Updates Neuropathic Pain
advertisement

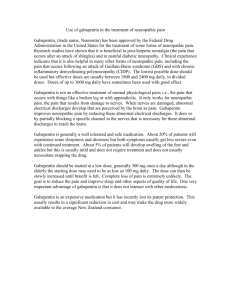
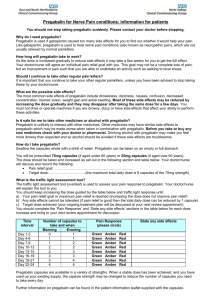
Neuropathic & Muscle Pain: Rational Polypharmacy Anticonvulsants, Antidepressants, Muscle Relaxers Steven Stanos, DO Center for Pain Management Rehabilitation Institute of Chicago IASP NEUROPATHIC PAIN: “initiated or caused by a primary lesion or dysfunction in the nervous system” “Nociceptive” vs. “Non-Nociceptive” Beydoun A, Backonja. J Pain Symp Management 2003. Cutaneous Sensation C-fiber • Small diameter • Slow conducting • Unmyelinated Caterina, Cur Op in Neurobiology (9), 1999. A-δ • Medium diameter • Fast conducting • Lightly myelinated • Polymodal Primary Afferent C & Aβ Fibers Sensation Mediated Fibre Threshold Principal Receptors Class For Transmitters Engaged Physiological Activation SP/NKA NK Noxious C High (pain) CGRP CGRP EAA NMDA AMPA mGlu Aβ Low EAA Millan, Progress in Neurobiology, 1999. AMPA Innocuous (no pain) Pathological Highly noxious (hyperalgesia) Cold Allodynia (pain) Mechanical allodynia Neuropathic Pain: A PARADOX Cutting a telephone wire Spontaneous Paresthesias Dysesthesias Pain Movement evoked pain Tenderness with denervation Peculiar symptoms Paroxysmal Electric shock-like Tingling Shooting Burning Neuropathic Pain MECHANISMS • • • • • Ectopic activity in sensitized C-nociceptors Regenerating nerve sprouts Recruitment of silent nociceptors Spontaneous/evoked activity in DRGs Neuronal “hyperexitability” Molecular Changes • • • • Sodium channel accumulation Glutamate receptor activity Reduction of GABA-ergic inhibition Penetration of calcium into cells Jensen T. European J Pain 2002; (6) A. Peripheral Sensitization SKIN Plasma Extravasation Vasodilation Macrophage Mast Cell TNF-α IL-6 LIF Tissue Damage Pressure ? Heat 5-HT3 Histamine PGE2 VR1 H+ 5-HT3 H1 Bradykinin EP H+ IL1ß NGF ATP B1/B2 IL1-R TrkA P2X ASIC Ca2+ (PKC) PKA PKC TTXr (SNS/SNS2) TTXs Gene Regulation TTXr Sub P Adapted from Woolf CJ, et al. Science. 2000;288:1765-1768. Peripheral Nerve Terminal Central Mechanisms/ Wind Up Hansson PT, Fields HL, Hill RG, Marchettini P eds, Neuropathic Pain: Pathophysiology and Treatment, International Association for the Study of Pain Press, Seattle, 2001 Central Sensitization Voltage sensitive: Ligand gated: N & P/Q channels Α2δ subunit L channel NMDA / glutamate Type C fibers GLU SP Voltagegated Ca2+ channel GLU SP AMPA Na+ Ca2+ K NMDA Ca2+ + Type C fibers Ca2+ Ca2 + NOsynthase NO Immediate-early genes (C-fos, C-jun) IP3 ACPD GL U SP Adapted with permission from Ollat H, Cesaro P. Pharmacology of neuropathic pain. Clin Neuropharmacol. 1995; 18:391-404. Mendell, NEJM 348;13,2003 SODIUM CHANNELS • Tetrodotoxin-sensitive • Tetrodotoxin-resistant Future: cloning human DRG GABA Glutamate Excitatory GABA Inhibitory GABA Modulate receptor (-)GABA transaminase (-) reuptake Enhance GABA 1st Generation Barbiturates Benzodiazipines Valproate 2nd Generation Tiababine (Gabitril) Topiramate (Topamax) Vigabitrin (Sabril) Zonisamide (Zonegran) *Gabapentin (Neurontin) *Pregabalin (Lyrica) NSAIDs Tricyclic Antidepressants Antiepileptics Topical Analgesics Tricyclic Antidepressants • Central blockade of monoamine