Presentation by Kara Kelb 10 May 2011
advertisement

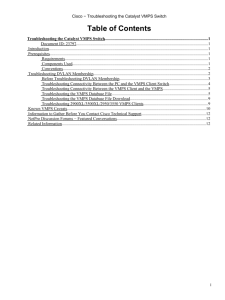
Members Talk May 10, 2011 Lean – is it generically applicable? Lean in different industries Lean in Healthcare in the U.S. Create a picture of your perfect “factory” Excerpt from US New and World Report What Medicine Can Learn From Business (U.S. News & World Report, June 17, 2008) “…During the visit, a team led by Virginia Mason's chief of medicine met with a Toyota guru, a sensei who had absorbed the Toyota approach into his very marrow. Examining a layout of the hospital, the sensei learned that there were waiting rooms scattered across the campus. "Who waits there?" the sensei asked. "Patients," said the chief of medicine. "What are they waiting for?" "The doctor." The sensei was told there might be a hundred or so such waiting rooms and that patients wait about 45 minutes on average. "You have a hundred waiting areas where patients wait an average of 45 minutes for a doctor?" He paused and let the question hang in the air. "Aren't you ashamed?“ “ Create a picture of your perfect factory Why? How do patients make Lean in Healthcare different? Lean in Healthcare Types of Customer Waste… Defects Re-sticks, redraws, med errors Overproduction Blood draws done early to accommodate lab Inventory Pts waiting for bed assignments Lab samples batched Dictation waiting for transcription Movement Looking for pts Missing meds Missing charts or equipment Excessive Processing Multiple bed moves Retesting Transportation Excessive transporting pts for tests Waiting Inpts waiting in ED Pts waiting for discharge MDs waiting for test results Under-utilization Nurses transporting patients to X-ray Lean in other industries… Financial Services Research from the Corporate Executive Board finds that financial firms leveraging Lean techniques achieve 20 percent to 40 percent cost reduction in 12 to 18 months. Equally remarkable are specific anecdotal results: One of the world’s largest financial institutions headquartered in the U.S., increased credit card activation by 10 percent in one year, achieving $2 million in additional revenue through increased card utilization. A prominent national bank reduced its wholesale lockbox (payment processing) unit cost by 58 percent while reducing associate handling time by 48 percent and errors by more than 75 percent in only eight months. By implementing the right Lean tools and practices at each level of the organization, they create a continuous improvement mindset throughout the culture. For example, senior leadership may leverage a “value-stream vision session event” as a methodology to support the continuous improvement goal of communicating, translating and deploying a new retail mortgage strategy. Middle managers may rely on Kaizen, Business Reviews, and “War” Rooms to drive weekly and monthly execution to operating commitments. And first level managers and employees may use MDI (Managing for Daily Improvement) tools, Performance Boards, and Point Kaizens for daily continuous improvement of existing processes. Ultimately, most executives who have experienced the transformative power of Lean note how it provides a disciplined, repeatable way to engage every employee to see their business from a customer’s perspective, identify areas for improvement and make changes rapidly. They say the true power of Lean isn’t just in the quick, dramatic results, but in its ability to create a sustaining, continuous improvement mindset throughout an organization. Examples • Cell manufacturing of CT scanners • Kanbans, Visual Instruction in factories • Factory lines synchronized to demand • Lean processing of payroll and benefits • Lean “complaints” processes • Early warning of equipment prior to break-down • Call centres using control charts to drive proactive action rather than wasted time later BUT… How do patients make Lean in Healthcare different? Lean in the US Healthcare System Miami Children’s http://www.youtube.com/watch?v=be1HsYhr82c&feature=youtube_gdata_player Virginia Mason Production System How VMPS Works Virginia Mason's vision is to be the Quality Leader in health care. This vision requires adopting a paradigm shift from expecting errors and defects, to believing that the perfect patient experience is possible. Key to accomplishing this is understanding that staff who do the work know what the problems are and have the best solutions. VMPS strategies range from small-scale ideas tested and implemented immediately to long-range planning that redesigns new spaces and processes. VM uses several continuous improvement activities, such as Rapid Process Improvement Workshops (RPIWs) and kaizen events focused on incremental changes, as well as 3P workshops intended to completely redesign a process. VM has held 850 continuous improvement activities involving staff, patients and guests. Benefits of VMPS •Patients spend more value-added time with providers, and VMPS helps providers deliver the best possible care. •Patients benefit from greater safety, less delay in seeing physicians for care and more timely results and treatments. •VM staff benefit by having less rework and greater opportunities to care for patients - one of the primary reasons many choose health care as a profession. •The reduction of waste in administrative processes that support patient care but take valuable resources ultimately benefits customers. As a nonprofit organziation, savings are reinvested to support VM's mission to improve patient health and well-being. Virginia Mason Continued VMPS Success Stories We have had many successes with VMPS. Below are a few examples of how VMPS has improved the quality of patient care. PSA System Improves Patient Safety Virginia Mason used VMPS to develop a Patient Safety Alert (PSA) system requiring all staff who encounter a situation likely to harm a patient to make an immediate report and cease any activity that could cause further harm. If the safety of a patient is indeed at risk, an investigation is immediately launched to correct the problem. From the program's inception in 2002 through 2009, 14,604 PSAs were reported. Most reports are processed within 24 hours — a significant improvement from when reports took three to 18 months to resolve. Patient safety at VM has increased and professional liability claims have dropped. One-Stop Care for Patients with Cancer