Using health datasets to improve the coordination of medical
advertisement
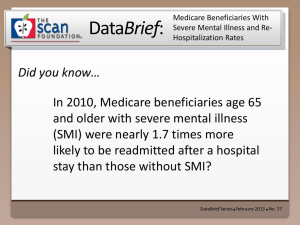
Using Healthcare Data Sets to Improve the Coordination of Medical and Behavioral Health The Potential Role For Health Homes Richard Surles, Ph.D. YAI International Conference New York Hilton, New York, NY May 2013 Agenda Understanding & Aligning Data Sets to Optimize Care and Control Costs Potential Use of Data Sets to Identify Members and Needs Leveraging Data Sets to Drive Workflow in Support of Effective Medical Homes 2 Complex Conditions Require New Ideas for Coordination Beyond Traditional Medical Management ~50% of People Who Have a Severe Mental Illness (SMI) Have Medical Comorbidities – Higher rates of utilization and costs – Problems achieving desired treatment outcomes – Lack of access to integrated services Major Issues in SMI Overall Care are Medication Management and Suboptimal Care Delivery combined with the Need for Non-medical Support Services Proven Interventions – Communication between mental health and physical health providers to provide integrated care – Use of information systems (tracking RX refills, clinical visits) to promote patient adherence and improved outcomes – Targeted interventions for both patient self care and provider engagement are critical – Care Management program engagement goals: decrease isolation, promote access – Relapse prevention programs contribute to medication maintenance, increased patient self-monitoring of symptoms 3 SMI and Medical Comorbidities in ABD* Population 39% of Population Has a SMI SMI Participants Account for 58% of Total Costs Non-SMI 42% SMI 39% SMI 58% Non-SMI 61% Top 5% of SMI Population Account for ~25% of All Costs 100% $321 M 80% $778 M 60% 40% 20% 0% Number of Participants 118,681 Non SMI SMI 75% spend SMI 75-90% *Aged, Blind & Disabled 4 Total Costs $1.34 B SMI Top 10% Levels of Complexity for Aged, Blind & Disabled ABD Medicaid Spend Category Differences by Acuity (10/10-9/11) PMPM – – – 36,408 1.8 4.9 7.1 Low: Mod: High: 1.9 5.2 10.7 Average MDs – – – $582M Low: Mod: High: Average Risk Score (CDPS)* – – – $679.94 $3,471.14 $8,262.26 Average Number of Conditions – – – Low: Mod: High: Low: Mod: High: 3.3 6.6 10.9 * Chronic Illness & Disability Payment System; Index risk score is 1.0 5 ABD Population – Prevalent BH + Chronic Medical Top 20% ABD Population (n = 7,282) Low Back MuscSkel SCHIZ Sleep Sub Abuse 16.4% 40.8% 50.1% 21.0% 15.1% 33.5% 15.9% 14.1% 38.3% 47.0% 25.8% 14.5% 34.5% 27.9% 18.8% 20.7% 41.3% 49.8% 18.8% 16.7% 32.1% 41.9% 23.7% 15.9% 17.7% 28.3% 38.8% 13.7% 11.2% 28.1% 52.7% 17.5% 14.9% 18.8% 44.6% 47.0% 20.7% 11.4% 18.5% Depress Diabetes Hyper- Hyperlipidimia tension Anxiety Asthma Bipolar COPD Anxiety 28.4% 16.2% 44.8% 16.7% 53.1% 22.2% 15.9% Bipolar 53.8% 14.4% 23.6% 13.5% 49.2% 20.5% Depress 49.6% 13.7% 38.2% 17.0% 30.4% SCHIZ 43.7% 11.7% 44.6% 15.6% Sub Abuse 51.4% 13.6% 44.1% 20.0% 6 Dimensions of Care - Supporting the Whole Person How Treatment is Delivered Intensive/Procedural Medical Treatment Rehabilitative Treatment Combined Treatment Patient Education & Counseling Self-Help & Natural Supports What is Treated Marital/Familial Vocational/Financial Social/Legal Intrapsychic Biomedical Hospital Home Office Community Partial Care Where Treatment is Done 7 Medical Services Community Services Clinical Supports Inpatient Hospital Outpatient Hospital Critical Access Hospital FQHC Skilled Nursing Home Health Rural Health Clinic Other Medical Ambulance Office Visits Specialists Lab Tests Comprehensive Medication Service Minor Procedures Anesthesia Major Procedures ER Visits Other Tests Residential Facility Intermediate Care Habilitation Other Supports Alcohol/Drug Treatment Community Wrap-Around services Community Support Services Case Management Personal Care Non-emergency