Char - CCC and Res prep
advertisement
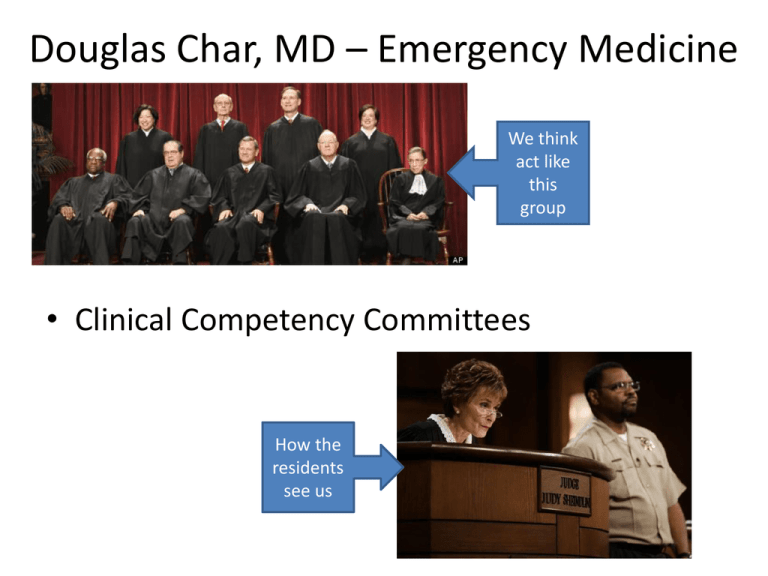
Douglas Char, MD – Emergency Medicine We think act like this group • Clinical Competency Committees How the residents see us Clinical Competency Committee • ACGME definition force us to broaden evaluation committee membership, change work process – – – – Expand beyond Program Directors PD is not chair but member of the committee Informal review -> formal assignment of milestone levels CCC meets prior to resident semi-annual performance evaluation (twice yearly) – Calendar allows submission of milestone data to ACGME Prior Approach based on 6-CC Interpersonal & Communications Skills Below Expectation Growth Area Meets Expectation History taking (EM1) – focus, depth X Team member effectiveness (EM1) X Communication patients/families (EM1) X Empathy (EM1) X Interaction with nurses and ED staff (EM1) X Clinical Attitude/ Problem solving (EM1) X Dealing with difficult patients (EM3) X Effectively delivers difficult info (EM3) X Team leader effectiveness (EM4) X Medical Knowledge Below Expectation Growth Area Meets Expectation General medical principles (EM1) X Intellectual curiosity (EM2) seeks new know X Fund of knowledge (EM2-4) in-train exam X Teaching – transfer of knowledge (EM3-4) X Application of know – clinical setting (EM3-4) X Not Applicable Not Applicable CCC Operationalize • 8-12 faculty member (PDs, FDs, core faculty) • It’s tons of work (48 residents takes 5+ hours) – Identify true stakeholders • Subcomm assigned to review each class the provide overview to full CCC – Class APD and 1-2 other faculty – 12-16 hours; review data, discuss, create report – Subgroup aware of class norms, follows individual throughout training • CCC ensured program norms between classes Performance Dashboard • Ideally pushes data to CCC members, residents in organized one stop shop format • Creating viable dashboard requires lots of IT muscle (residents faculty looking for fault) • Avoid getting trapped in the process - $$$ – Should there be a centralized resource? Milestones with Comments Comments (Core Competency): 1. Patient Care: Ahead of your peers, appropriate pace and number of patients seen (2.6/hour, class avg 2.14). Appears comfortable in physician role. Runs EM2 like an attending. 2. Medical Knowledge: Above average In-service score 83% (mean 72%), clinical judgment is excellent 3. Interpersonal & Communication: great with staff, patients. Need nursing evals. 4. Practice-based Learning: Continue self directed learning (follow up cases, procedure log, DOTs) on track. Good job tracking procedures focus on other procedures not just the RRC mandated core. 5. Professionalism: conf attendance great 100%, (8 hours of indep study) multiple compliments about bedside manner. 6. System-based Practice: Consider working on practice-based and quality improvement initiatives within the ED and hospital. Administrative Issues: 360 degree evaluation - 2/2 patient evals, 3/2 nursing evals, peers due in April 2014. 8 of 8 DOTs (3 Hx/Dx, 1 Dispo/dx, 1 professionalism, 1 systems based practice) , Procedure skills ( 8/4 – 2 wound care, 3 airway, 1 pain management, 2 vascular access) Need resuscitation DOTs (one for the semester) 1/1 resusc DOT Transition of care 1/1 Follow up cases 8/8 for the year (two months) EOS paper 17, electronic 12 ------------------------------------------------------------------------------------------------------------------------------Areas of Strength: XXX has a calm mature demeanor. Applies medical knowledge well, displays outstanding judgment for level of training. She gets along well with patients, staff and peers. Uses technology to accomplish and document safe healthcare delivery Uses the Electronic Health Record (EHR) to order tests, medications and document notes, and respond to alerts Reviews medications for patients Ensures that medical records are complete, with attention to preventing confusion and error Effectively and ethically uses technology for patient care, medical communication and learning X Comments: DOTs , FU cases (chart review) 8 of 8, faculty global rating Recognizes the risk of Uses decision support systems in computer shortcuts and reliance upon EHR (as applicable in institution) computer information on accurate patient care and documentation X Recommends systems re-design for improved computerized processes Gathering Data = Hassle Factor • Mistrust of data by residents, faculty • No good system to collect, lots of staff and faculty time • Residents see where data being applied Final Milestone Rating Decisions Preparing Residents for Milestones • Annual Retreat – we’ve talked NAS for the past 3 years • Self assessment – familiarize res w/ concepts, rankings • They don’t care about it until they get tripped up by the new rules • Have to make Milestones relevant to them • Include residents in plans & changes, this creates buy in (even if only in token way) • Make it clear this is moving target, it will change! Residents more invested than faculty Milestones likely to be part of their future as physicians • Maintenance of certification for Board status • Hospital privileging - ongoing CQI initiatives • Performance data have many uses