Using VMPS, the Floyd & Delores Jones Cancer Institute at Virginia Mason was redesigned with a laboratory and pharmacy inside, elimininating the need for patients to travel throughout the hospital for chemotherapy. Now, all cancer services are brought directly to the patient in his or her private treatment room. For one patient, this reduced the length of a chemotherapy visit from 10 hours to two and saved about 500 feet of walking at each visit. Getting Back to Nursing In most hospitals, nurses spend about 35 percent of their time in direct patient care. With VMPS, VM nursing teams increased it to 90 percent. They used RPIWs to evaluate their work and make improvements. Instead of caring for patients throughout a unit, nurses work as a team with a patientcare technician in "cells" (groups of rooms located near each other). The cell model allows nurses to monitor patients and quickly attend to needs. Also, the most commonly used supplies for each unit were moved to patient rooms so nurses reduced walking back and forth to get supplies. Steps walked per day fell from 10,000 to roughly 1,200. Hyperbaric Center Increases Patient Capacity When the VM Center for Hyperbaric Medicine could no longer accommodate all the patients needing treatment, many assumed the solution was a new building to house larger chambers. Instead, VM used VMPS tools to design and build a new hyperbaric center in existing hospital space, which saved $2 million in construction costs and increased capacity from two to three patients at a time to as many as 20. Express Treatment in the Emergency Department Emergency departments (ED) are a major entry point for hospitals and can be a bottleneck. ED patient care is typically more expensive and involves longer wait times. Using VMPS, the ED team at VM learned to predict appropriate staffing levels for times of greatest demand. A "team sort" process using standard clinical assessment tools to quickly identify and sort patients' care needs was implemented. Those requiring minimal services receive express treatment and are discharged without going to patient-care beds. This creates capacity for patients who require more extensive services. This work helped VM decrease the number of hours the ED was closed and unable to receive new patients by more than 90 percent over the past two years. In 2011, VM will move its ED into more efficient space and the team sort process will allow the team to care for more patients. Faster Revenue Cycle VMPS principles are used in all areas of the organization, not just in clinical settings. The Finance Department began using VMPS to address outstanding revenue (revenue owed to the organization that had not been paid in a timely manner). The team improved Days Revenue Outstanding (DRO) in the clinic from 52.3 in 2003 to 29.4 in 2009 and in the hospital from 66.5 in 2003 to 42.6 in 2009. Cash deposits improved from $471 million in 2003 to $794 million in 2009. Primary Care Achieves Positive Net Margins Primary care has long been a money-losing area of health care and often a good year means breaking even. Primary care teams in VM's eight locations used VMPS to realign their work and improve the patient experience. Teams analyzed how supplies and providers "flowed" through the day. By making key changes, such as doing non-direct patient care (reviewing lab results, calling the pharmacy) in between patient visits and setting up each exam room identically with needed supplies, providers were able to see more patients in shorter work days with better quality care. Doctors, who previously stayed until 8 or 9 p.m. doing paperwork, now leave by 6 p.m. The turnaround time for lab results also improved from 25 days for normal results to two days or fewer. Today, these clinics consistently achieve positive net margins and see more patients without sacrificing time spent with each patient. Process capability Sometimes 99% is just not good enough Sigma Patient Personal Items Coding Processing Scheduling Time DPMO % Yield 3 3,660 Patients With Misplaced Personal Items Every Day 770 Coding Errors Every Day Require Correction 257 Calls Each Day Exceed The Two Minute On-Hold Time 66,800 93.32000% 4 340 Patients With Misplaced Personal Items Every Day 72 Coding Errors Every Day Require Correction 24 Calls Each Day Exceed The Two Minute On-Hold Time 6,210 99.3490% 5 12 Patients With Misplaced Personal Items Every Day 13 Coding Errors Every Week Require Correction 5 Calls Each Week Exceed The Two Minute On-Hold Time 230 99.97700% 6 6 Patients With Misplaced Personal Items Every Month During The Year, Only 10 Coding Errors Require Correction During The Year, 3 Calls Exceed The Two Minute On-Hold Time 3.4 99.99966% Most Useful Tools for healthcare (in my opinion) •Value Stream Mapping…Patient at the Centre •5 S culture •Spaghetti Diagram •Single Piece Flow versus Batching •Visual Management Examples • Increase capacity utilization of CT scanners • Pharmacy workflow • Lab workflow • ED results signaling • Pre-Op assessment • Lean theatres late start and time between cases • Asset tagging • New hospital design Pharmacy Project source: isixsigma website Pharmacy Example – 5S, VSM Pharmacy Area IV Area Lean OR process improvement - OR Turn Around Time Turn around Time flows Eliminated Waste •Reduced total time to get patient ready in OR 21% •Reduced clinician travel distance to get patient ready in OR by 54% •Reduced EVS time to clean OR by 50% Team •10 hospital team members Lean OR process improvement – Case cart pick Before Eliminated Waste •Reduced technologist travel distance by 70% •Reduced cycle time by 46% •Improved productivity by 119% After Team •9 hospital team members Lean ED Example: ED Value Stream Map Triage Express Care EKG, Draw Blood, UA, Order X-Ray, administer Pain med Front Desk X-Ray – In ED Registration If rooms full may reg pt while waiting. 2- RNs 1 Tech Fax written report/ED access via PACS Portable CT Team Area ED Waiting Room CT Fax written report MR ED MD calls before schedulin g Lab Treatment Patient Flow MD People Flow (RN, MD, etc.) E-Information flow Other Flow (blood, etc.) Phone Call Patient Wait Time Call critical values Tube/blood Registration For collection- if have White Dot Discharged (home or elsewhere) Call Report RT Nursing Unit Order Entry, Call, wait, page Respiratory Therapy Blood Gases Reg-Hospital PsychConsult Thank you.