Extreme Physiology and HAPE by dr. Abundio Balgos
advertisement
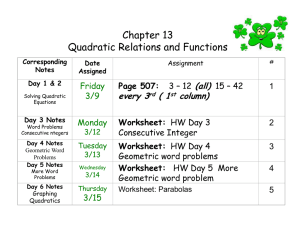
EXTREME PHYSIOLOGY HIGH ALTITUDE PULMONARY EDEMA Abundio Balgos, M.D., MHA, FPCP, FPCCP, FCCP Agatep Tolete Professor of Medicine Associate Dean for Planning and Research U.P. College of Medicine Disclosures • Currently a Professor at the College of Medicine, University of the Philippines, Manila • Active Pulmonary Consultant at Manila Doctors’ Hospital and Associate Active Consultant at Makati Medical Center • Has done studies, and given lectures in relation to these studies, for Astra Zeneca, Glaxo Smith Kline, Eli Lilly, Pfizer, United Laboratories, Pharmacia, Pfizer, Bayer, and Otsuka; these have no bearing on the lecture on High Altitude Diseases DO WE NEED TO KNOW HIGH ALTITUDE DISEASE? High altitude data: •140M people reside at altitudes >2500m •There are telescopes at >5000m and mines at >4500m •30 to 50,000 workers in the Tibet railroad project worked at >4000m •Skiers and mountain trekkers go to 3000m mostly, some to >8000m West, JB. Annals Intern Med, 2004, 141:789-900 Can anyone climb Mt. Everest? Up to 2004, Himalayan database showed that: • Mt. Everest summit was reached 2251 times • 130 of these ascents were without supplemental oxygen Who really was the first Filipino to reach the summit of Mt. Everest? •Leo Oracion •Erwin Emata •Romy Garduce •Dale Abenojar HOW HIGH IS HIGH-ALTITUDE ? • • •• High altitude: 1500-3000m above sea level Very high altitude: 3000-5000m For sea altitude: level visitors, Extreme above 5000m Andes 4600-4900m = (6962m) highest acceptable level for permanent habitation Tibetan plateau & Himalayan valleys (8848m) • For high altitude residents, 58006000m = highest so far recorded Ethiopian highlands (4620m) Mt. Apo Mindanao 2954m Mt. Pulog Luzon 2922 Mt. Halcon Mindoro 2582 Mayon Luzon Volcano Mt. Katanglad Mindanao 2462 Kanlaon Mountain Mt. Madiaas Negros 2430 Panay 2117 Mt. Mantaling Palawan 2938 2085 LECTURE OUTLINE • Review of basic physiological principles of respiration as they relate to changes in pressure and temperature • Animal and human adaptations to high altitude • What happens when acclimatization fails ? – Acute mountain sickness – High altitude pulmonary edema – High altitude cerebral edema External Respiration Atmospheric composition at sea level GAS NITROGEN OXYGEN ARGON CARBON DIOXIDE HYDROGEN NEON HELIUM PERCENT 78.08 20.95 0.94 0.03 0.01 0.0018 0.0005 Atmospheric Pressure declines with altitude Sea level: 1 atm = 14.7 lbs/inch2 (psi) 18,000 ft (5,486 m): 0.5 atm = 7.35 psi Atmosphere Reduction in Pressure And O2 - 8863 m Mount Everest Pressure reduced to 1/2 atm 0.1 atm reduction every 1km - 4860 m Human Settlement, Tibet 2954 m Mt. Apo Sea Level = 1 atm Hydrosphere Increase in Pressure And Gas Solubility 13 atm 370 atm -130 m -3700 m average depth of oceans 1 atm increase every ~10 m 1086 atm -10860 m Mariana Trench Baguio City QuickTime™ and a Photo - JPEG decompressor are needed to see this picture. Pressure differences are enormous, leading to differences in oxygen supply for air-breathers Mt. Apo Adaptations to high altitude High altitude mammals: More pigment in blood High affinity hemoglobin Birds: (1) Cross-current flow of air and blood allowing higher O2 concentration in blood than in exhaled air (2) Tolerate low CO2 in blood (Alkalosis) (3) Normal blood flow to the brain at low blood PCO2 (4) Total respiratory volume is 3X that of mammals Evolution of hemoglobin function •Highland Camelids (llama, vicuña, alpaca) display lower P50 (higher affinity) than lowland Asian/African camels • Amino acid substitutions in globin chains which reduce the effect of DPG binding • A small number of substitutions are sufficient to adapt the functional properties of hemoglobin to severely hypoxic conditions