ACA and Future Policy. - National Hispanic Medical Association
advertisement
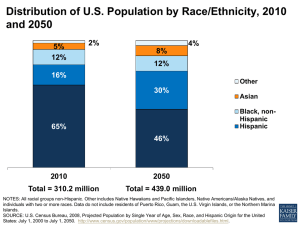
ACA and Future Policy Elena Rios, MD National Hispanic Medical Association October 2013 Demographics Demographics Key Trends Minorities face health care disparities in America By 2042, over half of Americans will be minority populations Latinos – immigrants, mixed families with strong cultural values -will be 1 out of 4 Americans Our nation is undergoing a major transformation: Cultural Competence & language requirements in hospitals/clinics and for future providers in medical education and public health Health care reform expands health care coverage to Hispanics and African Americans and increases the need for education and outreach efforts Quality value payments for coordinated patient centered care Disparities in obesity and chronic disease for minority populations remain high New demand for community-based health prevention and research NHMA/NHHF seeks to cultivate public and private partnerships to make a positive impact promoting prevention awareness & good will in new and growing Latino communities and markets around the nation Social Determinants of Health • SES – – – • • Education Income Residential segregation gradient of health outcomes and risk behaviors occupation, culture, social network and cohesion, correctional systems, legal policies, mental health and psychosocial factors, and forms of discrimination Residential Segregation • • The fundamental cause of racial/ethnic health disparities in the U.S. Environmental hazards, reduced access and quality of health care, increased violence and crime, and poorly built environments in which there is less access to supermarkets providing fresh fruits and vegetables, greater access to fast foods, and less recreational facilities than non-segregated neighborhoods, substandard housing. Societal Costs • • • • • Safety net providers (clinics, ED) more costly treatment than preventive and primary care Poor have more severe disease with complications and comorbidities Potentially preventable hospitalizations Premature deaths, loss in productivity Individuals, families, communities, employers, health plans, and governmental agencies, health insurance companies, businesses Societal Costs • • To date, estimated societal costs tend to underestimate the economic impact of health disparities by excluding costs to employers due to a larger pool of unhealthy workers and broader societal impacts such as decreased tax revenue because of lower productivity and increased insurance premiums as risk pools deteriorate. With increased minority population, global competition is at stake for the US. ACA, Disparities & Access Increased newly insured patients unfamiliar with healthcare, behavioral healthcare, oral healthcare and healthy living concepts Increased outreach and education especially to young adults and increase awareness about healthcare Increased communications – information on websites, social media, media, appointment systems, grievances, complaints with billing and subsidies/discounts Hispanic family-focused health information, coalitions, organizations, leaders Health Insurance Marketplace States/Federal Facilitated Grants to develop outreach with navigators that is culturally and linguistically appropriate; enrollment counselors; brokers Qualified healthplans - limited participation Essential community provider - safetynet Standards for benefits – presented in a culturally and linguistically appropriate manner, health literacy Subsidies 100-400%FPL ($23K -$96K) individuals/families, small businesses to get tax credits CBO Estimates by 2022, 25M Americans in the marketplaces Essential Benefits – transition policies needed Ambulatory care services Emergency Hospitalization Maternity/newborn Mental Health/Substance abuse disorders Prescription medications Rehabilitative and habilitative Laboratory Preventive services and chronic care management Pediatric, including oral, vision care Health Policy Trends Health insurance will be more prevalent in shopping centers, pharmacies, stores Home health, adult day care, PCMH – coordinated care, outpt care will increase Community prevention care programs Govt Hearings/document best practices Medical care use – population health, health planning needed Uninsured Populations Policy Need health insurance education in govt programs for mixed families– adult education programs, job training, CBOs, mental health, Medicaid, clinics, nutrition/farmers markets, schools Small business programs, faith-based, media campaigns Funding to public hospitals, clinics Public-Private Partnerships are the Future (social enterprise) Government procurement needs to link to public sector markets and solution economy or social innovation Example: Sec Clinton announced the USAID impact investment approach to development assistance, matching private sector funding Health insurance, pharmacies Corporations need healthy employees ACA, Disparities & Quality National Strategy for Quality Improvement in Health Care Priorities that have the greatest potential for improving health outcomes, efficiency, and patientcenteredness of health care, for all, including vulnerable populations Quality measures – Medicare/Medicaid hospitals, physicians experience, quality, use of info for pts and caregivers Equity of health services/disparities across health disparity populations Patient-centered, pt satisfaction, accessibility, availability ACA, Disparities & Quality Reimbursement – including activities to prevent hospital readmissions – comprehensive discharge program with pt centered education and counseling Best clinical practices that improve pt safety and reduce medical errors through evidence based medicine and Health Information Technology H-IT : EMR and PMR to include health disparities information from provider/patient/community assessments – for example, language needs ACA, Disparities & Quality Center for Medicare/Medicaid Innovation Pt centered medical home models Community health teams, small practice med homes – chronic care, self management Home health chronic care services Best practices Healthcare