Transportation BH Day Treatment Attendant care Psychosocial Rehabilitation Crisis Intervention Assertive Community Treatment Other DME Supported Employment 8 Are Integrated SMI Health Homes a possibility? Affordable Care Act Encourages the Use of Health Homes for Chronically Ill and People with SMI via Financial Incentives SMI Health Homes Addresses Behavioral Health Needs While Responding to Other Healthcare Issues – Individuals with SMI, on average, die 25 years earlier than the general population – 60% of premature deaths in persons with schizophrenia are due to medical conditions such as cardiovascular, pulmonary and infectious diseases – Second generation anti-psychotic medications are highly associated with weight gain, diabetes, dyslipidemia (abnormal cholesterol) and metabolic syndrome 9 Key Features of the Health Home: All Data Driven Feature Purpose Comprehensive care management • Predictive Modeling and Disease Stratification to identify clients with chronic disease and pinpoint risk • Technology that integrates settings of care and data sources • Secure messaging for information sharing and coordination Monitoring • Enhances clinical care by alerting team to client events and changes in client status • Addresses both clients and providers • Supports innovative payment systems Reporting & Quality • Easily accessible performance reports on key measures at multiple levels – client, provider, region, and state • Quality improvement program for structured initiatives Outcome Measurement • Stabilization of acuity and reduction of symptoms • Clinical performance – engagement, medication adherence, reduction of ER, Inpatient, Readmissions • Return on Investment analysis 10 A Vision of Provider Data Support Systems Medical Home Has Current and Complete Information Via the Integrated Technology Platform – Data Driven Plan of Care – Aggregate view of all services/billing/interactions Provider Tools – Real time access to data via secure Provider Portal – Reports highlighting alignment to best practice, gaps in care, services received outside of Medical Home • Patient Specific Information • Provider panel aggregate information Service Vendor Requirements – Integrated technology platform – Technical assistance and training – Community and telephonic member engagement – Engage providers for care coordination – Appointment tracking and follow up 11 James R: A Member Case Study of Integration 47 Year Old Male with CAD, Diabetes, HTN, Asthma, Hyperlipidemia, GERD, Bipolar Disorder – New enrollee at program “go live” – Gaps in care analysis triggered (IP, multiple ER), General Assessment identified positive PHQ-2 and housing issues Issue – Ineffective medical home – Unstable diabetes and behavioral health conditions – Unstable housing Model Intervention – Secured stable housing – Secured effective medical home – Transitioned from Telephonic Health Coach to Field Health Coach intervention 12 James R: Member Case Study Assessments Provide Additional Information 13 James R: Member Case Study 14 Changing the Dialogue: Data Driven Systems of Care “Health Care Home” HCH IDENTIFY > Data Driven, Predictive Modeling >Data analysis >Assessments INTERVENE EVALUATE >Facilitate access to care & service supports >Improve selfmanagement skills Measure goal progress >Feedback on results MONITOR Engaged, educated member >Informed HCH >Alert system for HR/HC potential “Provider – Clinical, Service & Community Support and Tools” 15 The Finish: Issues for a Data Driven Health System Access and Quality of Data Privacy and Consumer Consent Coordination of Medical and Behavioral Care with Pharmaceuticals Full integration of traditional Medical Managed Care with Non-traditional Community Support Services Including: – – – – Psychosocial Rehabilitation Habilitation Personal Care Other Home and Community Care Services 16