Adaptation vs Acclimation/Acclimatization 1) Short Term Acclimation Mountain climbers who are able to maintain normal pH at low oxygen 2) Developmental Acclimation A person reared at high altitude: larger lung volume Higher concentration of red blood cells 3) Adaptation Llamas: Blood with high Oxygen affinities blood High Altitude: Humans Developmental Acclimation (Mountain People) • Larger lung volumes • 40% higher ventilation rate in populations at 4500m (≠ maladapted hyperventilation) • Increase number of blood cells (5 million/mm3 --> 8 million/mm3 at 4000m) • Increase myoglobin concentration in muscles • Effect on Enzymatic pathways not understood • Increase in number of muscle capillaries and mitochondria • Whether Adaptive differences occur in Humans is not known High Altitude: Humans • Highest permanent settlement: 5000m mining camp in Andes RESPONSE TO LOW O2: • Hyperventilation leading to low PCO2 • Chronic Hypoxia High Altitude: Humans Acclimation (or Acclimatization) • Change in response of respiratory center (in hypothalamus) • Adjust bicarbonate concentration in blood to maintain normal blood pH at low PO2 (and low PCO2 that arises from hyperventilation) ACCLIMATIZATION • Process by which people gradually adjust to high altitude • Determines survival and performance at high altitude • Series of physiological changes O2 delivery hypoxic tolerance +++ • Acclimatization depends on • severity of the high-altitude hypoxic stress • rate of onset of the hypoxia • individual’s physiological response to hypoxia High Altitude: Humans • Hyperventilation (negative feedback) (1) In response to low O2, ventilation increases (2) But then this reduces PCO2 (3) pH increases, reducing normal stimulation in the respiratory center (4) Reduces ventilation (5) Decrease oxygen supply (6) More increased ventilation to gain O2 • Hypoxia: Brain damage after 4-6 minutes of oxygen deprivation Heart and Pulmonary Circulation at High Altitude Penaloza, D and vier Arias-Stella J. Circulation. 2007;115:1132-1146.) VENTILATORY ACCLIMATIZATION • Hypoxic ventilatory response = VE • Starts within the 1st few hours of exposure 1500m • Mechanism Ascent to altitude Hypoxia Decreased PCO2 Carotid body stimulation Respiratory centres stimulation Increased ventilation CO2 + H2O H2CO3 HCO3- + H+ Improved hypoxia ADJUSMENT OF RESPIRATORY ALKALOSIS • alkaline bicarbonate excretion in the urine but slow process ! • Progressive increase in the sensitivity of the carotid bodies • After several hr to days at altitude (interval of ventilatory acclimatization): cerebrospinal fluid pH adjustment to the respiratory alkalosis new steady state VENTILATORY RESPONSE TO EXERCISE • Varies with hypoxia ventilatory response (HVR) at rest at sea level – Larger ventilatory response climbing performance – but, at extreme altitude, larger work of breathing altitude trade-off Schoene et al., 1984 LUNG DIFFUSION • Definition Process by which O2 moves from the alveolar gas into the pulmonary capillary blood, and CO2 moves in the reverse direction • High altitude O2 diffusion, because of – a lower driving pressure for O2 from the air to the blood – a lower affinity of Hb for O2 on the steep portion of the O2/Hb curve and inadequate time for equilibration CONSEQUENCE O2 DIFFUSION arterial O2 saturation West et al., 1983 Wagner et al, Mt. Everest II project,1995 VA/Q HETEROGENEITY • Varies from zero to infinity • Zero : perfusion but no ventilation – O2 and CO2 tensions in arterial blood, equal those of mixed venous blood because there is no gas exchange in the capillaries • Infinity: ventilation but no perfusion – no modification of inspired air takes place due to overventilation or under-perfusion VA/Q HETEROGENEITY • At rest • At high altitude – interstitial edema heterogeneity +++ O2 - Inhaled air is not evenly distributed to alveoli Composition of gases is not uniform throughout lungs Different areas of the lungs have different perfusion Differences are less in recumbent position Penaloza, D and vier Arias-Stella J. Circulation. 