Fibromyalgia - Weber State University
advertisement

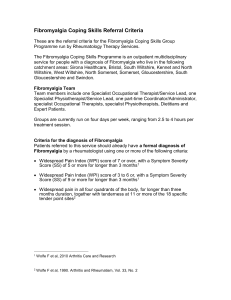
Fibromyalgia Justin Hogge Definition of Fibromyalgia A common clinical syndrome of generalized musculoskeletal pain, stiffness, and chronic aching characterized by reproducible tenderness or palpation of specific anatomical sites, generally referred to as tender points. Dr. Joe M. Elrod Tender Points Tender Point Count and Intensity Can vary from day to day The degree of tender points tends to predict functional limitation. But, the correlation is very far from perfect. Individuals with less than 11 of 18 of these tender points may still have severe functional limitations. (Chronic Pain Syndrome.) The cut-off between “fibromyalgia” and “chronic pain syndrome” is somewhat arbitrary Epidemiology An estimated 5 to 10 million people in the United States are diagnosed with Fibromyalgia. 80-90 percent of diagnosed fibromyalgics are said to be women between 20 and 55 years of age but the number of younger people with fibromyalgia is growing. Symptoms Anxiety and/or panic attacks Cardiovascular problems (dizziness, palpitations) Chronic fatigue and low energy Chronic widespread aches and pains Depression Gastrointestinal disturbances/irritable bowl syndrome Intolerance to cold temperatures Irritable bladder syndrome Memory and concentration problems “Fibro Fog” Neck and back pain Symptoms continued Pelvic pain in women (painful menstruation) Poor circulation (cold hands and feet) Sleep disturbances and/or restless leg syndrome Stiffness (especially in the morning)/muscle twitching Subjective soft tissue swelling or paresthesia in hands, arms, feet or legs Tension headaches and/or migrains What causes Fibromyalgia? Cause is unknown Abnormally high levels of Substance P in spinal fluid in some patients Substance P important in transmission and amplification of pain signals to and from brain “Volume control” is turned up too high in brain’s pain centers What causes Fibromyalgia (cont) Familial tendency to develop FMS suggests genetic role Can be triggered by physical, emotional or environmental stressors such as car accidents, repetitive injuries and certain diseases Patients with Rheumatoid arthritis and SLE (Lupus) are more likely to develop FMS How is Fibromyalgia diagnosed? A diagnosis is made by evaluation of symptoms and presence of tender points American College of Rheumatology Classification Criteria for Fibromyalgia (1990)…….widespread pain for at least 3 months and pain in 11 out of 18 tender point sites on digital palpation How is Fibromyalgia diagnosed (cont) X-rays, blood tests, specialized scans such as nuclear medicine and CT, muscle biopsies are all normal procedures. Objective “markers of inflammation” such as ESR (erythrocyte sedimentation rate) are normal procedures. Must be distinguished from other common diffuse pain conditions How is Fibromyalgia treated? Fibromyalgia is a chronic condition managed with medications, and physical and nutritional modalities Medication therapy is largely symptomatic, as there is no definitive treatment cure for fibromyalgia How is Fibromyalgia treated? (Medications) Current studies suggest that the best pharmacologic treatment for treating pain and improving sleep disturbance includes: Antidepressants - Tricyclic compounds such as cyclobenzaprine (FLEXERIL) and amitriptyline (ELAVIL) - Dual reuptake inhibitors such as venlafaxine (EFFEXOR), duloxetine (CYMBALTA) and tramadol (ULTRAM) effect norepinephrine & serotonin How is Fibromyalgia treated? (Medications) SSRIs/ antidepressants such as fluoxetine (PROZAC), paroxetine (PAXIL) and sertraline (ZOLOFT) for depression and pain - Recent studies have shown that the anti-epileptics (seizure meds) gabapentin (NEURONTIN) and pregabalin (LYRICA) have been effective Other Therapies for Fibromyalgia Acupressure/Acupuncture Balneotherapy (Therapeutic baths) Biofeedback (Power of the mind) Collagen Hydrolysat (Food supplement) Magnet therapy Meditation/visual imaging Therapeutic massage Prolotherapy (injection of dextrose & Sarapin into joints or trigger points) Effects of Fibromyalgia on Exercise Pain associated with basic activities of daily living, general fatigue, and altered perception of exertion make it hard for individuals with FM to stay physically active. Morning stiffness, exaggerated delayed-onset muscle soreness (DOMS) and difficulty with use of the arms in elevated positions associated with FM limit the type of activities that can be done. Exercise with Fibromyalgia The irony here is that even though exercise can make you feel worse short term, the lack of it can make your symptoms more severe long term, as well as inviting more health problems. The key is moderation and pacing. Numerous studies demonstrate that even small amounts of exercise, as little as 6 minutes per day, can lessen pain and fatigue. Effects of medications on Exercise Lyrica (antiepileptics) Has been known to cause clumsiness, but other than that has no significant effects on exercise. Neurontin (antiepileptics) Can cause dizziness and blurred vision so not recommended if doing activities requiring quick reaction time, but most exercise is ok. Antidepressants No significant effects on exercise. Effects (acute) of exercise on patient Exercise causes acute pain and exhaustion with patients diagnosed with fibromyalgia (more so than individuals without fibromyalgia) Effects (chronic) of exercise on patient Exercise has been shown to decrease symptoms including, pain, stiffness, fatigue, depression, and insomnia with fibromyalgia patients long term. Exercise Testing Functional Lifting-specific activities Flexibility Sit and reach Goniometry Endurance 6 and 12 min walk Strength Handgrip Isotonic Aerobic Cycle Fibromyalgia Video Summary Fibromyalgia is a chronic condition that affects 5 – 10 million Americans. Doctors diagnose fibromyalgia based on a patient's symptoms and physical exam. Patients experience pain and stiffness in the muscles, but there are no measurable findings on X-rays or lab tests. While fibromyalgia does not damage the joints or organs, the constant aches and fatigue can have a significant impact on daily life. References http://arthritis.about.com/od/fibromyalgia/a/fibro_facts.htm Clark, S.R. et al. “Exercise for patients with fibromyalgia: risks versus benefits.” Curr Rheumatol Rep. 3 no. 2 (April 2001): 135-140 Wolfe F. et al. “The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee.” Arthritis Rheumatology. (1990) www.Fibrocenter.com Dunne, F.J. and C.A. Dunne “Fibromyalgia syndrome and psychiatric disorder.” British Jounal of Hospital Medicine. (1995) Webmd.com/fibromyalgia Medline Dr. Joe M. Elrod “Reversing Fibromyalgia” Woodland Publishing. 2nd ed. 2002