pharmacological management of copd in patients
advertisement

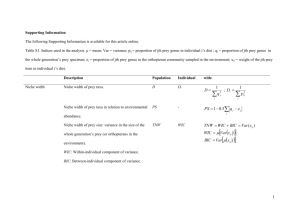
Grazie per aver scelto di utilizzare a scopo didattico questo materiale delle Guidelines 2011 libra. Le ricordiamo che questo materiale è di proprietà dell’autore e fornito come supporto didattico per uso personale. PHARMACOLOGICAL MANAGEMENT OF COPD IN PATIENTS WITH CHRONIC CO-MORBIDITIES Professor Peter Calverley University Hospital Aintree Liverpool UK A RUMSFELD MOMENT! Does having COPD influence the choice of therapy for a co-morbidity? Does taking a treatment for a co-morbidity improve the outcome in COPD? Does taking a treatment for COPD affect the co- morbidity? BETA –BLOCKERS AND COPD Good data for the benefits of selective beta- blockade in congestive heart failure, rate control of AF Longstanding worry that beta-blockade might precipitate bronchospasm So most people avoided beta-blockers in COPD Now we have evidence for safety and a reason why this is the case BETA-BLOCKERS, COPD AND VASCULAR SURGERY 1205 COPD patients, 462 receiving therapy with BB pre- surgery Van Gestel et al AJRCCM 2008 Why COPD is not asthma –bronchodilator testing is not helpful 30 Percent 25 20 15 10 5 35 30 25 Percent Smoker Controls 0 20 15 10 5 0 35 30 25 Percent Non-smoker Contr Subject Group COPD Subjects 35 20 15 10 5 0 -0.65 -0.55 -0.45 -0.35 -0.25 -0.15 -0.05 0.05 0.15 0.25 0.35 0.45 0.55 0.65 0.75 0.85 Change in FEV1 (L), Post-bronchodilator 0.95 1.05 1.15 1.25 1.35 THE STATIN STORY STATINS AND COPD OUTCOMES IN LOW RISK PATIENTS COPD/Low Risk Hospitalization 0.87 (.76, 1.0), 0.78 (.64, .95), 0.65 (.55, .78), for COPD p = .0502 p = .015 p < .0001 Hospitalization for COPD ACE Inhibitor ARB Statin 0.74 (.59, .92), p = .0062 Combination Myocardial Infarction 0.97 (.63, 1.50) 0.96 (.53, 1.73) 0.87 (.51, 1.49) 0.87 (.49, 1.54) Death 0.60 (.49, 0.52 (.38, 0.56 (.42, 0.38 (.27, .73), .72), .74), .54), p p p p < < < < ACE Inhibitor ARB Statin Combination ACE Inhibitor .0001 .0001 .0001 .0001 ARB Statin Combination (.59, (.49, (.51, (.36, .85), .84), .83), .66), p p p p = = = < 0.0 (.84, (.78, (.67, (.62, .99), .96), .81), .80), p p p p = = < < .0260 .0056 .0001 .0001 Myocardial Infarction 1.17 (.90, 1.52) 1.10 (.79, 1.54) 0.85 (.61, 1.18) 1.27 (.90, 1.78) Death 0.73 (.65, 0.55 (.46, 0.51 (.43, 0.35 (.28, .83), .66), .62), .44), p p p p < < < < .0001 .0001 .0001 .0001 Myocardial Infarction or Dea Myocardial Infarction or Death 0.71 0.64 0.65 0.49 0.91 0.86 0.74 0.70 ACE Inhibitor .0002 .0011 .0006 .0001 ARB Statin Combination 0.5 1.0 1.5 0.82 0.68 0.64 0.48 (.73, (.58, (.55, (.40, 2.0 Risk Ratio Mancini et al JACC 2006 .92), .80), .75), .58), p p p p = < < < 0.0 .0008 .0001 .0001 .0001 STATINS AND EXACERBATIONS Mortenson E et al Respir Res 2009 Angina Acute coronary syndromes Systemic Effects of COPD: Target Organs Lung Infections Lung Cancer Weight loss Muscle weakness Diabetes Metabolic syndrome Osteoporosis Peptic ulceration/reflux Systemic Inflammation Oxidatitive Stress From W MacNee Depression Depression TREATMENT AND COMPLICATIONS Depression –common, often associated with fatigue. Interaction with therapy more likely with systemic treatment. Corticosteroids possibly – roflumilast unproven Reflux – GI issues with theophyllines and PDEIV inhibitors Metabolism and diabetes –ocs associated with hyperglycaemia but this is a feature of acute exacerbations. More data from roflumilast Muscles Most frequently reported AEs COPD safety pool placebo rof500 (N=5,491) (N=5,766) (%) (%) 62.8 67.2 COPD exacerbations 23.1 19.8 Diarrhoea 2.6 10.1 Weight decreased 1.8 6.8 Nasopharyngitis 6.3 6.3 Nausea 1.4 5.2 Headache 2.0 4.6 Upper respiratory tract infection 4.3 3.8 Bronchitis 3.5 3.1 Back pain 2.1 3.1 Insomnia 0.9 2.6 Influenza 2.4 2.5 Dizziness 1.2 2.4 Decreased appetite 0.4 2.2 Pneumonia 2.0 1.8 All AEs PHARMACOLOGICALLY PREDICTABLE EFFECTS Nausea Events in the category Events in the category (%) Diarrhoea <1 week ≥1 week ≥4 weeks ≥13 weeks ≥26 weeks to <4 to <13 to <26 weeks weeks weeks <1 week placebo (n=5491) rof 500 mcg (n=5766 ET=number of patient-years of exposure ≥1 week to <4 weeks ≥4 weeks to <13 weeks ≥13 weeks ≥26 weeks to <26 weeks Weight loss Noted as a self-reported finding more often with roflumilast Not just confined to patients reporting GI intolerance Monitored with regular weight measurement