CMU - NatPaCT
advertisement

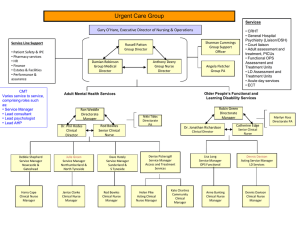
Cardiac Monitoring Unit (CMU) Hull Royal Infirmary ♥THE JOURNEY SO FAR.. Diane Rothwell, Project Manager North & East Yorkshire & Northern Lincolnshire CHD Collaborative diane.rothwell@herhis.nhs.uk REGION & BASE CMU MICROSYSTEM Doctors Nurses Domestics and caterers Ward Clerk Diabetic nurse PATIENTS Physio and Physio Assistants Pharmacist Social Worker Cardiac Rehab. Nurse Smoking cessation officer Dietician Paramedics Scarborough Bridlington Grimsby Ward 80 AAU Ward 8 Ward 8 HDU ICU Ward 6 (CHH) Ward 80 Ward 7 (CHH) Combined pr ICU (CHH) Chest P Clinic CMU MICROSYSTEM Combined Pr ECG Dept (o/p Home Scunthorpe Par/Ambulance Louth ICU (HRI) York Combined Procedures Private Sector HDU Other Hospital ICU HDU Aca. Cardiology GP/Home Information Flow Patient Flow ENGAGAING PERSONNEL WITHIN THE MICROSYSTEM 2 WAY COMMUNICATION BOARD CHALLENGE OF THE MONTH The CMU Team work together to Provide Quality Care That Reaches the Heart of the Problem “Your Heart in Our Hands” ‘P’ATIENTS Aim: To find out what our patients think about the care and services we provide. To carry out Discovery Interviews with Patients’ and their carers. PDSA in Progress ♥ OTHER PDSA’S PLANNED ♥ Patient Information ♥ Suggestion Box ♥ Patient Questionnaire Interviews being scheduled DISCOVERY INTERVIEW PDSA ‘P’ERSONNEL ♥ Staff Survey ♥ Assessment Tool ♥ Online Workforce Survey ‘P’ERSONNEL I I would recommend CMU as a great place to work would recommend CMU as a great place to work 12 11 12 11 10 9 8 7 6 5 4 3 2 1 0 10 9 8 7 6 5 4 3 2 1 0 Strongly Agree Agree Disagree Strongly Disagree Strongly Agree How easy is it to ask anyone a question about the w ay w e care for patients? 12 11 10 9 8 7 6 5 4 3 2 1 0 Very Easy Easy Difficult Very Difficult Agree Disagree Strongly Disagree ‘P’ROCESSES Paramedics Patient in ambulanceHRI Bottle neck - In rural areas 4045 minute journey to HRI 5 minutes VALUE ADDED Paramedic gives asprin if appropriate AAU NurseDiamorphine given House officer orders analgesia Paramedic gives VENFLON Some Junior doctors don't use AMI pathway and take full History 5 minutes ECG given to House officer (staff grade doctor) Bottle neck - In rural areas lack of ambulance can delay time Ambulance arrives -Hull Royal Infirmary A&E AAU Nurse takes ECG to doctor Result available on computer in AAU (Not CMU) AAU Nurse establishes if asprin administered 3 minutes Ambulance arrives Patient removed from ambulance into A&E ambulance entrance Onset of chest pain in patien t AAU Nurse Monitors patient AAU Nurse does ECG Triage nurse to triage point CMU Nurse set up monitor and baseline obs Consent for strep gained - explanation of issues for treatment, side effects etc. CMU SHO informed Triage nurse phones AAU (dedicated phone) Patient transferred to AAU trolley 3-5 minutes AAU agree to take Paramedics handover Digami Regime started on appropriate patient in AAU after 30 minute delay AAU Nurse Strep tends to be finished in AAU IF appropriate a Cardiology registrar may be called AAU Doctor Rings CMU 2 minutes G P gives Diamorphine & Cycizine Ambulance crew take patient to AAU 2 minutes AAU nurse greets patient Patient transferred to CMU with: AAU Nurse AAU Doctor AAU Porter CMU staff nurse accepts patient if bed available This is variable CMU Staff/ ECG Technician ECG Review at 90 minutes Bottleneck- Can take 5 minutes to 12 hours to find notes that have not been received by the ward History taken by SHO CMU If fails 90 minutes ECG consider REACT trial Ring porter in Theatre lift If no bed CMU staff decant patient to ward 8/80 Bed in CMU becomes available Call