Health Care Disparities: A Focus on Hypertension
advertisement

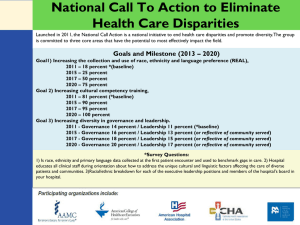
Health Care Disparities: A Focus on Hypertension Brian K. Irons, PharmD, BCPS, BC-ADM Division Head – Primary Care Associate Professor School of Pharmacy Objectives Review Types and Causes of Healthcare Disparities Assess Disparities in HTN Awareness / Control / Treatment Examine Ways to Minimize Disparities General Measures Role of Academia Focus on HTN Disparities in Healthcare Race / Ethnicity Health Disparities / Inequities Gender Race / Ethnicity Health Disparities / Inequities Gender Race / Ethnicity Health Disparities / Inequities Sexual Orientation Gender Race / Ethnicity Sexual Orientation Health Disparities / Inequities Socioeconomic Group Gender Race / Ethnicity Sexual Orientation Health Disparities / Inequities Age Socioeconomic Group Gender Race / Ethnicity Rural vs Urban Sexual Orientation Health Disparities / Inequities Age Socioeconomic Group Major Types of Disparities Access to Care (Disparities in Health Care) Quality of Care (Disparities in Health) Causes of Disparities in Access to Care Insurance coverage Regular source of care Delay in seeking care Decrease in needed care Financial resources Legal barriers Structural barriers Quality /Access to Care: Insured vs Uninsured Reduced Access to care Poorer medical outcomes Increased morbidities Earlier mortality Biggest impact on timeliness and quality of health care American College of Physicians 2004 Institute of Medicine 2001 2002 Population Base and Uninsured % of Population White % Uninsured Latino Afr-Amer Asian - PI Amer Indian Annals Intern Med 2004;141:226 Causes of Disparities in Access to Care Insurance coverage Financial resources Legal barriers Structural barriers Transportation Scheduling Employment issues Causes of Disparities in Access to Care Fragmentation of health care “system” Provider scarcity Language barriers Health literacy Healthcare beliefs Age Social Determinants in Disparities based on Race/Ethnicity Socioeconomic Status Social Determinants in Disparities based on Race/Ethnicity Socioeconomic Status Inadequate Housing Social Determinants in Disparities based on Race/Ethnicity Socioeconomic Status Inadequate Housing Proximity to Environmental Hazards Social Determinants in Disparities based on Race/Ethnicity Socioeconomic Status Education Level Inadequate Housing Proximity to Environmental Hazards Causes of Disparities in Quality of Care Provider – Patient Communication Provider Discrimination / Biases Poor Preventative Care Decreased patient satisfaction Decreased adherence Worse outcomes Awareness / Treatment / Control of Hypertension Differences between Races/Ethnicities and Age Risks of Uncontrolled HTN Stroke Arrhythmias Cognition Myocardial Infarction Increased BP Retinopathy Nephropathy Heart Failure NCHS Data Brief January 2008 NCHS Data Brief January 2008 NCHS Data Brief January 2008 Trends in HTN- Gender 35 Percent of Population 30 25 20 Men Women 15 10 5 0 1988-1994 Elevated BP or Taking BP Med 1999-2002 2003-2006 DHHS – CDC – NCHS 2009 Trends in HTN Race/Ethnicity - Men 45 Percent of Population 40 35 30 25 White Afr-Amer Mex-Amer 20 15 10 5 0 1988-1994 Elevated BP or Taking BP Med 1999-2002 2003-2006 DHHS – CDC – NCHS 2009 Trends in HTN Race/Ethnicity - Women 45 Percent of Population 40 35 30 25 White Afr-Amer Mex-Amer 20 15 10 5 0 1988-1994 Elevated BP or Taking BP Med 1999-2002 2003-2006 DHHS – CDC – NCHS 2009 Trends in HTN Income 35 Percent of Population 30 25 Poverty Level < 100% 100-199% 200+ % 20 15 10 5 0 1988-1994 Elevated BP or Taking BP Med 1999-2002 2003-2006 DHHS – CDC – NCHS 2009 BP Differences: Medicare Eligibility Annals of Intern Med 2009;150:505 Prevalence of HTN – Dyslipidemia – DM 2005-2006 NHANES 60 50 Percent 40 4.6 2.8 2.5 13.4 12.8 16.4 28.9 29.8 28.6 26.1 Total White Afr-Amer Mex-Amer 3.8 12.7 30 3 Conditions 2 Conditions 1 Conditon 20 10 0 CDC NHCS Data Brief #36 April 2010 Hypertension And Age Percent of Population HTN and Age 90 80 70 60 50 40 30 20 10 0 64.7 69.6 76.4 64.1 53.7 55.8 36.2 35.9 23.2 13.4 16.5 6.2 20-34 35-44 45-54 Men 55-64 65-74 75+ Women Lloyd-Jones D, et al. Circulation. 2009.119; e21-e181. Changes in SBP/DBP with Age NEJM 2007;357:789 BP-Age and Mortality from Heart Disease 80-89 yrs 70-79 yrs 60-69 yrs 50-59 yrs 40-49 yrs Chobanian AV, et al. JNC 7. Hypertension. 2003; 42:1206 1252. Fatal CAD Risk and Age For the same Systolic BP Patient 80-89 years of age versus 40-49 years 16x risk for fatal CAD Circulation 2007;115 Minimizing Disparities Minimize Disparities: Race/Ethnicity Increase government offices of minority health Expanded access Raise awareness (Providers and Patients) Health Disparities Roundtable Federal Collaboration on Health Disparities Research Disparity Reducing Advances Project CMS’s Health Disparities Program Healthy People 2010 and 2020 Minimizing Disparities in HTN Management : Age Don’t assume benefits will be limited just because a patient is older Don’t treat all older patients the same Functional / Cognitive Status Living Arrangements Co-morbidities Who is ‘Older’? Patient 1 81 yo WM No chronic medications No diagnosed chronic conditions Patient 2 66 yo HF Diagnosed with DM 12 years ago h/o CAD / CHF / CVA / HTN / Lipids / COPD On 17 meds Cognitively impaired Benefits to Treating Isolated Systolic HTN Relative Risk Reduction (%) 15,693 patients, mean age 70, initial BP 174/83, 3.8 yr follow-up 0 -5 -10 -15 -20 -25 -30 Stroke ALL CV Events MI Mortality Lancet 2000;355:865 Recommended HTN Treatments for Isolated Systolic HTN SHEP / Syst-Eur Trials Thiazide Diuretic Dihydropyridine CCB Approach and Goals similar to Essential HTN < 140/90 mm Hg Treating HTN in the Very Old Most trials excluded or simply didn’t recruit many very elderly patients (> 80) Meta-analysis in 1999 for those >80 15 10 Relative Change (%) 5 0 -5 -10 -15 -20 -25 -30 -35 -40 Stroke Death Lancet 1999;353:793 Treating HTN in the Very Old Retrospective Study in VA Patients > 80 years old 85% taking antihypertensives Shorter duration survival for those with SBP <140 mm Hg “Clinicians should use caution in their approach to BP lowering in this age group” JAGS 2007;55:383 Hypertension in the Very Elderly Trial (HYVET) 3845 patients 80+ years of age (mean 83.6 years) Baseline BP: 173/91 Indapamide vs placebo (perindopril added prn) Target BP: < 150/80 1.8 years of follow-up Primary outcome: Stroke (fatal and non) Secondary outcomes: all cause mortality / CV mortality / CAD mortality / stroke mortality NEJM 2008;358:1887 Hypertension in the Very Elderly Trial (HYVET) % Re Reduction (%) 0 -10 -20 NS -30 -40 -50 -60 -70 Stroke All Mortality Exp 143/78 vs placebo 158/84 Stroke Death HF Any CV Event NEJM 2008;358:1887 What is BP Goal in the Very Elderly? No specific guideline… yet < 150/80 ? Reduces mortality, fatal stroke, HF Does it cause cognitive problems, increase fall risk? What about very elderly patients with existing CAD Can we risk < 130/80? Risks of BP Meds in the Elderly Prone to ADRs Lots of comorbidities / contraindications to look out for Cognitive impairment