FT Course presentation - pbcc
advertisement

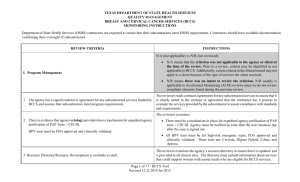
Free Treatment and Full Medical Coverage for Women with Breast or Cervical Cancer at no cost to facilities that accept Medicaid Online Course PowerPoint Presentation What we’ll cover How women with breast or cervical cancer can receive free treatment and full medical coverage for and during their treatment when they have no insurance or the plan they have is limited The role that doctors and nurses play in helping women receive free medical coverage Procedures for processing forms and helping women apply The criteria women must meet to become enrolled What we’ll cover What’s meant by creditable coverage The basics of the Commonwealth of PA’s Breast and Cervical Cancer Prevention and Treatment Program (BCCPT) Important facts to help you assist your patients Where to turn for more information Who are we concerned about? Women in Pennsylvania who have been diagnosed with breast or cervical cancer or diagnosed with a precancerous condition Have limited or no health insurance to pay for their treatment, tests, and medications There are over 12,000 women diagnosed with breast cancer in Pennsylvania each year. OVER A HALF-MILLION WOMEN ARE WITHOUT ADEQUATE INSURANCE COVERAGE TO TREAT THEIR CANCER IN PA. WOMEN WITHOUT INSURANCE ARE SIGNIFICANTLY MORE LIKELY TO DIE OF THEIR CANCER THAN WOMEN WHO ARE INSURED. So how can women get help? Knock on one door at the Pennsylvania Department of Health How does she get to the door? Through her doctor when… The doctor has diagnosed her with breast or cervical cancer OR A precancerous condition - a disease, syndrome, or finding that, if left untreated, may lead to cancer How does she get to the door? Through her doctor when… She informs the doctor that she doesn’t have health insurance or her plan is very limited. The doctor informs her that she may be eligible for free medical coverage and fills out a form and faxes it to begin the application process. What form and where is sent? The form is known as PA 600B You can get copies of it at www.pahealthywoman.com (at bottom of page under the quick links section “Healthcare Providers”) It takes only a few minutes to fill out. The woman fills out Part A of the Enrollment and Consent form. What form and where is sent? The physician fills out Part B which is the Medical Assistance Eligibility section. The form is faxed to one central statewide number at 412-201-4702. Where does the form go? It’s processed by the PA Department of Health’s statewide contractor and if the woman meets the eligibility criteria it is then sent on to the woman’s local County Assistance Office. The County Assistance Office has 5 business days from the day they receive the application to determine if the woman is eligible. What eligibility criteria is the County Assistance Office looking for? Criteria The PA 600B form Pennsylvania resident A Social Security Number Under the age of 65 years Criteria A United States Citizen However, if a non-citizen or undocumented woman has a precancerous condition or is diagnosed with breast or cervical cancer she can apply for “Emergency Medical Assistance” from her local County Assistance Office. For Medical Assistance information call the Welfare Helpline at 800-692-7462 or the Medicaid Helpline at 800-842-2020. If she is accepted, non-citizen or undocumented woman can only receive treatment specific to either breast or cervical cancer. For Immigration and non-citizen information contact the Pennsylvania Health Law Project at 800-274-3258 or www.phlp.org. Criteria Without insurance OR Underinsured or limited coverage This means that a woman’s plan does not adequately cover treatment for breast or cervical cancer. In other words, the woman’s plan is not creditable to what a woman can receive from the Full Medical Coverage program. Creditable means a plan is equal to or better than what it is being compared to. Here are some examples of how a plan is not creditable: The plan’s lifetime or annual limits have been exhausted. A woman is in a waiting period for an HMO. She has only Medicare Part A for hospitalization coverage, and thus, isn’t insured for outpatient treatment. Criteria Examples of creditable plans, meaning a woman would not qualify for the program if she has any of these plans: Medicare Medicaid (State Medical Assistance) Armed forces insurance A state health risk pool A group health plan Health insurance coverage (e.g. HMO, private plan) Criteria Has an income of no more than 250% of the Federal Poverty Level (FPL). The Department of Health and Human Services issues the annual FPL guidelines each year. The benefit levels of many low-income assistance programs are based on these poverty guidelines. Criteria Federal Poverty Level (FPL) In 2011, the FPL for a family of two was a gross annual income of $14,710. To calculate 250%, simply double the amount ($29,420) and then add half of $14,710 ($7350.00) which equals $36,775. A woman’s assets are NOT counted towards her income. You can find annual FPL charts by going to www.hhs.gov and entering “poverty guidelines” in the search bar. If a woman qualifies she will receive Free and Full Medical Coverage provided by the: COMMONWEALTH OF PA’S BREAST AND CERVICAL CANCER