Dr Warren Shattles - Fibromyalgia
advertisement
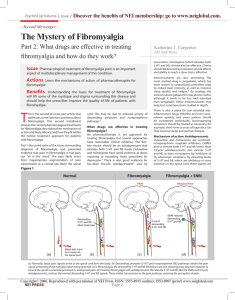
FIBROMYALGIA FIBROMYALGIA • 1ST defined by ACR criteria1990 • Pain is considered widespread when all of the following are present: pain in the left side of the body, pain in the right side of the body, pain above and below the waist. In addition, axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back) must be present. Shoulder and buttock pain is considered as pain for each involved side • Pain in 11 of 18 tender points on digital palpation (4kg force), must be described as painful, not tender • Widespread pain must have been present for at least 3 months Fibromyalgia • Redefined by ACR 2010 without emphasis on tender points: • A patient satisfies criteria if the following 3 conditions are met: • 1 Widespread Pain Index (WPI) of at least 7 and symptom severity scale score (SS) at least 5, or WPI 3-6 and SS scale at least 9 • 2 Symptoms present at a similar level for at least 3 months • 3 The patient does not have another disorder that would otherwise explain the pain Fibromyalgia: WPI • Note the number of areas in which the patient has had pain over the last week. In how many areas has the patient had pain? Score between 0 and 19 • • • • • • • • Shoulder girdle, L and R (2) Upper arm L and R (2) Lower arm L and R (2) Hip (buttock, trochanter ) L and R (2) Upper leg L and R (2) Lower leg L and R (2) Jaw L and R (2) Chest Abdomen Upper back Lower back neck Fibromyalgia SS scale score • • • Fatigue Waking unrefreshed Cognitive symptoms • For each of the 3 symptoms, indicate the level of severity over the week using the following scale: 0 no problem 1 slight or mild problems, generally mild or intermittent 2 moderate, considerable problems, often present and/or at a moderate level 3 severe, pervasive continuous, life disturbing problems Considering somatic symptoms in general, indicate whether the patient has 0 no symptoms 1 few symptoms 2 a moderate number of symptoms 3 a great deal of symptoms SS scale score is the severity of the 3 symptoms (fatigue, waking unrefreshed, cognitive symptoms) plus the severity of somatic symptoms, final score between 0 and 12 • • • • • • • • • • Fibromyalgia Somatic Symptoms • Muscle pain, irritable bowel, fatigue/tiredness, thinking or remembering problem, muscle weakness, headache, pain/cramps in the abdomen, numbness/tingling, dizzyness, insomnia, depression, constipation, pain in the upper abdomen, nausea, nervousness, chest pain, blurred vision, fever, diarrhoea, dry mouth, itching, wheezing, Raynauds, hives/welts, ringing in the ears, vomiting, heartburn, oral ulcers, loss of/change in taste, seizures, dry eyes, shortness of breath, loss of appetite, rash, sun sensitivity, hearing difficulties, easy bruising, hair loss, frequent urination, painful urination, bladder spasms Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management • 46 recommendations • FM represents a composite of symptoms, with body pain present as the pivotal symptoms. There is a spectrum of severity which associates with functional outcome, and fluctuating symptoms over time. • Diagnosis is clinical, not one of exclusion, not one requiring specialist confirmation, and requires limited laboratory testing. A physical examination is required to exclude other conditions presenting with body pain, but tender point examination is not required to confirm the diagnosis. Excessive laboratory testing is strongly discouraged • Ideal care is in the primary care setting and should be multimodal Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management • Focus on non pharmacological and pharmacological strategies to reduce symptoms and improve function • Patient must be an active participant • No ideal pharmacological treatment • Emphasis on healthy lifestyles, maintenance of function including retention in the workforce, periodic reassessment re need for continuing any medication, side effects of treatments and new symptoms Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management • • • • • • Pain Fatigue Nonrestorative sleep Cognitive dysfunction Mood disorders Pain related somatic symptoms (irritable bowel, migraine, headaches, severe menstrual pain, lower urinary Tract symptoms, myofascial pain, TMJ pain) • Non-pain related symptoms (sexual dysfunction, increased risk of post traumatic stress disorder) Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management • Dysaesthesia (sensitivity to light touch) • Allodynia (unpleasant sensation or pain after a non-painful stimulus) • No objective neurological findings • Expression of pain or pain behaviours may be present but should not imply faking of symptoms Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management • FBC • ESR CRP • TSH • CPK • Low Vit D level supplementation has no effect on FM pain • Low titre ANA present in around 10% and should only be tested on specific clinical suspicion Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management: DD • • • • • • • • Hypothyroidism Early inflammatory arthritis or CTDs PMR Myositis Multiple sclerosis Neuropathies Myopathies Drugs: statins, aromatase inhibitors, bisphophonates • Remember that FM can co-exist with other conditions Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management: Causes • Unknown • Abnormalities in pain processing at peripheral, central and sympathetic NS and hypothal-pitadrenal levels • Changes on functional MRI and SPECT brain scans, increased substance P in the CSF • Family studies suggest some genetic predisposition with up to 26% relatives reporting widespread pain, but no clear gene associated with FM • Psychosocial distress can predict onset Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management: Management • No cure • Education and reassurance of no harm with physical activity • Good social support and healthy lifestyle • Treatment of psychological stress including group therapy, motivational interviewing eg spaced phone calls to encourage exercise regimes, CBT • Distraction therapy Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management: Management • No evidence for alternative medicines including acupuncture, chiropractic manipulations Fibromyalgia: 2012 Canadian Guidelines for diagnosis and management: Management • Paracetamol never formally examined • NSAIDs tried • Tramadol showed positive effects on pain and quality of life • No convincing evidence of benefit from codeine, but often tried • Strong opioids not recommended • Tricyclic antidepressants • SNRI’s: duloxetine 60-120mg/day • gabapentinoids RHEUMATOID ARTHRITIS Aggressive regimes have long replaced the old treatment paradigm of 6 months NSAIDs then cautious introduction of DMARDs NICE recommend combination therapy from the beginning, including steroids BNF outdated as says drugs are contraindicated together due to potential drug interactions Preference for 2 DMARDs with steroid initially, trying to phase out steroids over several months, but patients often resistant to such initial polypharmacy RA DMARDs • • • • • • • • Methotrexate (MTX) oral or sc (to 30mg) Sulfasalazine (SSZ) Leflunomide Hydroxychloroquine Azathioprine (Aza or AZT) Ciclosporin Gold (IM) Penicillamine RA disease assessment • DAS 28 is the currently accepted European wide (and NICE) disease score • 28 tender joints • 28 swollen joints • ESR or CRP • Patient VAS • Complicated formula requires a special calculator RA disease assessment • CDAI: Clinical Disease Activity Score • • • • • 28 tender joints 28 swollen joints Patient VAS Physician VAS Add swollen and tender score to the 2 global scores (0-10 each) • Range 0-76, <10 is low activity, 10.1-22 is moderate, 22.1-76 high activity RA disease assessment • SDAI: Simplified Disease Activity Index • • • • • • Numerical sum of the following 5 scores: 28 tender joints 28 swollen joints Patient VAS (0-10) Physician VAS (0-10) CRP in mg/dl ie normal <1mg/dl RA: Biologics • Anti-TNFs: • • • • infliximab (IV) etanercept adalimumab certrolizumab golimumab best response when used with MTX (or another DMARD) but all but infliximab can be used alone RA: Biologics • Rituximab: anti-CD20 • best response if RF or • anti-CCP positive • recommended with MTX • 2nd choice in NICE guidance • unless RF/CCP negative • only funded if response>6/12 • RA: Biologics • TOCILIZUMAB • • • • Anti-IL-6 Best data on use without DMARD NICE accept it as potential 1st biologic Currently only allowed locally 1st if MTX intolerant R: BIOLOGICS • ABATACEPT • Fusion protein (Fc of IgG1 fused to extracellular domain of CTLA-4) • CTLA-4: Cytotoxic T Lympocyte Antigen 4 (or CD152) is found on surface of helper T cells and down regulates T cells Similar to CD28 which is a co-stimulatory protein activateingT cells through binding to CD 80 and CD 86 • Abatacept binds to CD80 and CD86 on APC with higher affinity and thus inhibits the co-stimulation of T cells