Compliance Costs Risks of BP Meds in the Elderly Orthostatic hypotension Sensitive to volume depletion / sympathetic inhibition Increased risk for falls Definition: Sitting to standing drop in BP (usually increase in heart rate) >20 mm difference in SBP / >10 mm dif in DBP Strategies for HTN Medication use in Elderly Start low and go slow COMMUNICATE Once daily regimens if compliance issues Avoid central acting agonists and alphablockers Caution with beta-blockers without a compelling co-morbidity Minimizing Disparities in HTN Management : Race / Ethnicity Optimize use of medications that may have pharmacodynamic benefits in certain populations African-Americans with HTN and Medication Adherence Beliefs Negative Factors Positive Factors Financial Resources Neighborhood Violence Distrust of Healthcare Professionals Family Friends Neighbors God J Cardiovasc Nursing 2010; 25:199 Age and Ethnicity Affect the Response of DBP to -Blockers but Not to Calcium Channel Blockers VA Cooperative Study of Responses to Single-Drug Therapy Atenolol Change in DBP (mm Hg) from Baseline 0 Diltiazem Placebo -5 -10 * -15 -20 -25 * * *† * * * ‡ White men, <60 yr Black men, <60 yr *P ≤ 0.05 vs. placebo †P ≤ 0.05 vs. white men of all ages ‡P ≤ 0.05 vs. placebo and atenolol DBP = diastolic blood pressure Materson BJ, et al. N Engl J Med. 1993;328:914-921. White men, ≥60 yr Black men, ≥60 yr Reductions in Diastolic Blood Pressure in Response to Specific Drugs Were Influenced by Age and Ethnicity VA Cooperative Study of Responses to Single-Drug Therapy Change in DBP (mm Hg) from Baseline 0 HCTZ Captopril Clonidine Prazosin Placebo -5 -10 -15 * *† * * * * ‡ * † * * * White men, <60 yr -20 -25 *P ≤ 0.05 vs. placebo only †P ≤ 0.05 vs. captopril or placebo ‡P ≤ 0.05 vs. HCTZ or placebo DBP = diastolic blood pressure; HCTZ = hydrochlorothiazide Materson BJ, et al. N Engl J Med. 1993;328:914-921. Black men, <60 yr White men, ≥60 yr Black men, ≥60 yr Reductions in SBP* in Response to Atenolol, Captopril, and Prazosin Were Influenced by Age and Ethnicity VA Cooperative Study of Responses to Single-Drug Therapy Change in SBP (mm Hg) from Baseline 0 Captopril Prazosin Placebo -5 -10 -15 † * * * ‡ *§ * -25 -30 *§ * -20 -35 *SBP Atenolol *P ≤ 0.05 vs. placebo only †P ≤ 0.05 vs. older white men ‡P ≤ 0.05 vs. older white men and younger black men §P ≤ 0.05 vs. older white men = systolic blood pressure Materson BJ, et al. N Engl J Med. 1993;328:914-921. White men, <60 yr Black men, <60 yr White men, ≥60 yr Black men, ≥60 yr Reductions in Systolic Blood Pressure in Response to Specific Drugs Were Influenced by Age and Ethnicity VA Cooperative Study of Responses to Single-Drug Therapy HCTZ Change in SBP (mm Hg) from Baseline 0 Clonidine Diltiazem Placebo -5 -10 -15 -20 * * * * * * * * * * * * -25 White men, <60 yr -30 White men, ≥60 yr -35 Black men, <60 yr *P ≤ 0.05 vs. placebo only Black men, ≥60 yr HCTZ = hydrochlorothiazide; SBP = systolic blood pressure Materson BJ, et al. N Engl J Med. 1993;328:914-921. 100 75 50 25 0 White Men <60 yr * * Successful Treatment (%) Successful Treatment (%) Rates of Successful Treatment Were Similar for Most Single Drugs in White Men VA Cooperative Study of Responses to Single-Drug Therapy 100 White Men ≥60 yr 75 * 50 25 0 *There were no clinically important differences (<15%) between the treatment groups spanned by the arrows. Treatment was considered to be successful if the diastolic blood pressure measured <95 mm Hg after 1 year. HCTZ = hydrochlorothiazide Reprinted from Materson BJ, et al. Am J Hypertens. 