uptake • Enhancement of descending inhibition • Adrenergic blockade on sprouts, NMDA antagonistic effects, opioid modification, and sodium channel blockade • Constant vs. Paroxysmal pain • Nortriptyline = Amitriptyline (McQuay, Pain, 1996) Tricyclic Antidepressants: Adverse Effects • Commonly reported AEs (generally anticholinergic): – – – – – – – – – blurred vision cognitive changes constipation dry mouth orthostatic hypotension sedation sexual dysfunction tachycardia urinary retention AEs = adverse effects. Fewest AEs • Desipramine • Nortriptyline • Imipramine • Doxepin • Amitriptyline Most AEs Neuropathy PHN Central Pain All types 3.0 2.3 1.7 TCA all types 2.4 2.3 1.7 TCA serot / norad 2.0 2.4 1.7 SSRI 6.7 ND ND Antidepressants Ion Channel Blockers Mexilitine 10.0 Phenytoin 2.1 Carbamazepine 3.3 Gabapentin 3.7 3.2 NMDA Antagonist Dextromethorphan 1.9 Oxycodone Capsaicin 2.5 5.9 Sindrup, Jenson Pain 83, 1999 5.3 Tricyclic Antidepressants: Positive Controlled Trials Study Painful DPN Max Max N Weeks 29 108 12 14 Pain relief Pain relief 26 6 Max Amitriptyline (25-150, PBO) Desipramine (12.5-150, PBO), Amitriptyline (12.5-150, PBO) Desipramine (50 or 200, PBO), Clomipramine (50 or 75, PBO) Desipramine (12.5-250, PBO) 20 12 Neuropathy symptoms Pain relief PHN Watson Max Graff-Radford Kishore-Kumar Raja Amitriptyline (12.5, PBO) Amitriptyline (12.5-150, PBO) Amitriptyline (12.5-200, PBO) Desipramine (12.5-250, PBO) Nortriptyline (10-160, PBO) 24 58 49 26 76 8 12 8 12 24 Sindrup Agent (mg/d) Primary End Point Pain relief Pain relief Pain intensity Pain relief Pain intensity, relief; cognitive function Max et al. Neurology. 1987;37:589 1987;37:589--596; 596; Max et al. N Engl J Med. 1992;326:1250 1992;326:1250--1256; 1256; Sindrup et al. Br J Clin Pharmacol. Pharmacol. 1990;30:683 1990;30:683--691; 691; Max et al. Pain. 1991;45:3 1991;45:3--9; Watson et al. Neurology. 1982;32:671 1982;32:671--673; 673; Max et al. Neurology. 1988;38:1427 ;16:188--192; 1988;38:1427--1432; 1432; GraffGraff-Radford et al. Clin J Pain. 2000 2000;16:188 192; KishoreKishore-Kumar et al. Clin Pharmacol Ther. 1990;47:305 1990;47:305--312; 312; Raja et al. Neurology. 2002;59:1015 2002;59:1015--1021. 1021. Antidepressants Class of Medicatio Medication n Action Tricyclic Amitripyline Nortriptyline Serotonergic, noradrenergic, anticholinergic, Na+ channel blocker, antihistaminic Noradrenergic, anti-cholinergic, Na+ channel blocker, antihistaminic Tricyclic Desipramine SSRI Escitalopram Citalopram Sertraline Serotonergic SNRI Vanlefaxine Duloxetine* Atypical Mirtazepine Site of Action Therapeutic Effects Side Effects Brain Descending pathways peripheral nerve Brain Descending pathways peripheral nerve Brain Descending pathways Antidepressant Drowsiness, Dry Analgesic (neuropathic mouth, constipation, pain at low dose) arrythmia, urinary retention, weight gain Antidepressant Drowsiness, agitation Analgesic (neuropathic pain at low dose) Antidepressant sexual dysfunction, perspiration Serotonergic Noradrenergic Brain Descending pathways Antidepressant Analgesic sexual dysfunction, perspiration, drowsiness Serotonergic Antihistaminic Brain Descending pathways Antidepressant Drowsiness, weight