Diagnostic Indicators of Anxiety and Depression in Older
advertisement
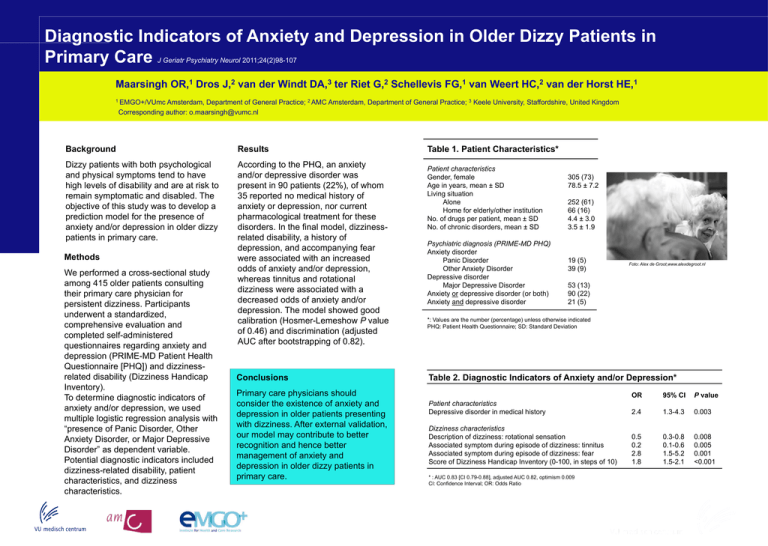
Diagnostic Indicators of Anxiety and Depression in Older Dizzy Patients in Primary Care J Geriatr Psychiatry Neurol 2011;24(2)98-107 Maarsingh 1 OR, Dros 2 J, van der Windt 3 DA, ter Riet 2 G, Schellevis 1 FG, van Weert 2 HC, van der Horst 1 HE, 1 EMGO+/VUmc Amsterdam, Department of General Practice; 2 AMC Amsterdam, Department of General Practice; 3 Keele University, Staffordshire, United Kingdom Corresponding author: o.maarsingh@vumc.nl Background Results Dizzy patients with both psychological and physical symptoms tend to have high levels of disability and are at risk to remain symptomatic and disabled. The objective of this study was to develop a prediction model for the presence of anxiety and/or depression in older dizzy patients in primary care. According to the PHQ, an anxiety and/or depressive disorder was present in 90 patients (22%), of whom 35 reported no medical history of anxiety or depression, nor current pharmacological treatment for these disorders. In the final model, dizzinessrelated disability, a history of depression, and accompanying fear were associated with an increased odds of anxiety and/or depression, whereas tinnitus and rotational dizziness were associated with a decreased odds of anxiety and/or depression. The model showed good calibration (Hosmer-Lemeshow P value of 0.46) and discrimination (adjusted AUC after bootstrapping of 0.82). Methods We performed a cross-sectional study among 415 older patients consulting their primary care physician for persistent dizziness. Participants underwent a standardized, comprehensive evaluation and completed self-administered questionnaires regarding anxiety and depression (PRIME-MD Patient Health Questionnaire [PHQ]) and dizzinessrelated disability (Dizziness Handicap Inventory). To determine diagnostic indicators of anxiety and/or depression, we used multiple logistic regression analysis with “presence of Panic Disorder, Other Anxiety Disorder, or Major Depressive Disorder” as dependent variable. Potential diagnostic indicators included dizziness-related disability, patient characteristics, and dizziness characteristics. Conclusions Primary care physicians should consider the existence of anxiety and depression in older patients presenting with dizziness. After external validation, our model may contribute to better recognition and hence better management of anxiety and depression in older dizzy patients in primary care. Table 1. Patient Characteristics* Patient characteristics Gender, female Age in years, mean ± SD Living situation Alone Home for elderly/other institution No. of drugs per patient, mean ± SD No. of chronic disorders, mean ± SD Psychiatric diagnosis (PRIME-MD PHQ) Anxiety disorder Panic Disorder Other Anxiety Disorder Depressive disorder Major Depressive Disorder Anxiety or depressive disorder (or both) Anxiety and depressive disorder 305 (73) 78.5 ± 7.2 252 (61) 66 (16) 4.4 ± 3.0 3.5 ± 1.9 19 (5) 39 (9) Foto: Alex de Groot,www.alexdegroot.nl 53 (13) 90 (22) 21 (5) *: Values are the number (percentage) unless otherwise indicated PHQ: Patient Health Questionnaire; SD: Standard Deviation Table 2. Diagnostic Indicators of Anxiety and/or Depression* OR 95% CI P value Patient characteristics Depressive disorder in medical history 2.4 1.3-4.3 0.003 Dizziness characteristics Description of dizziness: rotational sensation Associated symptom during episode of dizziness: tinnitus Associated symptom during episode of dizziness: fear Score of Dizziness Handicap Inventory (0-100, in steps of 10) 0.5 0.2 2.8 1.8 0.3-0.8 0.1-0.6 1.5-5.2 1.5-2.1 0.008 0.005 0.001 <0.001 * : AUC 0.83 [CI 0.79-0.88], adjusted AUC 0.82, optimism 0.009 CI: Confidence Interval; OR: Odds Ratio