Click here to - National Health Systems Resource Centre
advertisement

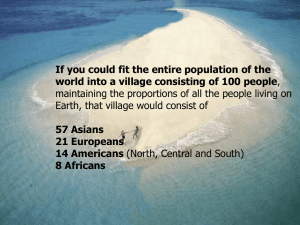
Aarogya-Swaraj An empowerment model of health care Abhay Bang SEARCH, Gadchiroli Outline • Current challenge of health care. • Data and learning from Gadchiroli. • Alternative model of health care. Health Care cost in India Health care cost : 5% of the GDP $ 100 per capita per year (at ppp) 20% by the public sector 80% by the private sector Health status of the people in India • • • • 2 million new cases of TB annually 55% women anemic 43% children underweight 1.5 million child deaths each year The quest for Universal Health Care * How to provide UHC? The US medical care cost : $ 6000 per capita/year Cost of Health Care % of GDP 2010 2050 2100 US 17 % 37 % 97% Europe 10 % 25 % 60% The medical care models from the West are wasteful * UHC = MEGs A Medical Employment Guarantee Scheme Medical Nemesis Health care of ventilators What is the alternative? SEARCH Society for Education, Action & Research in Community Health New Delhi Bombay Gadchiroli Laboratory of 86 villages SEARCH, Gadchiroli What are the health care needs of the people? 1. Ask them 2. Population based data 3. Hospital data SEARCH, Gadchiroli The priorities expressed by the people (not in any order of ranking) 1. Communicable diseases (diarrhea, malaria, TB, filariasis) 2. Respiratory problems (cough and breathlessness.) 3. Back-ache and musculo-skeletal pains 4. Sexual, reproductive and uro-genital problems. 5. Weakness – (anemia, malnutrition ?) 6. Blood pressure and stroke 7. Alcohol and tobacco 8. Anxiety Interestingly, missing were the national vertical program priorities such as the Maternal Mortality, Family Planning, Polio, HIV. * Universal Health Care must move beyond the few vertical programs and incorporate people’s priorities. Causes of death in children ( 0-5 Year) Govt. Program area ( 2004-2010) Causes Neonatal : ( Deaths : 314 , Live births : 5146) Cause Specific Mortality Rate per 1000 Live Births 1 Birth Injury / Asphyxia 2 Prematurity 3 Neonatal sepsis 4 Low birth weight 29.3 20.6 13.4 11.7 1month – 5 years 1 Pneumonia 2 Malnutrition 3 Encephalitis/ Meningnitis / cerebral malaria 14.4 6.8 5.2 Causes of death In age group above 15 years (SEARCH 86 villages 2002-2009) ( person years : 520,162 , Total deaths : 5003 ) Suicide Heart disease Malaria Cancer Accident or poisoning TB Diarrhoea Asthma / COPD Stroke Unexplained fever Pneumonia /Ac. Bronchitis 0 50 100 150 200 Cause specific mort. rate per 100000 popul. Population based morbidity studies in Gadchiroli A) Newborns and Children Expected cases / village of 1000 1) Newborn morbidities Incidence of morbidities in newborns 74 % 15 2) Childhood ARI Acute Respiratory Infections in children - Incidence of cough and cold 6 episodes per child / year 600 - Incidence of Pneumonia 13 % of children / year 13 Population based morbidity studies in Gadchiroli Expected cases / village of 1000 B) Women 3) Maternal morbidities Incidence of Maternal morbidities during - pregnancy, delivery , post partum : 59 % - Emergency Morbidities : 13 % 12 3 4) Gyneacological morbiditiesGynecological and sexual morbidities prevalence ( n=650) : 92 % 340 5) Prevalence of anemia in women Anemia in women ( n= 2019) : 59% 12 - non pregnant women : 43 % 159 - During pregnancy Population based morbidity studies in Gadchiroli Expected cases / village of 1000 C) Men 6) Prevalence of health complaints in males - Non-reproductive symptoms : 70 % 259 - Reproductive, urogenital, sexual : 68 % 252 7) Prevalence of Alcohol consumption Prevalence of alcohol consumption : 36 % 133 - Prevalence of daily alcohol consumption : 4 % 15 - Prevalence of alcohol consumption Population based morbidity studies in Gadchiroli Expected cases / village of 1000 D) Population 8) Prevalence of tobacco consumption Tobacco consumption : 50.4 % 504 9) Prevalence of hypertension Hypertension (n= 879) in Males : 6.5% in females : 13.5 % 24 50 10) Prevalence of sickle cell gene Prevalence of sickle cell gene Homozygous ( S – S ) : 0.80 % 8 Heterozygous ( A – S ) : 15.60 % 156 The health care needs of population are enormous in magnitude, multiple, and are often chronic.( 2600) Health care must be designed appropriately Rs. 140 million District Development plan Rs. 200 million spent on alcohol * “Now we know why are we poor” People’s parliament and people’s prohibition Government of Maharashtra accepted the demand Introduced prohibition in Gadchiroli District in 1993. Private expenditure on tobacco versus the Government’s annual expenditure on three national schemes in the Gadchiroli district (2008-09,Rs Crore) Crore Rs. 100 90 80 70 60 50 40 30 20 10 0 73.4 22 14.9 Tobacco NREGA ICDS 10.4 NRHM NREGA- National Rural Employment Guarantee Act Scheme ICDS- Integrated Child Development Services NRHM – National Rural Health Mission Social Determinants of Health (e.g. alcohol, sanitation ) - Policy change - Regulation - People’s education through public campaign - Corrective measures What Next ? What type of health care do people