Extended Release Naltrexone - Nysam
advertisement

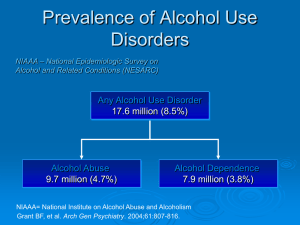
Extended Release Naltrexone: Current Evidence Joshua D. Lee MD MSc joshua.lee@nyumc.org Assistant Professor NYU School of Medicine NYSAM, NY, NY FEB 5 2011 Financial Support to Dr. Lee •NIDA •Alkermes Inc (Investigator Sponsored Studies) •NYU School of Medicine XR-NTX Evidence Base •Alkermes, Biotek Inc •NIAAA, NIDA Outline •Oral naltrexone –Alcohol Disorders –Opioid Treatment –Strategies to improve naltrexone adherence •XR-NTX for alcohol dependence •XR-NTX for opioid dependence •Practical considerations, dissemination and implementation Neurochemical Circuits Involved in Alcohol and Opioid Dependence: Naltrexone reduces dopaminergic tone of alcohol and opioid use Mechanisms of action of naltrexone: Reduces acute dopamine release at nucleus accumbens Reduces craving during non-drinking periods 1. Anton RF, NEJM 2008;359 (7): 715-721. Oral Naltrexone Evidence Base: efficacious, but effective? • Mu, delta, kappa opioid receptor antagonist – Synthesized 1963, patented 1967 Endo Labs – Opioid dependence, Trexan, 1984, Dupont – Alcohol dependence, ReVia, 1994, DuPont • Efficacious in RCTs of alcohol dependence • Effectiveness less clear • Poor daily adherence a clear issue in all studies • Dissemination never very broad Naltrexone Efficacy in St. Kitts Rhesus Monkey and Human Laboratory Studies Altshuler HL,1980, Alteration of ethanol self- administration by naltrexone. Life Sci. 26: 679–688. Oral Naltrexone (NTX) as Treatment for Alcohol Dependence Clinical Trials and Systematic Reviews, 2000-2010: Mixed Messages • VA multi-site NTX trial (Krystal 2001) – Oral naltrexone plus 12-step facilitation not effective vs. placebo in reducing drinks per drinking day or time to relapse – Oral naltrexone compliance at 12 and 48 weeks was low: 72% and 44% – Placebo arm did fairly well – all participants substantially reduced drinking • Cochrane meta-analysis of 29 RCTs (Srisurapanont, Jarusuraisin 2004) – Supports short-term NTX treatment – Number needed to treat = 7 • COMBINE Trial (Anton 2006) – NTX plus Medical Management effective vs. placebo in reducing time to heavy drinking – Mu-opioid ‘G’ allele (Asp40 homo/heterozygotes) predicts NTX response – Greater response in males (v females) – Greater response in participants w pre-treatment abstinence – COMBINE oral naltrexone adherence 72% overall across all NTX arms – 100mg daily dose of naltrexone (vs. 50mg) Oral Naltrexone: Poor Real-World Adherence Panel 1B: Oral naltrexone refills from a multicommercial insurer database. (Kranzler 2008) Panel 1A: Months of disulfiram and oral naltrexone in NE VAs. (Hermos 2004) Panel 1C: Oral naltrexone refills across three consecutive 1year periods. (Harris 2004) Naltrexone adherence enhancement: behavioral counseling or XR formulation • Behavioral enhancement: – Medical Management model • Information/teaching • Encouragement and motivational enhancement • Biomarkers (AST/ALT, GGT, CDT) – Naltrexone-specific adherence enhancement • Mild treatment effect • Sustained Release Formulations – Naltrexone implants (Australia, Europe, US) – Extended-release injectable naltexone (XR-NTX) XR-NTX Development, 1970s-2006 • NIAAA/NIDA support from 1970s-2000s for drug development • Poly-lactide glycolide (PLG) architecture • No first-pass metabolism – Increased naltexone vs. 6betanaltrexol hepatic metabolite • 380mg vs. 1500mg / month • Continuous vs. pulse dosing XR-NTX Efficacy: Garbutt Vivitrol (Vivitrex) Pivotal Trial, 2005 • 6 Months of XR-NTX 380mg, 190mg, and Placebo – Mostly (84%) white men, mean age 45 (19-74) – 20 heavy drinking days/month – 9% lead-in abstinence – 74% of pts got 4+ injections. • Outcomes: – Sig difference in heavy drinking days/month for high dose • HR: 0.75 OVER 6 MONTHS • @ 30days 6 vs. 9 fewer days of heavy drinking • @ 60days 18 vs. 26 – Significantly better outcomes in subgroup w lead-in abstinence – Outcome