2007;115:1132-1146.) MIGET evaluation of Ventilation-perfusion relationships during induced polycythemia (with no pulmonary hypertension) Hct Range Hct Midpoint Log SD Perfusion Mean Perfusion Log SD Ventilation Mean Ventilation 30-39 35 0.47+0.20 0.56 1.79+0.14 1.66 40-49 45 0.49+0.09 1.05 1.40+0.52 2.20 50-59 55 0.48+0.08 1,22 1.53+0.26 2.87 60-69 65 0.46+0.04 1.97 1.10+0.52 3.44 70-79 75 0.44+0.10 2.72 0.84+0.58 3.96 Balgos A, Willford D, West JB. J Appl Physiol, 65(4): 1686-1692, 1988 Maximal oxygen consumption at high altitude • 85% of sea level values, at 3000m; 60% at 5000m, and only 20% at 8000m • Ascribed to reduction in mitochondrial PO2 • Could also be due to central inhibition from brain • Most likely not due to pulmonary hypertension • Elite mountaineers tend to have an insertion variant of angiotensin-converting enzyme gene West, JB. Annals Intern Med, 2004, 141:789-900 Effects on Mental performance • Most people working at >4000m experience increased arithmetic error, reduced attention span, and increased mental fatigue • Visual sensitivity (night vision) decreased at 2000m, and up to 50% at 5000m • Molecular and cellular mechanisms of these effects of hypoxia are poorly understood • Suggested mechanisms: altered ion homeostasis, changes in calcium metabolism, alterations in neurotransmitter metab., and impaired synapse function West, JB. Annals Intern Med, 2004, 141:789-900 Effects on Sleep • Sleep impairment common and most distressing: frequent awakenings, unpleasant dreams, do not feel refreshed on waking up in the morning • Periodic breathing,which occurs at >4000m is most likely an important causative factor • Possible reasons for periodic breathing: instability of of control system for hypoxic drive, or response to CO2, as well as low levels of PaO2 after apneic episodes West, JB. Annals Intern Med, 2004, 141:789-900 WHEN ACCLIMATIZATION FAILS • Altitude syndromes – Acute mountain sickness (AMS): the least-threatening and most common – High altitude pulmonary edema potentially lethal form of AMS – High altitude cerebral edema • All these syndromes have – several features in common – respond to descent or oxygen ACUTE MOUNTAIN SICKNESS • Major symptoms – – – – – Headache Fatigue Dizziness Anorexia Dyspnea (but tricky!) • Incidence and severity depend on – – – – – Rate of ascent Altitude attained Length of time at altitude Degree of physical exertion Individual’s physiological susceptibility • Treatment hardly needed • Only a problem if progression of symptoms to those of – HAPE – HACE HIGH ALTITUDE PULMONARY EDEMA (HAPE) • Noticed only after 24-48hr and occurs after the 2nd night • Occurs in otherwise healthy people without known cardiac or pulmonary disease – 1:50 climbers on McKinley succumb to HAPE (Hackett et al., 1990) • Occurs when people go rapidly to high altitude • Extravasation of fluid from the intra- to extravascular space in the lung WHY DOES HAPE OCCUR ? • Hypothesis 1. Pulmonary hypertension • Strong relationship between the development of HAPE in people with – Mild pulmonary hypertension at rest – Accentuated pulmonary vascular response to hypoxia or exercise • But pulmonary hypertension alone is not enough to result in HAPE (Sartori et al., 2002) • There is strong evidence that HAPE is due to patchy capillary damage due to pulmonary hypertension (West JB, 2004) WHY DOES HAPE OCCUR ? • Hypothesis 2. Pulmonary endothelium barrier fragility – Pulmonary endothelium barrier susceptible to • Mechanical stress Stretching of the endothelium gaps passage of proteins and red blood cells • Inflammation Mediators