Altitude - Related Illnesses
advertisement

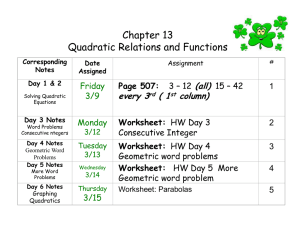
Altitude - Related Illnesses Jim Holliman, M.D., F.A.C.E.P. Professor of Military and Emergency Medicine Uniformed Services University of the Health Sciences Clinical Professor of Emergency Medicine George Washington University Bethesda, Maryland, U.S.A. Altitude - Related Illnesses Acute Mountain Sickness (AMS) High Altitude Pulmonary Edema (HAPE) High Altitude Cerebral Edema (HACE) High Altitude Retinopathy High Altitude Peripheral Edema Acute Mountain Sickness : Incidence Sudden ascent > 10,000 feet (3000 meters) : 30 % Sudden ascent > 14,000 feet : 75 % Report from Colorado ski resort : 12 % Can occur in those with no prior problems with altitude exposure Can recur (no consistent tolerance or "immunity") Acute Mountain Sickness : Etiology Typically occurs at altitude > 8000 feet Rarely occurs at altitude 6000 to 8000 feet No predeliction based on gender More likely if : –Rapid ascent –Lack of acclimatization Situations Predisposing to Possible Acute Mountain Sickness Prolonged non-pressurized aircraft or balloon flight Colorado or Utah ski resorts –Base altitude for most is about 8000 feet Yellowstone National Park –base altitude 7000 to 7500 feet Medellin and Bogota, Colombia –base altitude > 9000 feet Wall mounted oxygen in hotel in Lhasa, Tibet (altitude 13,000 feet) Relationships of the Different Forms of Altitude Illness Altitude illness may be an interrelated spectrum : AMS HAPE HACE Acute Mountain Sickness : Pathophysiology Much individual variation in susceptibility Basically due to hypobaric hypoxia of altitude Also involves tendency for fluid retention (effect of antidiuretic hormone) Barometric pressure versus altitude Arterial Blood Gas Values in Normal Adults at Different Altitudes Altitude PaO2 O2 Saturation PaCO2 (per cent) Sea Level 90 to 95 96 40 5000 feet 75 to 81 95 32 to 33 7500 feet 69 to 74 92 to 93 31 to 33 15,000 feet 48 to 53 86 25 20,000 feet 37 to 45 76 20 25,000 feet 32 to 39 68 13 29,029 feet * 26 to 33 58 9.5 to 13 * (the top of Mt. Everest) Relative hypoventilation Sleep disordered breathing s Acute Mountain Sickness : Exacerbating Factors Sudden ascent Exertion soon after arrival Alcohol intake Sedatives (sleeping pills) Narcotics Note : youth and / or prior conditioning are NOT uniformly protective Acute Mountain Sickness : Symptoms Headache Nausea Anorexia Lassitude "Like a hangover" Insomnia Decreased urination Onset typically 8 to 24 hours after ascent Acute Mountain Sickness : Differential Diagnosis Dehydration Hypothermia Exhaustion Respiratory infection Hyperventilation syndrome Psychiatric disorders Drug intoxication Carbon monoxide poisoning (as from tent heaters or stoves) Acute Mountain Sickness : Prophylaxis Acclimatization –Staging of ascent –Delaying exertion Medication choices : –Acetazolamide (Diamox) 250 mg PO bid or tid –Dexamethasone (Decadron) 4 mg PO tid or qid –Should start either med 24 hours prior to ascent Physiologic adaptation to altitude Acute Mountain Sickness : Treatment of the Established Syndrome Usually resolves in 1 to 3 days even without Rx or descent Sx will improve however with descent If severe Sx, start acetazolamide 250 mg PO bid or tid, or dexamethasone 4 mg PO tid to qid Resting is the most important treatment Progression of Acute Mountain Sickness If ascent is continued or accelerated by a patient with untreated AMS, HAPE or HACE may occur and death may result High Altitude Pulmonary Edema (HAPE) Is a non-cardiogenic pulmonary edema related to altitudinal hypoxia Can be fatal if patient is unable to descend Occurs in 1 to 2 % of patients quickly ascending to > 12,000 feet Can occur even in well fit and acclimatized individuals High Altitude Pulmonary Edema : Onset Usually begins 24 to 72 hours after arrival at altitude Can occur, but uncommon, at altitude 8000 to 12,000 feet Onset usually at night High Altitude Pulmonary Edema in Longterm Mountain Residents H.A.P.E. has been reported in patients acclimatized to high altitude who went to low altitude for > 10 days, & then returned to high altitude Termed "reentry pulmonary edema" Abrupt ascent High Altitude Pulmonary Edema : Symptoms Usual sequence : –Cough dyspnea at rest achy chest pain progressive cough progressive rales frothy sputum hemoptysis frank respiratory failure Chest X-ray appearance is variable : –Patchy infiltrates (often right > left) –If severe, may be bilateral "whiteout" High Altitude Pulmonary Edema : Treatment Most important : Rapid descent : at least 2000 feet High flow O2 ; CPAP mask if available Have patient avoid exertion on descent (other people should carry him / her) Can give acetazolamide or dexamethasone but these do not help much or obviate the need for descent Can try bag pressure chamber if available but still need descent High Altitude Cerebral Edema (HACE) Less common than HAPE Possibly a malignant form of AMS Can be fatal or result in permanent