of complete abstinence: 7% at 380mg (vs. 5%, placebo) GarbuttJ, KranzlerH, O’MalleyS, JAMA, 2005 Garbutt Vivitrol Pivotal Trial, 2005: 25% Reduction in Heavy Drinking XR-NTX: Lead-in Abstinence • Lead-in abstinence 9% of study population, did exceptionally well on Vivitirol 380mg • All arms received 12-session low intensity psychosocial therapy • FDA Labelling, 1996, Vivitrol: alcohol dependent patients who are able to abstain from alcohol prior to treatment initiation, as part of a comprehensive management program that includes psychosocial support XR-NTX Pivotal Alcohol Trial: other findings • Women (15%): no difference vs placebo • Holiday drinking: sig. reduction among lead-in abstinent, 380mg Vivitrol participants • Adverse Events: 14% vs. 7% (placebo) d/c of treatment – 200 severe injection site reactions nationally – No hepatic toxicity – Acute pain control a general concern XR-NTX Effectiveness: what about the ‘real world’? • NYU/Bellevue (Lee 2010): XR-NTX Alcohol Primary Care Medical Management – 62% monthly retention at 3 months • Portland, ME (Publiker 2010): XR-NTX at detox discharge among homeless patients – 2.3 months of XR-NTX – Fewer ER, greater outpatient MH/PC visits post-detox • San Francisco VA (Batki 2007): XR-NTX vs. Oral NTX among severely mentally ill alcoholics (schizoph., bipolar) – 80% monthly retention at 3 mos (40% O-NTX adherence) LeeJD, GourevitchMN, et al, Journal of Substance Abuse Treatment, 2010 Prescreened, N=116 Adult Alcohol Dependent (DSM-IV), N=76 Eligible, N=72 Ineligible, n=4 LFTs >3x nl (2), opioid dep (1), psych (1) 1st Injection No 1st injection, n=7 n=65 Changed mind (3), lost-to-follow-up (4) 2nd Injection No 2nd Injection, n=16 n=49 Lost (10), side effects (3), no effect (3) 3rd Injection No 3rd Injection, n=9 Lost (5), AEs (2), no effect (1) n=40 Month 4 Follow-up n=28 12-month extension study, n=19 XR-NTX Alcohol Treatment at NYU/Bellevue • XR-NTX appears effective for Primary Care medical management of alcohol dependence Treatment Retention 1 1 0.9 0.89 0.8 0.69 0.6 Drinking rates in treatment 0.56 0.5 30 0.4 0.3 25 0.2 0.1 20 0 Baseline 1st Injection 2nd Injection 3rd Injection # Proportion 0.7 20 Drinking Days / Month 15 # Drinks / Drinking Day 12 10 56% of patient stayed in treatment 90 days Daily drinking reductions were robust and seen within the first month 6 5 7 5 6 4 0 Baseline Month 1 Month 2 Month 3 1st 2nd 3rd Injec tion Injec tion Injec tion LeeJD, GourevitchMN, et al, Journal of Substance Abuse Treatment, 2010 XR-NTX Long-term Retention • Garbutt 2005 and Alkermes open-label extension study – – – – – 74% at 4 months 64% at 6 months 56% at 7 months in an extension study offering 18 months 24% completed 18 injections 10% continued for 3-4 years Bellevue/NYU 2010: 56% at 3 months, ~50% elected to continue treatment x 12 months Proportion Retained in Treatment Through Month 15 (N=19) 1.00 1.00 0.90 0.89 0.80 0.72 0.70 0.67 0.61 0.60 0.50 0.50 0.50 0.40 0.39 0.33 0.33 0.30 0.20 0.17 0.10 0.06 0.00 Dose 4 Dose 5 Dose 6 Dose 7 Dose 8 Dose 9 Dose 10 Dose 11 Dose 12 Dose 13 Dose 14 Dose 15 XR-NTX Alcohol Treatment: Translation, Dissemination, Cost-Effectiveness • XR-NTX and all alcohol meds remain poorly prescribed – 16-17% of U.S. substance abuse treatment facilities report using any alcohol medication (disulfiram, acamprosate, O/XRnaltrexone) – ~170,000 individual alcohol medication prescriptions, 2009 – 10-20 million U.S. with alcohol use disorders • How to expand the use of these medications – Comparative Effectiveness: are they better than med-free treatment? – Are they cost-effective? Tami L. Mark PhD (Thompson Reuters Inc.), AHSR 2009, supported by Alkermes, Inc. Characteristics and Outcomes of Insured Patients Treated with XR-NTX or Oral Alcohol Dependence Medications MarketScan Jan 2006 – Dec 2008 XR – NTX NTX Acamprosate Disulfiram (295) (2,064) (5,068) (2,076) Alcohol Dependence Dx No Rx (17,632) Alcohol Use Disorder In