gain *FDA indicated for diabetic peripheral neuropathy. Physician's Desk Reference. Montvale, NJ: Thomson PDR; 2005 Pharmacologic Profile of Antidepressants Type of Action Receptor Type TCAs Amitriptyline Clomipramine Imipramine Desipramine Maprotiline* Nortriptyline SNRIs SSRIs Duloxetine Venlafaxine Citalopram Fluoxetine Paroxetine (±)? Ion channel blockade Sodium channel Calcium channel + + + + (±) ? ? ? Monoamine transporter blockade 5-HT Norepinephrine Dopamine + + – (±) + + – + – – – – – – – – – – + – α-Adrenergic + + H1-Histaminergic + + Receptor Muscarinicblockade cholinergic + + + + *Tetracyclic antidepressant. NMDA +=present; (+)=weak; –=not present; ?=unknown; 5-HT=serotonin. Sindrup S, Jensen T. Hansson P, Fields H, Hill R, Marchettini P, eds. Neuropathic Pain: Pathophysiology and Treatment Progress in Pain Research and Management. Seattle, Wash: IASP Press;2001:169-183. 1st generation anticonvulsants • Phenytoin Diabetic Neuropathy: NNT: 2.1 • Carbamazepine (300 – 1000 mg/day) Trigeminal Neuralgia: NNT: 2.6 NNH: 3.4 Diabetic Neuropathy: • Valproic acid: 3.3 FDA-Approved Treatments for Neuropathic Pain • Carbamazepine – Trigeminal neuralgia • Duloxetine – Peripheral diabetic neuropathy • Gabapentin – Postherpetic neuralgia • Lidocaine Patch 5% – Postherpetic neuralgia • Pregabalin – Peripheral diabetic neuropathy – Postherpetic neuralgia AED action Medication Action Side Effects Interaction Gabapenitin Pregabalin Ca++ Channel modifiers Short term memory loss, Opioids weight gain, confusion Topirimate Ca++, Na++ chan, fatigue, wt loss, nrw GABA-ar, CA in, free angle glaucoma, renal radical scavenger stones BCPs, First gen AEDs Tiagabine GABA Reuptake inhibitor First gen AEDs Lamotrigine Anti TB drugs, First Ca++, Na+ chan, Dec Dizzy, somn, nausea, gen AEDs, NMDA Ca, GABA-ar ataxia, Stevens Johnson oxcarbazepine Oxcarbazepine Na+ chan, K+ efflux Levetiracitam Blocks inhibitors of Somnolence, dizzy, GABA-ar (Zinc, beta agitation, headache, carboline) aggression Dyspepsia, drowsiness, confusion, seizure Hyponatremia, nausea, BCPs, cyclosporine HA, dizzy, hepatotoxicity Physician's Desk Reference. Montvale, NJ: Thomson PDR; 2005 None Topiramate (Topamax) 25, 100, 200mg 1. Modulation of voltage-gated Na channels 2. Potentiate GABA inhibition 3. Block Glutamate neurotransmission 4. Modulate Ca channels 5. Inhibition of carbonic anhydrase side effect. perioral paresthesias Side effects: diarrhea, anorexia, somnelance, asthenia, weight loss, confusion 6. Renal stones: 2-4 times greater risk 7. Oligohydrosis, metabolic acidosis warning Chong, Clin J Pain (19),2003. Topiramate (Topamax) (Edwards, 1998) DN, N=8, 258mg/day, VAS 8.7 vs. 4.5 (Zvarau,2000) TN/MS, N=6,200-300mg/day, 4=complete (Haugh,2000) TN, N=8, avg. 175mg/day (Potter, 2000) NPP, N=14, weekly titration 25mg, First Pain Relief = 214 mg/day Last visit dose = 271 mg/day, VAS 8.8 vs. 3.1 (Pappagallo, 1998) refractory chronic pain Pain reduction correlated with allodynia (Rosenthal,2003) DN, N= 323, titrated to 400mg/day VAS: pre 68.0, post 46.2 (54.0) >50% in VAS: 36% Chong, Clin J Pain (19),2003. Lamotrigine (Lamictal) 25, 100, 150, 200mg • • • • • Blocks voltage-sensitive