bed Coordinator (Bleep 203) if no Bed Physio and/ or CMU nurses start Physio 1b exercises Rethrombolysed if needed CMU Nursing staff introduce patient to initial rehab booklet If Lysis successful CMU staff nurse proceeds with bedrest and monitoring Record 2 hour ECG by CMU nurse/ECG technician Record each treatment & inform nursing/ medical staff if any problems DailyPhysio finds out patients with a definite MI and finds out their condition (Mon-Fri) Porter breaks and After 10pm general porter used Day time -10pm porter has key. After 10pm kept in Cupboard on AAU Nurse in charge reviews ward occupancy (ward 8) Find patients who have moved wards and follow to continue treatment Nurse transfers patient from CMU to Ward 8 Patient may stay in AAU Bottle neck O ften beds not available Start inpatient cardiac rehab programme from appropriate stage until completion (daily) Nurse/ Physio G ive all relevant information required to aid recovery Nurse continues health education Rehab stages reiterated by nurse Take home medication sorted by SHO and Pharmacy Day/Stage 2 Bottleneck - Bed blocking. If no beds in CMU decant other patients if required. (Involve Reg) Contact Bleep holder and ward Nurse/ dietitian/ Physio all carry out health education Nurse Identifies patient worries and concerns Nurse discusses discharge with patients Nurse reiterates stages to patient Nurses involve the family as appropriate Communication Day/stage 4 Nurse/ Facilitator gives heart manual for patient to read Nurse Checks CK's Nurse checks patient's cholesterol Can refer to dietitian Nurse fills in care pathway (not AAU one) Dietitian receives referral from from nursing staff (ward 8 or CMU) Dietitian sees patient on ward for assessment and advice Referral to social services Follow-up arrangements made by ward clerk Nurse/Physio continue with Physiotherapy Pharmacist check drug cards and gives patient education Nurse carries out social assessment SHO review Bottle neck Nurse explore patient's risk factors Referred to physiotherapy Nurse reiterates stages to patient SHO Review Nurse requests transport for discharge Tests requested for postdischarge Nurse discusses medication with patient Physiotherapy Nurse completes discharge letter Patient given chest pain leaflet by nurse Nurse completes discharge ECG Bottleneck Nurse checks discharge arrangements Nurses gets date for R.N.U Nurse allocates bed Bottle neck- Time consuming Meet patient and explain the role of Physiotherapist Ward clerk Daily filing of casenotes Nurse completes ECG Nurse in charge/ named nurse Informs ward clerk & SHO 's of transfer details SHO Review More physiotherapy Day/stage 5 O ften problem in getting hold of notes Nurse in charge negotiates appropriate inter-ward transfers to create bed space Nurse or ECG technician carries out ECG Inform rehab co-ordinator of confirmed MI's relaying all patient admission information from board and nurse C/P files Nurse explains rehabilitation Referred to Cardiac rehab programme administrator Daily Physio checks medical notes and writes Patient O rientated Medical Record (Mon-Fri) Ward 8 nurse in charge discusses patient transfer details with CMU Nurse in charge allocates ward bed for CMU-ward transfer Physio Stage 1a exercises by Physio or CMU nurse Facilitate Heart Manual (Daily) G et AAU Porter who has key to lift AAU Nurse Rings CMU 2 minutes G P Inserts cannulae There is often a problem getting old note for comparison of ECG pre Lysis Arive on CMU and transferred to bed 10 minutes AAU Nurse give strep Bottle neck Problem in phoning for results Digami started if not completed in AAU CMU nurses complete 30 minute