in pivotal one year trials In one 6 month study bioimpedance data were available Body weight over time in the studies with available data 4 placebo roflumilast 500µg 2 = -2.17 kg 0 (CI –2.4;-1.9) p < 0.0001 -2 -4 0 8 16 24 Weeks Timecourse: Mean change in kg Between Treatment Differences least-squares means from ANCOVA 32 40 48 Weight change by BMI Percent weight change from baseline to end of treatment by BMI at baseline: pivotal COPD studies pool (SAF) Placebo Mean Change (%) Rof500 N= 127 134 Underweight 605 572 Normal 462 475 Overweight 316 317 Obese Weight loss associated with roflumilast was primarily fat mass Tiotropium + placebo (BMI) Mass indices [kg/m2] 0 Tiotropium + placebo (FFMI) Tiotropium + Daxas® (FFMI) -0.5 Tiotropium + Daxas® (BMI) -1 0 4 8 12 16 20 24 Weeks Wouters EFM, Teichmann P, Brose M, et al. Am J Respir Crit Care Med 2010;181:A4473. FFMI: Fat Free Mass Index; BMI: Body Mass Index MUSCLES Loss of muscle bulk vs weakness A marker for more health care expense and mortality but the thresholds may vary A clear relationship of weakness to ocs use long term –not seen with ics Anabolic steroids reverse this process but only in people taking oral corticosteroids (Kreutzberg E et al) BONES AND INHALED CORTICSTEROIDS Database associations but confounded by disease severity TORCH - Time to First Fracture Safety Population Plc N=1544 SAL N=1542 FP N=1552 SFC N=1546 Non-Traumatic 20 (1.3%) 29 (1.9%) 21 (1.4%) 21 (1.4%) Traumatic 39 (2.5%) 37 (2.4%) 45 (2.9%) 58 (3.8%) KM Prob at 3 years 5.1% 5.1% 5.4% 6.3% Hazard Ratio 95% CI p SFC vs Placebo 1.22 (0.87, 1.72) 0.248 SFC vs SAL SFC vs FP 1.23 1.16 (0.88, 1.72) (0.83, 1.61) 0.229 0.382 SAL vs Placebo FP vs Placebo 1.00 1.06 (0.69, 1.43) (0.74, 1.51) 0.977 0.765 Prevalence of Osteoporosis & Osteopenia at Baseline % patients 50 40 30 20 10 0 Placebo SALM 50 FP 500 SFC 50/500 T score < -1 and > -2.5 for hip or spine: osteopaenia T score < -2.5 for hip or spine: osteoporosis US Safety sub-study : percent change in total hip BMD Adjusted mean change BMD hip 1 0 –1 –2 –3 –4 Placebo SAL FP SFC –5 0 48 108 158 72 82 80 95 52 78 65 82 Time (weeks) Number of subjects 161 162 158 162 Vertical bars are standard errors 87 105 112 118 Ferguson et al Chest 2009 Time to First Pneumonia AE Probability of Event (%) 12 11 10 9 8 7 6 5 4 3 2 1 Number 0 at Risk Probability of event prior to wk 104 SFC 9.9% TIO 5.5% Treatment TIO 18 SFC 50/500 656 664 550 543 511 497 491 468 470 4242 451 426 426 405 415 387 150 136 0 13 26 39 52 65 78 91 104 Time to Event (Weeks) SFC vs TIO Cox Hazard Ratio 1.94 95% CI (1.19, 3.17) p-value 0.008 SFC 50/500 TIO 18 TIME TO FIRST PNEUMONIA AE OR SAE Sin et al Lancet 2009 Cardiovascular Events with Tiotropium Composite Endpoint* Used by Singh et al applied to UPLIFT Placebo Tiotropium Rate Ratio1 (95 % CI) n Rate2 n Rate2 Composite endpoint 246 2.89 208 2.25 0.78 (0.65, 0.94) Fatal composite 124 1.42 98 1.04 0.73 (0.56, 0.95) UPLIFT 1 rate ratio tio vs. placebo; 2per 100 person-years of time at risk to tiotropium or placebo *SOC cardiac (fatal), SOC vascular (fatal), MI (fatal+nonfatal), stroke (fatal+nonfatal), sudden death, sudden cardiac death All-cause mortality at 3 years Probability of death (%) 18 16 14 12 10 8 6 4 Placebo SALM FP SFC 2 0 0 12 24 36 48 60 72 84 96 108 120 132 144 156 Time to death (weeks) Number 1524 alive 1533 1521 1534 Vertical bars are standard errors 1464 1487 1481 1487 1399 1426 1417 1409 1293 1339 1316 1288 Calverley et al. NEJM 2007 CARDIOVASCULAR EVENTS AND THERAPY Calverley et al Thorax 2010 CVS TREATED COPD AND THERAPY Calverley et al Thorax 2010 Time to onset of first major adverse CV event (MACE*) Probability of event 0.04 roflumilast 500 mcg, od, p.o. + roflumilast 250 mcg, od p.o. placebo, od, p.o. 0.03 0.02 0.01 0.00 0 30 60 90 120 150 180 210 240 270 300 330 360 390 Days post-randomisation MACE : CV death, non-fatal MI, non-fatal stroke CONCLUSIONS Beta–blockers and other cardiac drugs are safe in COPD Statins may improve COPD outcomes but proper trial data are needed Oral therapies produce more GI upset, oral corticosteroids long term are hazardous Inhaled corticosteroids do not seem to accelerate osteoporosis but some may induce pneumonia LAMA and LABA treatment is safe in COPD – antiinflammatory therapy may improve cardiac outcomes On balance our treatments are more friend than foe