sodium channels Inhibits pre-synaptic glutamate release Lack of drug interactions No serum monitoring Rash Lamotragine (Lamictal) Zabrzewska Pain 73 (1997) N = 14 DBPC Refractory TN Superior to placebo 11/13 400 mg Eisenberg 2000 N = 59 NP 6.4 to 4.1 Eisenberg Eur J Pain 7 (2003) N = 14 Sciatica VAS 7.9 to 4.1 50% completed 25-400 mg/day 400 mg Simpson Neurology 60 (2003) N= 227 RDBPC HIVassociated DSP/ ATN Effective in patients on neurotoxic ART 400 mg Oxcarbazepine (Trileptal) 150, 300, 600mg • Keto analog of Carbamazepine (Tegretol) • Active metabolite (MHD) • Voltage-dependent sodium channels • N-type calcium channel effect • Potentiate dopamine, inhibit glutamate • TGN: 900-2100 mg/day • APS 2004: 700-800 mg/day Ambrosio et al, Neurochemical Res 27, 2002. Tiagabine Selective GABA Reuptake Inhibitor (SGRI) 2, 4, 12, 16mg Tiagabine(Gabitril) Jenson 2002 N = 10 NP refractory to gabapentin 80% good to 12 mg/day excellent Kanard 2000 N = 17 Painful Sensory Neuropathy 50% 4 to 16 mg/ discontinued day Taylor FB J Clin Psych 2003 N=7 PTSD 6/7 Improved 4 – 12 mg/ day Kirby APS 2004 N = 14 Diabetic Neuropathy Decreased pain, improved sleep 16 mg/day Zonisamide: Mechanisms of Action • Reduces repetitive neuronal firing via blockade of Na+ channels1 • Reduces voltage-dependent T-type Ca+2 channels2, facilitates dopaminergic and serotonergic neurotransmission1 • Weakly inhibits carbonic anhydrase2 • Blocks K+ evoked glutamate release3 • Long half life: 63 – 69 hours • Sulfonamide derivative 1Schauf. 2Suzuki, Brain Res. 1987;413:185-188. et al. Epilepsy Res. 1992;12:21-27. Levetiracetam (Keppra) • Atypical GABAergic & glycine effects • (-) zinc & beta carbolines, enhancing choride ion influx at GABA-A receptor • No hepatic metabolism, low protein binding • Rapid dosage titration • Case reports of rectal use (1000 BID) Dunteman APS, 2004 Levetiracetam (Keppra) Cochran APS,2003 NP N = 15 Rowbotham Neoplastic N = 10 AAN,2003 NP Price Clin J Pain, 20(1), 2004 Periph 3 cases Neuropathy Kaplan APS, 2004 57% Radic 26% HA 17% DN N = 53 65% very effective 1000 2000mg 33% responders 500 – 3000mg 500 – 1500mg BID 92% good to 750 – excellent 1500mg Anxiety Pregabalin Binds to the 2- Subunit of Voltage-Gated Ca2+ Channels in the Central Nervous System Pregabalin Presynaptic α2- subunit Ca2+ channel Neurotransmitters Presynaptic α2- subunit Ca2+ channel Neurotransmitters Postsynaptic Postsynaptic Schematic representation of pregabalin’s proposed mechanism of action • Pregabalin selectively binds to 2- subunit of calcium channels • • • • Modulates calcium influx in hyperexcited neurons Reduces neurotransmitter release Pharmacologic effect requires binding at this site The clinical significance of these observations in humans is currently unknown Taylor. CNS Drug Rev. 2004;10:1832004;10:183-188. Pregabalin Is Not a Calcium Channel Blocker Ion channel Ion channel PREGABALIN α2 α2 EXTRACELLULAR EXTRACELLULAR CCB α1 Ca2+ influx blocked α1 β δ Cell membrane INTRACELLULAR • Ca2+ channel blockers (CCBs) bind to 1 subunit • • of L-type calcium channels and directly block the pore CCBs prevent movement of Ca2+ CCBs work in the peripheral vascular smooth muscle and relax arteries to