postLysis ECG O ften case notes are not where the tracing states they were. Left in rooms which are not easily accessible CMU nursing staff inform patient and relatives what is going to happen whist in hospital O ngoing throughout the stay If entered in to Trial CMU nurses and doctors follow REACT guidelines Name nurse introduces themselves AAU Makes up Strep in treatment room VALUE ADDED Education started by Dietitian if going onS/C insulin Relative cared for by CMU nurse CMU Nurse establish when Post Lysis ECG 's need doing and order (9-5) out of hours nursing staff do Ward clerk books patient and requests notes Imediately on arrival Strep in same drugs cupboard as controlled drugs 70 minutes G P takes History VALUE ADDED Problem for oxygen saturation 3 minutes 1 minute GP examines patient History taken by CMU Nurse Bottle neck NO written consent AAU Nurse complete O bservations Paramedic rings bell G P calls 999 and goes to patient Access blood results by phoning AAU 2 minutes 3 minutes Patient Calls GP Doctor takes history FBC, U&E, Bloodsugar, LKT, CK. Lipids 3 minutes Patient calls 999 Check glucose and if >11mmPx then IV dextrose and insulin Asprin given if not already House officer assesses Paramedic gives O xygen G P gives asprin if appropriate CMU nursing & medical staff complete admission documentation (written & clerking in) AAU nurse gets controlled drugs AAU walks to controlled drugs cupboard Nurse reads medical notes CMU and Ward 8 named nurse accept patient onto ward and handover information SHO review Nurse checks medication Bottleneck - ??? Why When how? Discontinue monitoring if appropriate Day/stage 3 Nurse sets up cardiac monitoring (if telemetry liaise with CMU) CMU Microsystem process for AMI Consultant/ registrar review Nurse Reiterates stages Technician performs ECG Nurse facilitates heart manual Physiotherapy Patient discharged ‘P’ROCESSES Smoking cessation officer ‘P’ATTERNS Patients Admited, Transfered In and Out, and Discharged to/from CMU by Hour 3 Month Period 60 50 Deaths Discharges Transfers Out Transfers In Admits 40 30 20 23 22 21 20 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 0 10 ‘P’ATTERNS TRANSFERS FROM OTHER HOSPTIALS 400 350 300 250 200 150 100 50 0 20 18 16 14 12 10 33% AMI 6 4 2 INCREASE – WHY? Statistical Process Control Jan-2004 Dec-2003 Nov-2003 Oct-2003 Sep-2003 Aug-2003 0 Jul-2003 c 8 Jun-2003 in Pa in at ro th d an st he May-2003 n Ab m or i al s tie ... ar he f o Apr-2003 N C ot ed od Mar-2003 H rt ea re i lu fa Feb-2003 . .. ia is i .. .. a. fl . rd or a. rd he ct nf ca ca nd c e i y la i o a p y i n ch em rd na io ta tm ha gi at ca al en i ll sc r i m u An yo q ic m fi b ys se e al on ox ut ub tri hr ar c S A P C A Jan-2003 Number of Patients TOP TEN The 5 P’s! Processes Patterns Patients Personnel Purpose ASPIRATIONS Patient Experience Improve the ‘interface’ with other Microsystems Integration ‘service improvement is not a separate activity’ Ensure that CMU is a place that people feel happy about coming to work. Microsystems has given me a much needed boost of enthusiasm I feel privileged to have had the experiences I’ve had We are creating a culture that supports service improvement I was full of ideas of how we could use the concept in CMU I must admit my initial thoughts were somewhat sceptical Reflections of Clinical Microsystems I feel better equipped to suggest ways in which we could change Microsystems has helped us explore ways of improving communication Staff feel empowered to make small changes from within our microsystem I contracted ‘microsytemiti s Being involved with ‘Microsystems ’ has made a difference to staff morale