Obesity Hypoventilation Syndrome
advertisement

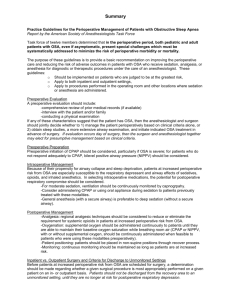
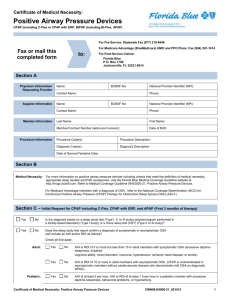
Obesity Hypoventilation Syndrome Pickwickian Syndrome Obstructive sleep apnea was called the Pickwickian syndrome in the past because Joe the Fat Boy who was described by Charles Dickens in the Pickwick papers had typical features with snoring, obesity, sleepiness and “dropsy”. OHS: Definition - Obesity (BMI 30 kg/m2) - Hypercapnia (PaCO2 45 mmHg) - Sleep-disordered breathing Thomas Nast, The Pickwick Papers OHS: Clinical Presentation • • • • Middle-aged 2:1 male-to-female Extremely obese Significant sleep-disordered breathing (fatigue, hypersomnolence, snoring, AM headache) OHS: Epidemiology • Prevalence among OSA: 10-20% • No clear ethnic or racial predominance In USA, prevalence of OSAS among middle-aged men and women were 4% and 2% (Young et al) OHS: Hypercapnia • Increased CO2 production • Decreased respiratory drive (will not breathe) • Respiratory pump malfunction or increased airway compliance (cannot breathe) • Inefficient gas exchange Obesity Leptin resistance Increased mechanical load and weak respiratory muscles OSA Upper airway resistance Acute hypercapnia during sleep Blunted ventilatory response Chronic hypercapnia Increased serum bicarbonate Mokhlesi, B et al., Recent Advances in Obesity Hypoventilation Syndrome, Chest OHS: Lung Volumes TLC TLC TV TV RV RV OHS: Lung Volumes Volume Lungs TLC TLC Chest Wall FRC FRC RV RV Pressure Mechanism of OSAS • The upper airway dilating muscles,like all striated muscles-normally relax during sleep. • In OSAS, the dilating muscles can no longer successfully oppose negative pressure in the airway during inspiration. • Apneas and hypopneas are caused by the airway being sucked and closed on inspiration during sleep. Anatomy of OSA NORMAL SNORING SLEEP APNEA Symptoms of OSA,OHS Night time • • • • • • • • • Snoring Witnessed apnoea Frequent nocturnal awakenings Waking up choking or gasping for air Unrefreshed sleep Restless sleep nocturia Dry mouth decreased libido Symptoms of OSA,OHS Daytime • • • • • • • Early morning headaches Fatigue Daytime sleepiness Poor memory, concentration or motivation Unproductive at work Falling asleep during driving Depression Symptoms of Sleep Apnea Syndrome Features of Excessive Sleepiness Motor vehicle crashes Work related accidents Impaired school or work performance Marital problems Memory and concentration difficulties Depression Impaired quality of life OHS,OSA & Cardiovascular Diseases • Uncontrolled HTN- 83% have OSAH; activation of sympathetic drive. • Acute coronary syndrome- 40-50% has OSA • Cardiac arrhythmias mostly Af • Heart Failure • Sudden cardiac death • Stroke OSA,OHS and DM • Patients from the sleep clinic with AHI>10 are much more likely to have impaired glucose tolerance and diabetes (Meslier et al Eur Respir J 2003) Diagnosis • A good sleep history • Assessment of obesity, oral cavity • Assessment of possible predisposing causes: HTN, hypothyroidism, acromegaly and • Polysomnography: gold standard tool Polysomnography • • • • • • • • EOG - Electrooculogram EEG - Electroencephalogram EMG - Electromyogram EKG - Electrocardiogram Tracheal noise Nasal and oral airflow Thoracic and abdominal respiratory effort Pulse oximetry Overnight PSG Apnea-Hypopnea Index • Apnoea-hypopnoea index (AHI)= number of apnea/hypopnea per hour of sleep • AHI<5 Normal • AHI 5-15 Mild OSA • AHI 15-30 Moderate OSA • AHI >30 Severe OSA OHS: Treatment • PAP (CPAP or BiPAP) – No standard protocol for titration • Oxygen therapy • Surgery – Tracheostomy – Weight reduction • Pharmacotherapy – Medroxyprogesterone – Acetazolamide Behavioral Treatments 1. Attain an ideal body weight 2. Sleep on the side 3. Avoid sedative medication before sleep 4. Avoid being sleep deprived 5. Avoid alcohol before sleep 6. Elevate the head of the bed 7. Promptly treat colds and allergies 8. Avoid large meals before bedtime 9. Stop smoking Body Position • Raise HOB • Avoid supine position Strategies• Tennis ball in pajamas • Backpacks CPAP Therapy • Works as a pneumatic Splint • 1st choice of treatment in moderate to severe OSAHS • Success rate 95-100% • Long term compliance 60-70% • Retitrate pressure if needed Oral Appliances □ Not yet available in Iran □ Appropriate first-line treatment for Mild OSA, primary snoring, upper airway resistance syndrome ( UARS ) □ Not as effective as CPAP, 52% OSA have AHI<10% □ Young, non-obese □ Second line therapy for moderate-severe OSA □ Patient’s choice - Not tolerating / refuse to use CPAP, or are not surgical candidates MAD TRD Medical Treatments 1. Weight loss 2. Pharmacological 3. Oxygen therapy 4. Nasopharynegeal intubation 5. Nasal CPAP 6. BiLevel CPAP 7. Automatic CPAP 8. Oral Appliances 9. Atrial Pacing Oxygen Therapy • Improves oxygen saturation during sleep • May prolong apneic episodes • Reduces cardiac arrythmias • Useful additive treatment with CPAP • Rarely reduces apneic episodes • Can improve daytime sleepiness • May cause CO2 retention Pharmacological Therapy Protriptyline Medroxyprogesterone Fluoxetine Antihistamines Nasal Steroids Theophylline Acetazolamide Modafinil Magalang UJ et al, 2003 Conclusion • With the increasing problem of obesity, the impact of undetected OHS & OSAS as a public health burden cannot be undermined among our population, • It merits appropriate preventive and treatment strategies. references Mokhlesi, B., Tulaimat, A. (2007), “Recent Advances in Obesity Hypoventilation Syndrome”, Chest 132 (4),1322-1332. Weinberger, S.E., Drazen, J.M., “Disturbances in Respiratory Function”, in Kasper et al (eds), Harrison’s Principles of Internal Medicine (16th Edition), New York: McGraw-Hill, pp. 14981505. Guyton, A.C., Hall, J.E. (2000), Textbook of Medical Physiology (10th edition), Philadelphia: W.B. Saunders.