need ? Tribal friendly hospital • 26,000 patients from 1000 villages • Cerebral malaria • Snake bites • 500 major operations • Spine surgery, Gynec surgery • Mental Health OPD • Oral & dental health OPD Newborn and Child Deaths Newborns in India 27 million newborns are born each year 30 % born at home Even the hospital delivered mother and newborns are sent home < 24 hr. Newborn health care must visit where the neonates are. * SEARCH, Gadchiroli SEARCH, Gadchiroli Neonatal mortality rate (1993 to 2003) (intervention and control area) Neonatal mortality rate 80.0 70.0 Control area 60.0 50.0 40.0 30.0 Intervention area 20.0 10.0 0.0 1993-95 1995-96 Baseline Training & visiting 1996-97 1997-98 1998-01 2001-03 Interventions Full Continuation of care Interventions The Infant Mortality Rate in Gadchiroli (1988 – 2003) 39 intervention villages Infant Mortality Rate 140 120 100 Pneumonia case management Home-based newborn care 80 60 40 Linear regression trend in IMR 20 0 Year Reduction in IMR = 6 points per year * SEARCH, Gadchiroli SEARCH, Gadchiroli 11th & 12th Five Year Plan of India Gadchiroli model to be the main strategy to reduce IMR in India. SEARCH, Gadchiroli HBMNC Scaling up SEARCH, Gadchiroli ANKUR Project in Mahatashtra Africa 4 countries ICMR Study: Government of India, five states. 23 States in India Other Countries State ASHA training centers SEARCH, Gadchiroli Global Policy Statement Joint statement by the WHO, UNICEF, US-AID and Save the Children , US ( 2009). How to provide health care to 1.25 billion population living in 1 million villages/ hamlets ? Universal health care by a medical system may generate dependence, exploitation and astronomical costs. The best way of providing universal health care to 1.25 billion population is to generate * Universal Capacity to Care for Health. Universal Health Care must include : • Control of social determinants by regulations and social campaigns. • Generating pro-health culture through the media and school education. • Health education for behavior change. • Training and capacity building for self care, and care of the community. • Preventive and promotive activities • Health care in the village or close to village. • Continuum of care. Suggested Health Care in a Block Public health system Population Villages Village Health Work units (6 / village) x 100 Village Health and Sanitation Committees Health Centres (1/5,000 pop) Primary Health Centers (1/30,000) Community Health Centre (50 bed hospital) 100,000 100 600 100 20 3 1 Health care activities in the village Hours / 1000 popl /month Maternal and Newborn Health 7 activities 62 Sexual health + FP + Urogenital and gynecological problems 5 activities 63 Child health & Nutrition 7 activities 49 Communicable disease control & sanitation 7 activities Chronic diseases 5 activities Mental health , health promotion 8 activities 60 60 60 Village Health Team The 6 VHW units can be performed by • 6 different individuals, each working for nearly 2 hour per day • or two persons working for 6 hrs/day They can be women (ASHA) and men (ASHOK) (B) Health Centre One health centre per 5,000 population (5 villages) is proposed. In each block (100,000 population) the current 20 sub-centres (1:5000) should be upgraded as Health Centres,. Functions 1. Clinical services at health center. 2. Outreach services in 5 villages 3. Training 4. Supervision 5. Coordination * Annual budget Rs. 2 million Aarogya-Swaraj Hospitals Health care Community based care Individual and family : Behavior and capacity to care Health empowerment Social determinants : Policies , Development, Culture Social Health Health for All Alma-ata (1978) Universal Health Coverage UHC needs to be conceived and designed more radically * Dependence is a political disease Universal Health Care must include the fundamental freedom to be healthy (and not freedom to be sick) as well as universal capacity to care for health ‘Aarogya-Swaraj’ describes this goal better than a patronizing promise of access to cash-less medical care mass produced by a medical industry whether public or private ‘swa-stha’ * The concept of health, in India, is inalienably linked with autonomy The promise of universal health care itself should not produce universal disease of health care dependence. Evidence from Gadchiroli 1. People actively campaigned to control social determinants of ill health, such as alcohol. * Question 1 : Can this mobilization approach be applied to other determinants of ill health ? 2. People identified their health priorities correctly * Question 2 : What are the limitations of this approach ? Question 3: How can the People’s Health Assemblies be made an operational reality from the village, block to the national level ? The community Health Workers were feasible and very effective. * Question 4: How can such model be operationalzed on a large scale? Question 5: How can such model be financed ? Universal Health Care can not be a one more centrally financed and controlled scheme. It has to become a movement for health, autonomy and freedom ! Aarogya - Swaraj