reduce systemic blood pressure α1 α1 β Ca2+ influx attenuated δ Cell membrane INTRACELLULAR • Pregabalin binds to the 2- subunit and modulates the influx of Ca2+ into the cell in hyperexcited neurons – Pregabalin works at brain and spinal cord synapses that have Ca2+ channels, but does not alter vascular or cardiac function Pregabalin modulates Ca2+ channels (does not block) Triggle. Triggle. Cleve Clin J Med. Med. 1992;59:6171992;59:617-627; Taylor. CNS Drug Rev. 2004;10:1832004;10:183-188; Data on file. Pfizer Inc, New York, NY. Pregabalin: Predictable Response Versus Gabapentin Linear PK Profile High Bioavailability 18 Steady State Cmax (μg/mL) 16 Pregabalin Gabapentin 14 900 mg, 60% 12 μ 10 All doses 8 90% 1200 mg, 47% 2400 mg, 34% 3600 mg, 33% 6 4 Pregabalin Gabapentin 2 1800 mg Recommended dose 0 0 600 1200 1800 2400 3000 3600 4200 4800 Dose (mg/d) Lyrica® (pregabalin) Capsules CV [package insert]. New York, NY: Pfizer Inc; 2005; 2005; Neurontin® (gabapentin) [package insert]. New York, NY: Pfizer Inc; 2004; Wesche, Wesche, Bockbrader. Bockbrader. Presented at: 24th Annual Scientific Meeting of the American Pain Society; 2005. Mechansims, Mechanisms AED Na+ Channel Blockade Pregabalin Gabapentin Lamotrigine Ca2+ Channel Blockade Glutamate Antagonism GABA Potentiation Carbonic Anhydrase Inhibition X X* X Topiramate X Tiagabine OxcarbazepineX Zonisamide X Levetiracetam X X X X X X X X X X X X mechanism unknown *Mechanism not clearly established. White HS. In: Pellock JM, Dodson WE, Bourgeois BFD, eds. Pediatric Epilepsy: Diagnosis and Therapy. 2nd ed. New York, NY: Demos Medical Publishing Inc; 2001:301-316. • • • • Muscle Relaxers: Patterns of Use 85% took for back pain1 Average length of use: 2.1 years1 44.5% took longer than 1 year1 No difference in use patterns in those patients with ambulatory impairment or lung disease1 • Benzodiazepine and muscle relaxer use associated with fractures in elderly2 1. Dillon C, et al. Spine 2004;8:892-96. 2. Coutinho E, et al. BMC Geriatrics 2008;9:21. Muscle Relaxants Muscle Relaxers Name Generic Staring dose Effective dose Cyclobenzaprine Flexeril 5mg TID 10-20mg TID Orphenadrine Norflex 100 mg BID 100 mg TID Carisoprodol Soma 350 mg TID 350 mg QID Metaxalone Skelaxin 400 mg TID 800 mg TID Methocarbomal Robaxin 500 mg QID 750 mg QID Balcofen Lioresol 5mg TID 10-20 mg TID Cyclobenzaprine (Flexeril) (5mg, 10mg) • FDA approved 1977 (10mg) • Animal studies1: via serotonin receptors at spinal level to block alpha-mononeuronal excitation • “muscle spasm” dose: 5mg TID • 2 studies for acute pain 2: Result: 7 day treatment, by day 3, 78%-83% relief, average 2 days earlier (30% reduction in time to relief) 1. Honda M, et al. Eur J Pharmacol. 2003;458:91-99. 2. Borenstein DG, Korn S. Clin Ther. 2003;25:1056-73. Cyclobenzaprine: Meta-analysis • Treated patients 5x as likely to report symptom improvement by day 14 vs. placebo1 • Effect is greatest in first 4 days • NNT: 2.7 • Effects size: 0.5 • Myofascial Pain2: (2 studies) – Insufficient evidence 1. Browning R, et al. Arch Intern Med. 2001;161:1613-20 2. Leite et al. Cochrane Database 2009;3:CD006830. Cyclobenzaprine HCl ER (Amrix) Amrix (Cephalon): 15mg or 30mg Q day Tmax: 8.1 hrs, T1/2: 34 hrs Results: 15 mg and 30mg effective in treating muscle spasm associated with painful MSK conditions after 4 days 1. Malanga G, et al. Cur Med Res Opinioin 2009;251179-96. 