PREVENTION AND TREATMENT PROGRAM PA DEPARTMENT OF PUBLIC WELFARE Her coverage begins the day she was diagnosed with a precancerous or cancerous condition • Her eligibility can be retroactive up to three months prior to enrollment. • However, all eligibility requirements under BCCPT must be met during the retroactive period, including screening and diagnosis of breast or cervical cancer. Once she’s enrolled in the program THIS IS WHAT SHE RECEIVES… Free and Full Medical Coverage She receives a PA Medicaid Access Card providing: Health care coverage for any health conditions while she is being treated for breast or cervical cancer. Medical Treatment for her cancer such as surgery, chemotherapy, radiation, medications. Physician visits. No limits on visits. No co-pays. No premiums. Screening for other Medical Assistance Benefits such as free transportation for medical visits. This program is a Medicaid Program IT IS A FEE-FOR-SERVICE PROGRAM NOT AN HMO. AS A RESULT, A WOMAN CAN RECEIVE SERVICES ANYWHERE IN THE STATE, NOT ONLY WHERE SHE RESIDES. What physicians should do Whenever he or she diagnoses a patient with breast or cervical cancer, ask if the patient has insurance. If they don’t or if there is any doubt that the insurance she does have isn’t creditable to cover her treatment -- then tell the patient and the nurse manager about the BCCPT program. Offer to fill out the necessary paperwork and fax it to the statewide number at which point DPW’s Health Insurance Premium Payment Program reviews policies for creditable coverage. What physicians should do Every year women must re-enroll and they need the doctor to submit PA600BR (renewal form) that verifies she needs continued treatment for breast or cervical cancer or precancerous condition of the breast or cervix. When valid, the doctor should write that “the cancer is persistent and incurable” so the patient can receive treatment during the duration of her cancer. Once a woman is in the Breast and Cervical Cancer Prevention and Treatment program this is what you should know… What Women Need To Know The coverage for the program is for the duration of her cancer treatment. Women must continue to sign up for the program every year once they have been enrolled. If they do not, they will be removed from the program. This means the doctor’s office needs to fill out their section of the PA 600B every year when the patient brings it in. Women rely on their doctor submitting the papers quickly. What Women Need To Know Depending on the woman’s diagnosis (ICD code), she may need to complete a partial renewal more frequently. For example, women with cervical cancer as long as “active treatment” is needed renew every three months. The PA600BR renewal form is sent directly to the patient and they’ll need the doctor to complete their portion and sign it. What Women Need To Know If a woman receives a letter from the Department of Welfare that her Medical Assistance via the BCCPT program will terminate, she should get as many health care services that she needs (such as annual exams, dental care). She can appeal if she is denied. What Nurses And Doctors Need To Know Remind women that even though this is a Medical Assistance program, they can have higher incomes than the standard eligibility requirements. Her assets (home, car, savings) will not be affected or counted as income. You’ll help them through the fear of applying for “welfare.” If there is ANY question about a woman’s eligibility or coverage we encourage you to help her apply for this program! Program case managers can help navigate the process. What Nurses And Doctors Need To Know Your physician’s office is key in letting women know about the program and processing the initial paperwork for them to enroll. When a woman is enrolled – all of her health care is covered for any type of condition throughout the duration of her cancer treatment. What Nurses And Doctors Need To Know A woman remains in the BCCPT program until all treatment is completed, including while a patient is taking tamoxifen. Needing follow-up exams and tests does NOT qualify as “in treatment.” A woman’s medications and chemotherapy are covered. Note: the medication must be administered in a hospital outpatient clinic, not in a doctor’s office or a cancer center. What Nurses And Doctors Need To Know Any pharmacy that accepts Medicaid will provide needed drugs/medications to eligible women. For all pharmacy questions as to what’s covered call the Pharmacy Call Center at 800-558-4477 and choose Option 1. Final Points A woman’s BCCPT benefits end when she: Reaches age 65 years Has creditable coverage No longer needs breast or cervical cancer treatment Does not comply with annual renewal requirements Final Points The BCCPT program is a federal Medicaid Program (Title XIX) administered by the PA Department of Public Welfare. Be sure to print the Resource Guide for resources and contact information that can help you assist your patients receive full medical coverage for breast or cervical cancer. If there is ANY question about a woman’s eligibility or coverage we encourage you to help her apply for this program! Final Points If you have any questions or need help please call the PA Breast Cancer Coalition at 717-721-2580 or 800-377-8828.