neurologic disability (stroke-like syndromes) Onset is gradual : usually over 2 to 3 days High Altitude Cerebral Edema : Symptoms Severe headache Confusion Agitation / irritability Nausea / emesis Ataxia Hallucinations Seizures Coma High Altitude Cerebral Edema : Field Treatment ONLY effective treatment is descent : at least 3000 feet Rx adjuncts : –High flow O2 / hyperventilation –Dexamethasone / acetazolamide –Furosemide / mannitol –Benzodiazepines / diphenylhydantoin if seizures occur –Avoid exertion during descent –Hyperbaric bag if available In-Hospital Treatment of Suspected HAPE or HACE Airway / breathing / circulation High flow oxygen +/- intubation & hyperventilation Chest X-ray IV dexamethasone & acetazolamide Check ABG & carboxyhemoglobin Consider tox & drug screen Head CT if abnormal mental status Admit to ICU Consider hyperbaric O2 Rx (call nearest chamber) High Altitude Retinal Hemorrhage Incidence is 20 to 40 % above 14,000 feet Usually does not affect vision (unless macular bleed) Usually asymptomatic Diabetics at higher risk Usually no Rx or descent needed High Altitude Peripheral Edema Shows as edema of : –Face –Eyelids –Hands –Feet –Lower legs No Rx usually needed (can use diuretic effect of acetazolamide if patient uncomfortable) Miscellaneous Altitude Related Medical Problems Tendency to venous thrombosis & pulmonary emboli (partly due to polycythemia of altitude exposure) Immune suppression –probably related to tissue hypoxia –wounds slower to heal & more likely to get infected –wound infections can show antibiotic resistance High Altitude Flatus Expulsion (HAFE) –Reference : Auerbach & Geehr, 1989, pg. 25 –No serious sequelae noted to date "Snow Blindness" (ultraviolet light exposure) Preexisting Illnesses Aggravated by High Altitude C.O.P.D. Coronary artery disease Peripheral vascular disease Hypertension –Variable worsening in some patients Sickle cell disease Pregnancy –Preeclampsia, but not other complications of pregnancy, is more common at altitude Skin Problems Related to High Altitude Exposure Shorter time for sunburn to occur to exposed skin Tendency to drying ; thereby more risk of chilblains or pernio Slower wound healing & higher wound infection rate ; prevention of even minor skin injuries (especially friction blisters) is therefore important Altitude Illnesses : Summary Best treatment is prevention : –Acclimatization / staging ascent –Avoiding alcohol & sedatives –Medication prophylaxis If symptoms suggest HAPE or HACE : –start oxygen –arrange immediate assisted descent –definitive followup care in a medical facility after descent, even if symptoms abate Ultraviolet Light Keratitis ("Snow Blindness") UV radiation increases 4 % for every 300 meters increase in altitude Cornea absorbs UVB (below 300 nm) Lens cataracts can result from chronic exposure to UV radiation > 300 nm High exposure levels can cause corneal burn in < 1 hour Symptoms usually take 6 to 12 hours to develop (same as for "welders' arc keratitis") Snow Blindness Symptoms & Signs Eye pain Gritty sensation of eyes Light sensitivity Tearing Conjunctival injection Chemosis Eyelid swelling Snow Blindness : Treatment Remove contact lenses Topical anesthetic : single dose only –Tetracaine or proparacaine –Repetitive use may damage cornea Ophthalmic antibiotic ointment –Erythromycin, gentamicin, or sulfacetamide Eye patch for 12 to 24 hours Most should heal in < 24 hours May need oral narcotics for pain Snow Blindness : Prevention Should choose sunglass lenses that are rated to transmit < 10 % of UVB Side shields or full goggles needed to prevent exposure from side bounce Sunglasses should always be secured with a neck loop when mountain climbing If sunglasses are lost, makeshift protective shields can be made by cutting thin slits in pieces of cardboard Snow Avalanches : Medical Relevance About 100,000 release annually in U.S. About 100 of these cause injury, death, or major property damage About 140 people in U.S. are caught each year Reported average of 12 major injuries & 17 deaths annually Persons at risk include skiers, snowmobilers, highway plow operators, and forest rangers & game wardens Physical Characteristics of Avalanches Typical velocities are 50 to 100 miles per hour Can be as fast as 200 miles per hour Can generate impact pressures > 150 lbs/square inch (can destroy even concrete structures) Occur with greatest frequency on slopes of 30 to 45 degrees Causes of Death from Avalanches Direct impact trauma of snow blocks or ice Indirect trauma of hitting against objects such as trees or rocks Hypoxia from encasement in snow Hypothermia Restrictive chest compression Prevention of Death or Injury from Avalanches Have group spread out when approaching or crossing avalanche terrain Have rescue poles, colored cords, & avalanche rescue beacons or transceivers ready Always try to escape an avalanche to the side (not downhill away from the avalanche) If caught & tumbled, keep your hands up near your face