release permeability gaps passage of proteins, red blood cells and inflammatory mediators • Questions: – inflammation = 1st culprit – High pressure alone enough to result in extra vascular leak ? INFLAMMATION IN HAPE ? • Schoene et al., 1986, 1998 – [Leukotrienes] (marker of inflammation) very high in BAL in subjects acutely ill with HAPE • But is inflammation present at the start or as a result of HAPE ? • Swenson et al., 2002 – RBC and proteins present in BAL in people at onset of HAPE – But no inflammatory markers present Inflammation probably not the causative factor Swenson et al., 2002 HYPOXIC PULMONARY VASOCONSTRICTION hypoxia • The stress failure Alveolar theory (West et Mathieu-Costello, 1998, 99) Hypoxic pulmonary vasoconstriction (uneven) VA/Q heterogeneity capillary pressure (some capillaries) Damage to capillary wall (stress failure) EDEMA Exposed basement membrane Inflammatory mediators West, JB. Annals Intern Med, 2004, 141:789-900 EXERCISE-INDUCED HYPOXEMIA EXERCISE +/- Alveolar hypoxia Hypoxic pulmonary vasoconstriction (uneven) VA/Q heterogeneity capillary pressure (some capillaries) Damage to capillary wall (stress failure) EDEMA Exposed basement membrane Inflammatory mediators O2 in about ½ endurance MORE HYPOXEMIAresults athletes (Powers et al., 1988) INTEGRITY OF PULMONARY BLOOD-GAS BARRIER IN ATHLETES • Hopkins et al., 1997 – BAL in 6 athletes after a 7min exercise at maximal intensity – Post exercise: • • • • RBC Total protein Albumin Leukotrienes B4 > control subjects at rest • Hopkins et al., 1998 – 1h at 70% VO2max no signs of alteration Impairment of the integrity of blood-gas barrier only at extreme level of exercise in elite athletes Circular break of the epithelium Full break of the blood-gas barrier Costello et al., 1992 Red cell moving out of the capillary lumen (c) into an alveolus (a) West et al., 1995 WHY DOES HAPE OCCUR ? • Hypothesis 3. Perturbation of alveolar fluid clearance • Role of fluid in extravascular space depends on: – Its accumulation – Efficiency of its rate of clearance • Hypoxia Na,K-ATPase activity (Dada et al., 2003) PREVENTION OF HAPE • Don't climb at high altitude!!!! • Undergo hypoxic ventilation test to determine natural fitness for high altitude • If not fit, undergo training, and plan for slow ascent (At altitudes above 3000 m individuals should climb no more than 300 m per day with a rest day every third day) • Avoid strenuous physical exertion • Anyone suffering symptoms of acute mountain sickness should stop, and if symptoms do not resolve within 24 hours descend at least 500 m. TREATMENT OF HAPE • Get the patient down in lower altitude as fast and as low as possible • Give O2 or hyperbaria • Apply expiratory positive airways pressure – With a respiratory valve device – Or by pursed lips breathing • Treat like any other case of pulmonary edema; in some cases, antibiotics may be needed SPECIFIC TREATMENT OF HAPE • Acetazolamide, oral 125-250 mg 2x/day • Dexamethasone, oral. I.M. or I.V. 2 mg q 6hrs or 4 mg q 12 hrs. • Nifedipine, oral 20-30 mg long-acting, q 12 hrs. • Tadalafil oral 50 mg. 2x/day • Sildenafil 50 mg q 8 hrs • Salmeterol inhaled 125mg 2x/day Medication Acetazolamide Renal Insufficiency Avoid if GFR <10 Hepatic Insufficiency Pregnancy Other Issues Contraindicated Category C Avoid if w/ concurrent longterm aspirin; cuation with sulfa allergy; avoid concurrent Kwasting diuretics and ophthalmjic CAI mL/min, metab acidosis, hypoK, hypercalcemia, & hyperphosphatemia Dexamethasone No C.I.; No dose adjustments No C.I.; No dose adjustments Category C May increase FBS in diabetics; avoid in PUD or GO-bleed risk patients Nifedipine No C.I.; No dose adjustments Best to avoid; if use necessary, 10 mg B.I.D. Category C Caution PUD or GO-bleed risk or gastroesoph varices patients Tadalafil 5mg if