1995;8:189-192, with permission from Elsevier; Materson BJ, et al. N Engl J Med. 1993;328:914-921. 100 75 50 25 0 Black Men <60 yr † Successful Treatment (%) Successful Treatment (%) CCBs* and Diuretics Produced More Treatment Successes in Black Men VA Cooperative Study of Responses to Single-Drug Therapy 100 75 50 Black Men ≥60 yr † † † † 25 0 *CCB = calcium channel blockers; HCTZ = hydrochlorothiazide †There were no clinically important differences (<15%) between the treatment groups spanned by the arrows. Treatment was considered to be successful if the diastolic blood pressure measured <95 mm Hg after 1 year. Reprinted from Materson BJ, et al. Am J Hypertens. 1995;8:189-192, with permission from Elsevier; Materson BJ, et al. N Engl J Med. 1993;328:914-921. ALLHAT Outcomes: Black vs ‘Nonblack’ No benefit of chlorthalidone over amlodipine in: Nonfatal MI / Death CHD All-cause mortality Stroke Combined CHD events Favored thiazide over CCB for heart failure Same results for age (< 65 or >65 years) JAMA 2002;288:2981 ALLHAT Outcomes: Black vs ‘Nonblack’ No benefit of chlorthalidone over lisinopril in: Nonfatal MI / Death CHD All-cause mortality Favored thiazide over ACE-I for: Stroke Combined CHD events Heart failure JAMA 2002;288:2981 ALLHAT Outcomes: Age (< 65 or > 65) No benefit of chlorthalidone over lisinopril in: Nonfatal MI / Death CHD All-cause mortality Stroke Favored thiazide over ACE-I for: Combined CVD events Combined CHD events Heart failure JAMA 2002;288:2981 Minimize Disparities: Role of Academia Societal Roles Deliver primary and specialty services Service to the poor or uninsured Research Education Academic Medicine 2006;81:788 Minimize Disparities: Race / Ethnicity Role of Academia Health Care System Collect/Report data by race/ethnicity Implement/Evaluate disparities-reduction programs Support language interpretation Support use of evidence-based therapeutics Academic Medicine 2006;81:788 Minimize Disparities: Race / Ethnicity Role of Academia Education Increased cultural competency (everybody in the work force not just providers) Increase minority representation in the healthcare workforce Increase cross-cultural education Impact of disparities on decision making Academic Medicine 2006;81:788 Minimize Disparities: Race / Ethnicity Role of Academia Research Identify sources of disparities Develop and evaluate interventions Academic Medicine 2006;81:788 TTUHSC SOM Examples Admissions: Increase minority enrollment Recruitment activities Scholarship monies Recognized in past as a top recruiter of Hispanic students Curriculum: Required Basic Medical Spanish Required didactic or experiential training in cultural competency TTUHSC SOM Examples Clinical Services: Grace Clinic (East): Cardiology Fellows clinic serves underserved patient populations Other Outreach: Student run free clinic (Lubbock Impact) BP screenings by SOM students TTUHSC SON Examples Larry Combest Community and Wellness Center Endowed Professor on Rural Health Disparities Grants Childhood obesity prevention / Focus on Hispanics RN-Family home visitation program for low income first time mothers TTUHSC SOP Examples Admissions Process: Increased enrollment of minorities Curriculum: Only SOP in the country with required advanced experiential training in both Peds and Geries Only 1 of 3 SOPs with required Rural rotation Medical Spanish Elective / Cult Competency Elective Reviewing cultural competency within the curriculum Service: Numerous faculty clinics in West Texas providing care to underserved populations QUESTIONS ??????