2. Cyclobenzaprine ER/ Amrix package insert (Cephalon), 2009 Metaxalone • FDA approved 19641 • “adjuvant therapy to rest, PT, and other measures for the relief of discomforts ” • 400mg to 800 mg TID or QID • 69.6% vs. 17.4% marked or moderate improvement • Onset of action: 1 hr • Peak levels: 2 hr • Tmax: 4.3 h (fat meal); 3.3 h (fasting) • Duration: 4-6 h 1. Fathie K. Curr Ther Res Clin Exp. 1964;6:677-83. Carisoprodol (Soma) • FDA approved in 1959 • Human evidence of muscle relaxation limited, animal models possible block of descending reticular formation in spinal cord1 • Dose: 350mg QID • Soma vs. Butabarbital2:at 4 days, greater overall relief • Metabolite: meprobamate (Schedule IV) • SOMA scheduled in individual states • 14 of 20: list of abused mood-altering substances2 1. Physicians’ Desk Ref, 58th ed, PDR, 2004. 2. Hindle TH, California Med. 1972;117:7-11. 3. Prescription Drug Addiction: http://www.addicusbooks.com/news_release_RxAddiction.htm Abuse Potential: Soma • n = 40, use of Soma for > 3 months, with/without history of substance abuse • Results: (with Hx substance abuse): – 40% used in larger amounts than prescribed – 30% used for an effect other than prescribed – 10% used to augment effect of another med – 20% attempted to obtain extra Soma prescription – 10% used others, or obtained illegally • All patients with Hx abuse: 65% used Soma in >1 of the above Reeves RR, et al. J Addict Dis. 1999;18:51-56. Muscle Relaxants in Acute LBP Bernstein et al, Spine 2004;29:1346-131. • Good: APAP NSAIDs, muscle relaxers (acute), TCAs (chronic) • Fair: tramadol, benzos, gabapentin (radiculopathy) • 36 trials in 4 systematic reviews • Duration of trials 2 weeks or less • Acute LBP: muscle relaxants superior 2-4 days • Mixed results for cyclobenzaprine Chou R, Huffman L. Ann Intern Med. 2007;147:505-14. Tizanidine • Peak serum levels:1-5 hrs • ½ life: 4-8 hrs • Side effects: dry mouth, somnolence, hypotension, bradycardia • Renal impairment: clearance 50% • Max dose 36 mg/day • Muscle spasm1:tizanidine vs. diazepam (7D) Greater lateral flexion • Myofascial Pain2: titrated to 12 mg, improved pain, sleep, pressure thresholds 1. Fryda-Kaurimsky Z. J Int Med Res. 1981:9:501-5. 2. Malange G, et al Pain Phys 2002;5:422-32. 57 Topical Agents for Myofascial Pain • Lidocaine Patch 5% • Diclofenac Patch 1.3% Lidocaine Patch vs. lidocaine injection Methods: lidocaine patch BID, placebo patch BID, TrP injection 1 mL 0.5% bupicacaine Outcomes: VAS, pain attacks, pain-related function, pressure and pain thresholds Results: Affaitati G, et al. Clin Ther 2009;31:705-720. Lidocaine Patch vs. bupivicaine injection Affaitati G, et al. Clin Ther 2009;31:705-720. Diclofenac Patch • Study: MPS upper trapezius • Diclofenac 60mg patch TID vs, Menthol patch • Outcomes: VAS, cervical ROM, pain threshold, PGIC, neck disability index • Results: – Day 4: 27% reduction in VAS vs. 21% – Day 8: 51% reduction in VAS vs. 25% Hsieh L, et al J Pain Symptom Manage 2009, in press.