innovation zones Programs that address health care disparities and show impact ACA, Disparities & Prevention National Prevention, Health Promotion and Public Health Council (Fed agencies under HHS) Provide coordination and leadership at the Federal level with respect to prevention , health promotion, public health system and integrative health care in the US Develop a National Prevention and Health Promotion Strategy – health disparities priority Prevention and Health Promotion Investment Fund $10B Community Transformation Plan to promote healthy living and reduce disparities (including social determinants) Schools, restaurants, worksites Community prevention ACA, Disparities & Workforce National Health Care Workforce Plan – HHS, DEd, DOL Scope of work laws – need more providers of care Diversity needs to include Recruitment K-16 Interprofessional education, focus on primary care Nursing, oral, mental, allied, and public health workforce Geographic distribution of providers vs need Diversity to increase URM minority health professionals Cultural Competence training for all providers Community-based participatory research, PCORI (pt centered outcomes research), evidence based needed NHMA Vision to increase Latino Physicians – STEM Diversity Summit, Nov. 2013 Need for diversity and health professions in the President’s STEM Initiative (recruitment counseling still needed) OMB White House, Dept of Education, NSF, NIH, HRSA, Congress, IOM, Josiah Macy Foundation, RWJF Career pathway program – Hispanic STEM Program from HSIs to medical school Cultural Competence Standards Federal Law – Title VI Medical Education – AAMC, LCME, ACGME Joint Commission NCQA NQF standards Licensing – required in CA, NJ Language Services in Medicaid – in 13 Cultural Competence and Quality There is excellent evidence that tracking/reminder systems can improve quality of care, and fair evidence that multifaceted interventions, provider education interventions, and interventions that bypass the physician to offer screening services to racial/ethnic minority patients can improve quality of care. There is, however, excellent evidence for improvement in provider knowledge, good evidence for improvement in provider attitudes and skills, and good evidence for improvement in patient satisfaction. (AHRQ, Strategies for Improving Minority Healthcare Quality (Publication No. 04-E008-01, 2004) National Physician Survey 2011 Physicians overwhelmingly want the health care system to cover the costs associated with connecting patients to services that address their social needs. A majority of physicians surveyed say that the health of up to half their patients would improve if the health care system did a better job of addressing social needs. Source: RWJF Website – 1000 physician survey 2011. NHMA & NHHF– Who are We? Established in 1994 in DC, NHMA is a non-profit 501c6 association representing 45,000 Hispanic physicians in the U.S. Mission: to empower Hispanic physicians to improve the health of Hispanic populations with Hispanic medical societies, residents, students and public and private partners. Established in 2002, NHMA’s foundation, National Hispanic Health Foundation, a nonprofit 501c3 foundation for research & education activities – affiliated with NYU Wagner Graduate School of Public Service NHMA Board of Directors Kathy Flores, MD, Chairwoman, Director, UCSFresno Latino Research Center Louis Aguilar, MD, Treasurer, Tucson, AZ Sam Arce, MD, ViceChair, NYC Jorge Girotti, PhD, Secretary, Assoc. Dean, U of Illinois, Chicago School of Medicine Elena Rios, MD, President/CEO Washington, DC Raymond Arroyo, VP, Aetna David Carlisle, MD, President, Charles R. Drew University of Medicine and Science Emilio Carrillo, MD, MPH, Professor, Cornell Weill School of Medicine Judy Flores, MD, Dir, Adol Health, Woodhull Med Ctr/NYU Efrain Fuentes, EdD, Walt Disney Paloma Hernandez, MPH, CEO, Urban Health Inc. Norma Parra, MD, med dir, CentroMed, San Antonio Jorge Puente, MD, Regional President of Asia, Pfizer Nelson Reyneri, VP, Liberty Power John Sanchez, MD, Young Physicians Gerardo Lopez-Mena, MD, Chairman, Council of Residents Alvaro Galvis, Coordinator, Latino Medical Students Association NHHF Board of Directors Mark Diaz, MD Chairman, Principal, Alivio Medical Group, Sacramento, CA Conchita Paz, MD Secretary -Treasurer, Principal, Family Care Associates, Las Cruces, NM Elena Rios, MD, MSPH President, NHHF, NY Jo Ivey Boufford, MD President, New York Academy of Medicine Gary Pelletier Director, Pfizer Helpful Answers United Healthcare Walmart National Hispanic Medical Association – what do we do? Serve as a resource for White House, Congress, and Federal agencies on health policies and programs Support Hispanic physician leadership at national and state level Provide networking opportunities for advancement of Hispanic health National Hispanic Medical Association Programs Resource: Federal government Private sector Provide technical assistance to corporate health programs Nominate members to corporate boards Leadership Development: Capitol Hill Briefings on Hispanic health Issues to eliminate health disparities Nominate members to Federal advisory commissions NHMA Leadership Fellowship National Hispanic Health Professions Leadership Institute Health Professional Student Recruitment and Mentoring Programs Networking: NHMA 18th Annual Conference, Mar. 27-30, 2014, Washington, DC Regional Health Reform Events – NYC, Los Angeles, San Antonio, Chicago, Atlanta, DC NHMA Network 2013 Hispanic State Medical Societies National Hispanic Health Professional Leadership Network National Association of Hispanic Nurses Hispanic Dental Association Latino Caucus of APHA Latino Forum of Health Executives PAs, Mental Health Workers, Dietitians 12,000 Members and 40,000 Prospects Latino Medical Student Association Partners, Contacts NHMA & NHHF Contact Us NHMA - www.nhmamd.org NHHF - www.nhmafoundation.org Portal - www.hispanichealth.info National Hispanic Health Professional Student Scholarship Programs – Nov 21, LA; Dec 5, NYC – NHMA Annual Conference “ACA and Best Practices that Improve the Health of Hispanics” – Mar. 2014, DC