GFR 30-50 mL/min. Max 10 mg; <5 if GFR < 30mL/min. Child's Class A & B = 10mg/dL; Child's class C= don't use Category B Incr. Risk of GERD; caution Same dose adj as Tadalafil Decrease dose; start with 25 mg; avoid use if with g-e varices Category B No C.I.; No dose adjustments Insufficient data; best to avoid Category C Sildenafil Salmeterol with other meds affecting cP450; avoid concurrent nitrates and B-blockers Incr. Risk of GERD; caution with other meds affecting cP450; avoid concurrent nitrates and B-blockers Potential for adverse reaction in pts w/ CAD prone to arrhythmia; avoid concurrent beta-blockers, monoamine oxidase inhibitors, or tricyclic antidepressants Luks and Swenson, Chest, 2008; 133: 744-755 Medication Malaria Traveler's Diarrhea Acetazolamide No known interactions with prophylaxis med, but could increase serum quinine concentration No interactions with fluroquinolones or macrolides; Dexamethasone No known interactions with prophylaxis or treatment meds Potential increased risk of tendon injury Nifedipine No reported interactions with prophylaxis or treatment med, except mefloquine Avoid clarithromycin; safe to use azithromycin and fluroquinolones Tadalafil No reported interactions with prophylaxis or treatment med, except mefloquine Avoid clarithromycin; safe to use azithromycin and fluroquinolones Sildenafil No reported interactions with prophylaxis or treatment med, except mefloquine Avoid clarithromycin; safe to use azithromycin and fluroquinolones Salmeterol Avoid chloroquine due to increased risk of QT- interval prolongation and ventricular arrhythmia. Other agents safe to use Avoid clarithromycin; safe to use azithromycin and fluroquinolones Luks and Swenson, Chest, 2008; 133: 744-755 KEY POINTS • High altitude = stressful environment for the lungs – At extreme altitudes : lung = primary and essential organ for human function and survival • HAPE = potentially lethal form of AMS – Extravasation of fluid from the intra- to extravascular space in the lung – Main mechanism involved: pulmonary hypoxic vasoconstriction Capillary stress failure • Exercise-induced hypoxemia at sea level shows a similar pattern Summary • • • • • Respiration is directly tied to metabolism, and physical and physiologic principles High Pressure and Altitude pose problems for Respiration, which reach the limits of normal physiology Different animals, including man, respond to high altitude through adaptation and/or acclimatization; Gene regulation of Hemoglobin evolves more quickly than structural changes Acute ascent to high altitude poses clinical problems that could lead to various forms of acute mountain sickness (AMS) which, like HAPE, may be fatal Prevention and early recognition of symptoms of HAPE important, for prompt treatment Summary • Best treatment is prevention • Specific treatment modalities helpful, but not always successful • Best treatment is descent from high altitude. • Other supportive treatment similar to any capillary leak pulmonary edema is often necessary RECOMMENDED REFERENCES BOOK • Ward et al. High altitude medicine and physiology. 3rd edition. Arnold. 2000 ARTICLES • Hopkins et al. Intense exercise impairs the integrity of the pulmonary blood-gas barrier in elite athletes. Am J Respir Crit Care Med. 1997;155(3):1090-4. • West JB et al. Pathogenesis of high-altitude pulmonary oedema: direct evidence of stress failure of pulmonary capillaries. Eur Respir J. 1995;8(4):523-9. • Schoene. Unraveling the mechanism of high altitude pulmonary edema. High Alt Med Biol. 2004;5(2):125-35. • West, JB. The Physiologic Basis of High Altitude Diseases. Annals Intern Med, 2004, 141:789-900 • Luks and Swenson, Chest, 2008; 133: 744-755 • Martin, et al. Variattion in human performance in the hypoxi mountain environment. Exp Physiol, 2010; 953: 463-470