Health Politics and Policy in the United States
advertisement

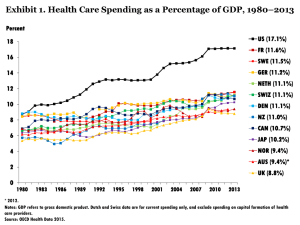
Health Politics and Policy in the United States PH 150 November 25, 2013 Prof. Tom Rice Dept. of Health Policy and Management Topics Covered (1) (2) (3) U.S. health system performance in an international context Politics of cost containment Recent reform legislation: The Patient Protection and Affordable Care Act U.S. Health System Performance SPENDING 4 International Comparison of Spending on Health, 1980–2010 Average spending on health per capita ($US PPP) Notes: PPP = purchasing power parity; GDP = gross domestic product. Source: Commonwealth Fund, based on OECD Health Data 2012. Total health expenditures as percent of GDP Total Health Expenditure per Capita and GDP per Capita, US and Selected Countries, 2008 $8,000 Per Capita Health Spending USA $7,000 $6,000 $5,000 Belgium $4,000 France $3,000 Italy $2,000 Austria Germany Spain Switzerland Canada Norway Netherlands U.K. Japan Australia Sweden $1,000 $0 $25,000 $30,000 $35,000 $40,000 $45,000 $50,000 $55,000 $60,000 $65,000 GDP Per Capita Source: Organisation for Economic Co-operation and Development (2010), "OECD Health Data", OECD Health Statistics (database). doi: 10.1787/data-00350en (Accessed on 14 February 2011). Notes: Data from Australia and Japan are 2007 data. Figures for Belgium, Canada, Netherlands, Norway and Switzerland, are OECD estimates. Average Annual Worker and Employer Contributions to Premiums and Total Premiums for Family Coverage Source: Kaiser/HRET Survey of Employer-Sponsored Health Benefits, 2002-2012. ACCESS 8 Percentage of Population Covered Under Public Programs (Source: OECD Health Data, 2008) 100% 100% 100% 99.9% 100% 98.7% 100% 100% 100% 89.5% 90% 80% 70% Percent 60% 50% 40% 27.4% 30% 20% 10% 0% AUS CAN FRA GER JAPAN NETH SWE SWITZ UK US Country 9 Percentage of Population Uninsured, 2007 (Source: OECD Health Data, 2008) 18% 16% 16% 14% Percent 12% 10% 8% 6% 4% 2% 2% 1% 0% 0% AUS CAN 0% 0% GER NETH UK US Country 10 Projected Trend in the Number of Uninsured in Absence of Health Reform in Absence of Health Care Reform, 2009–2020 Millions 80 60 48.0 48.9 50.3 51.8 53.3 54.7 56.0 57.2 58.3 59.2 60.2 61.1 40 20 0 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Path to a High Performance U.S. Health System: A 2020 Vision and the Policies to Pave the Way, February 2009. 11 Cost-Related Access Problems in the Past Year Percent AUS CAN FR GER NETH NZ NOR SWE SWIZ UK US Did not fill prescription or skipped doses 16 15 11 14 8 12 7 7 9 4 30 Had a medical problem but did not visit doctor 17 7 10 12 7 18 8 6 11 7 29 Skipped test, treatment, or follow-up 19 7 9 13 8 15 7 4 11 4 31 Yes to at least one of the above 30 20 19 22 15 26 14 11 18 11 42 Source: 2011 Commonwealth Fund International Health Policy Survey of Sicker Adults in Eleven Countries. 12 Access to Doctor When Sick or Needed Care Base: Adults with any chronic condition Percent 80 80 Same-day appointment 6+ days wait or never able to get appointment 60 60 60 54 48 42 40 43 36 40 26 34 26 20 26 20 18 23 18 14 8 3 0 S N AU CA 0 H FR GER NET NZ UK US S N AU CA H FR GER NET Data collection: Harris Interactive, Inc. Source: 2008 Commonwealth Fund International Health Policy Survey of Sicker Adults. NZ UK US 13 14 Wait Times for Elective Surgery and Specialist Appointments Percent AUS CAN FR GER NETH NZ NOR SWE SWIZ UK US Specialist appointment* Less than 4 weeks 54 41 53 83 70 61 50 45 82 72 80 2 months or more 28 41 28 7 16 22 34 31 5 19 9 Elective surgery** Less than 1 month 53 35 46 78 59 54 44 34 55 59 68 4 months or more 18 25 7 0 5 8 22 7 21 21 7 * Base: Needed to see specialist in past 2 years. ** Base: Needed elective surgery in past 2 years. Source: 2010 Commonwealth Fund International Health Policy Survey in Eleven Countries. 14 QUALITY 15 HEALTHY LIVES Infant Mortality Rate Infant deaths per 1,000 live births National average and state distribution U.S. average 12 Top 10% states 11.1 10.3 8 Bottom 10% states 7.2 7.0 International comparison, 2007 10.8 10.2 9.9 9.9 6.9 7.0 6.8 9.6 10.1 6.8 6.8 10.0 9.9 6.9 6.7 6.8 6.8 5.1 4 5.3 5.1 5.0 4.9 4.8 4.7 4.7 5.0 5.0 4.0 5.0 2.0 0 98 19 99 19 00 20 01 20 02 20 ^ 03 20 04 20 ^ 05 20 06 20 07 20 2.6 2.5 n d de la n e e w Ic S 2.7 3.1 s ay da nd ate ark an t a a w p l m r S n n Ja Ca ited No Fin De Un ^ Denotes years in 2006 and 2008 National Scorecards. Data: National and state—National Vital Statistics System, Linked Birth and Infant Death Data (AHRQ 2003–2008; Mathews and MacDorman, 2011); international comparison—OECD Health Data 2011 (database), Version 06/2011. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2011. 