided by participating providers.
– Clinical, behavioral health, preventive health and pharmaceutical guidelines are
reviewed at least annually and approved by the Executive Medical Policy
Committee (EMPC).
– Using state and/or national guidelines, as well as HEDIS data, quality indicators
for preventive care services are monitored and analyzed on a continual basis
and interventions are implemented as indicated for continued quality
improvement.
– Visit our website to for the most current CPG
http://www.uhccommunityplan.com/health-professionals/HI/clinical-practiceguidelines or you may call Provider Services for a free copy at 1-888-980-8728.
– ePrescribing capability is now available for providers
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Provider Websites
• Participating providers can log onto our secure website for member
eligibility, online claims submission, prior authorization submission and
status, and other online provider services:
– www.unitedhealthcareonline.com
• Providers can go to our public website to view and download the provider
administrative guide, forms, provider directory, disease management best
practice guides, newsletters and more at:
– www.UHCCommunityPlan.com/health-professionals
• Providers may also check eligibility by logging on to the DHS Medicaid
website at:
– https://hiweb.statemediciad.us/home.asp
(Handout: Provider Quick Reference Guide)
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
UnitedHealthcareonline.com
Click on Tools and Resources
67
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
UnitedHealthcareonline.com
Click on UnitedHeathcare
Community Plan Resources
68
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
UnitedHealthcareonline.com
Click on Hawaii
69
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
UnitedHealthcareonline.com
70
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Other Info and Helpful Links
Sign up for online access & service at www.unitedhealthcareonline.com or
1-866-842-3278 (option 5 for electronic payment sign up)
UHC Medicare Plan website: www.uhcmedicaresolutions.com
UHC Electronic Payment & Statements demo: www.welcometoeps.com
Optum Behavioral Health: www.providerexpress.com
For questions on electronic billing the appropriate process is to contact the
EDI Hotline at 800-842-1109
Submit claims electronically using Payer ID 87726
Governor’s Office on Aging (Sage+) : Oahu (808) 586-7299, toll free
number from the neighbor islands and the mainland: 1-888-875-9229
Local CMS Office : (808) 541-2732 (Honolulu)
CMS Website : www.medicare.gov
Social Security Administration: www.socialsecurity.gov
Medicaid Office : www.state.hi.us/dhs (808) 586-5390 (Kapolei)
Local Call Center
For Provider and Member Services contact information:
Monday – Friday 7:45 AM to 4:30 PM
Phone:
TTY:
1-888-980-8728
711
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
THANK YOU!
ARE THERE
ANY
QUESTIONS WE
CAN ANSWER?
Confidential Property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.