the Pre-period Any Rx (4,047) Tami.Mark@Thomsonreuters.com (301) 214 - 2211 Alcohol Use Disorder In Pre-period No Rx (4,730) Inpatient Days per 1,000 Patients 1,400 *** 1,163 Days per 1,000 Patients 1,200 *** 1,086 967 1,000 800 862 706 650 600 400 200 0 Detoxification *** P < 0.01 Alcohol-Related Inpatient Alcohol Rx Other Inpatient No Alcohol Rx 21 Charges for Detoxification Days Per 1,000 Patients (vs. XR-NTX) $1,600,000 *** *** $1,400,000 $1,200,000 * $1,000,000 $800,000 $600,000 $400,000 $200,000 * P< 0.1 $0 ** P< 0.05 XR-NALTREXONE ORAL NALTREXONE DISULFIRAM ACAMPROSATE ***P < 0.01 Charges for Principal Alcohol Dx Inpatient Days Per 1,000 Patients (vs. XR-NTX) $1,400,000 *** $1,200,000 *** $1,000,000 $800,000 $600,000 $400,000 $200,000 * P< 0.1 $0 ** P< 0.05 XR-NALTREXONE ORAL NALTREXONE DISULFIRAM ACAMPROSATE ***P < 0.01 Aetna Data, N=2204 7% of 78,000 patients with alcohol use disorders Non-specialty settings Addiction and MH settings Proportion of Population Reached Intensity of Treatment Provided De-fragmenting Care with Medications: Paradigm for the Medical Home? SUBSTANCE ABUSE CO-LOCATED CARE PRIMARY CARE MENTAL HEALTH NIAAA Clinician’s Guide: Medical Management Proposed Study (NIAAA): A Randomized Comparative Effectiveness Trial to Evaluate XR-NTX vs. O-NTX for Alcohol Dependence in Primary Care XR-NTX Alcohol Treatment Questions? Next: Opioid Treatment Current U.S. Opioid Treatment Methadone: 220,000 treatment slots Buprenorphine: 500,000 prescriptions Naltrexone: ? XR-NTX Opioid Treatment, Comer 2006: better retention, less relapse to sustained opioid use Retention in treatment XR-NTX Opioid Treatment, Comer 2006: Less opioid and other drug use Urine Toxicology Results XR-NTX Vivitrol Opioid Treatment Pivotal Trial: KrupitskyE 2010 (APA 2010, FDA 2010) •24 week double-blind, placebo-controlled, randomized trial following inpatient detox, N=250 •Russia, no agonist TAU alternative •Clear superiority vs. placebo at preventing lapses and sustained relapse/dependence •No ODs or deaths •FDA approval of Vivitrol for opioid depencence Oct 2010 Office-Based Buprenorphine in Bellevue Primary Care Retention in Treatment: 50% at 6 months On-going Opioid Use: High rates of on-going, ‘low-grade’ opioid use XR-NALTREXONE FOR TREATMENT OF OPIOID DEPENDENCE DURING PAROLE/PROBATION Adult parole/probation, history of opioid dep., N=400 RCT 5 sites XR-NTX Treatment as usual Relapse 6 month treatment phase Re-incarceration Cost-benefit 6, 12, 18 month f/u NIDA 1R01DA024555-01A1 2008-2013 (Lee JD, PI) XR-Naltrexone for treatment of opioid dependence at release from NYC JAILS Adults in NYC jail, not seeking addiction treatment (N=40) Randomization XRNaltrexone Relapse Overdose JAIL Treatment as usual Follow-up: 1 week post-release Bellevue Primary Care Follow-up: 1 month post-release Re-incarceration Saperstein Medical Fellowship, NYUMC Center of Excellence Seed Grant, Alkermes ISS XR-NTX Opioid Treatment In CJS Populations • Multisite pilot study using Depotrex – N=60 opioid dependent persons on parole – Fewer positive urines and fewer arrests if retained in treatment • Multisite N=400 RCT of parole/probationers randomized to XR-NTX vs. TAU – Robust retention in treatment to date – Not recruiting current daily, heavy opioid users • MO and NM: DUI pilots appear successful XR-NTX Opioid Treatment: Experience to Date • Outpatient induction has been among detoxed patients only at our sites • Other national sites piloting induction strategies – Buprenorphine/clonidine/oral naltrexone/IVFs/benzos • Induction of actively using (urine +) patients in primary care likely very difficult XR-NTX Beyond Opioids and Alcohol: Potential Benefits of Mu Opioid Blockaide • NIDA CTN 0048 ‘CURB’ Trial: cocaine dependence • • • • XR-NTX mu opioid blockade + buprenorphine for kappa antagonism Amphetamine dependence Weight loss Smoking cessation Gambling Thank You • Questions? • Copy of presentation: joshua.lee@nyumc.org