17 Medical, Medication, or Lab Test Errors in Past Two Years Percent reported: AUS CAN FR GER NETH NZ NOR SWE SWIZ UK US Wrong medication or dose 4 5 6 8 6 7 8 5 2 2 8 Medical mistake in treatment 10 11 6 8 11 13 17 11 4 4 11 Incorrect diagnostic/ lab test results* 4 5 3 2 6 5 4 3 3 2 5 Delays in abnormal test results* 7 11 3 5 5 8 10 9 5 4 10 Any medical, medication, or lab errors 19 21 13 16 20 22 25 20 9 8 22 * Base: Had blood test, x-rays, or other tests in past two years. Source: 2011 Commonwealth Fund International Health Policy Survey of Sicker Adults in Eleven Countries. U.S. Lags Other Countries: Mortality Amenable to Health Care Deaths per 100,000 population* 1997–98 150 2006–07 134 127 116 115 109 99 100 89 88 120 113 106 97 97 88 81 76 50 96 57 55 61 60 61 64 66 74 67 76 79 78 77 80 83 d De nm Un ar ite k d Ki ng do Un m ite d St at es al an d Ze la n Ne w Ir e ec e Gr e m an y d Ge r Fi nl an No rw ay Ne th er la nd s Au st ria en Sw ed pa n Ja ly It a ra lia Au st Fr an ce 0 * Countries’ age-standardized death rates before age 75; including ischemic heart disease, diabetes, stroke, and bacterial infections. Analysis of World Health Organization mortality files and CDC mortality data for U.S. Source: Adapted from E. Nolte and M. McKee, “Variations in Amenable Mortality—Trends in 16 High-Income Nations,” Health Policy, published online Sept. 12, 2011. Readmitted to Hospital or Went to ER from Complications During Recovery Base: Adults with any chronic condition who were hospitalized Percent 40 20 17 18 17 11 7 9 11 10 NZ UK 0 AUS CAN FR GER NETH Data collection: Harris Interactive, Inc. Source: 2008 Commonwealth Fund International Health Policy Survey of Sicker Adults. US 19 20 Features of U.S. Health Care System • Insurance coverage is not universal and relies on a system of voluntary private insurance – Employers do not have to offer coverage – Individuals do not have to purchase coverage – This will change partly on January 1, 2014 • There is no overall budget • Rationing is largely carried out on the demand rather than supply side – Price rather than personnel or technology is limiting factor Politics of Cost Containment A Fundamental Identity in Health Economics* Total Revenue = Total Expenditures = Total Income T+R+C=PxQ=WxZ where, T = taxes R = private insurance premiums C = direct charges to patients P = average price of health care services Q = quantity of health care services provided W = average wage Z = total inputs used (labor and capital) *from Robert Evans Some Political Implications Regarding Cost Containment from this Economic Identity T+R+C=PxQ=WxZ • If we cut taxes, we either have to cut prices or services provided to deal with reduced revenue. • If revenue is reduced, either wage or inputs (e.g., employment) will have to be cut. • There are therefore strong forces that will oppose particular cost containment proposals because every dollar of costs that are contained means that someone’s income or job will be at stake. Patient Protection and Affordable Care Act of 2010 (ACA)* * Most provisions go into effect on January 1, 2014 Insurance Coverage • From about 55 million to about 31 million uninsured: – – – – Income-based subsidies to uninsured Employer mandate Individual mandate Medicaid (low-income coverage) expansion but at states’ option • Mechanisms: – Private: Each state create insurance exchange for individuals w/o coverage and small employers – Public: the Medicaid expansion 26 Coverage (continued) • Subsidies: sliding scale up to 400% poverty level • Medicaid: everyone covered whose income is less than 138% of poverty level – if state agrees • Individual mandate: Everyone must buy coverage or pay a penalty (by 2016, $700/individual, $2100/family), unless this exceeds 8% of income. • Employer mandate: Employers with more than 50 employees must provide coverage or pay penalty of $2000/employee. (This has been delayed to 2015.) 27 Health Insurers… • Cannot turn applicants down who have history of illness • Cannot terminate coverage • Must renew coverage • Cannot charge more to those who history of illness (older people can be charged maximum of 3 times that of younger person) • Return at least 80% of premiums in the form of health service benefits 28 Quality Enhancement • Establish office to support “comparative effectiveness research” • Pilot program to develop “bundled payment” systems for hospital, physician, and post-acute services to “accountable care organizations” • Pay hospitals based on performance on quality measures, with nursing homes and home health care to follow 29 Financing • Increase Medicare Part A payroll tax from 1.45 to 2.35%, and 3.8% extra tax on investment income, for those with incomes over $200,000 individual or $250,000 family • “Cadillac tax” on employer health plans with values above $10,000 individual/$27,500 families, beginning 2018. Tax = 40% of amount above thresholds • Reduce payments to Medicare managed care plans • Effect other reductions in Medicare spending; establish Board to submit proposals to contain costs if Medicare spending rises too quickly • 10% tax on indoor tanning services 30 Examples of How Politics Affected ACA • Insurance exchanges only include private companies; no government option • Comparative effectiveness research cannot consider costs, and cannot influence what services will be covered or their reimbursement • No coverage for undocumented individuals • More generally, very little in the way of cost containment is included Issues “du jour” • “Disastrous” roll-out of the websites for purchasing insurance • President Obama’s original assurance that “If you like your plan, you can keep it.”