Session Agenda - Collaborative Family Healthcare Association
advertisement

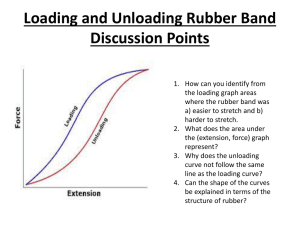
Session D3 October 28, 2011 3:30-4:15 PM How Far Will the Rubber Band Stretch? Implementing New Clinical and Operational Concepts without Additional Resources Samantha Pelican Monson, PsyD, Clinical Psychologist Cheryl Palsic, BSN, RN-BC, Family Practice Nurse Lauren Gray, DO, Family Medicine Chief Resident Collaborative Family Healthcare Association 13th Annual Conference October 27-29, 2011 Philadelphia, Pennsylvania U.S.A. Faculty Disclosure We have not had any relevant financial relationships during the past 12 months. Need/Practice Gap & Supporting Resources Already strapped healthcare delivery systems are repeatedly expected to implement new cutting edge concepts without additional resources. But how??? Objective Process discussions (such as this presentation) can promote the creativity required to meet implementation expectations without additional resources. Expected Outcome You will leave with new implementation ideas for your respective healthcare delivery systems. Learning Assessment As we share our process with you, we’ll be soliciting your thoughts about how it could inform your implementation approach. Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Our Healthcare Delivery System • Denver’s public safety-net hospital Community Health Services (CHS) • 8 FQHCs • 355,000+ patient visits/year • 20,000+ patient visits/year • Relationship with state refugee clinic • 4-2-2 family medicine residency Our Practice’s New Concept Our Practice’s Primary Implementation Processes • Division of practice into two clinical teams • Establishment of two quality improvement (QI) teams • Identification of three clinically important conditions: – Diabetes – Hypertension – Asthma Our Clinical/QI Team • Green Team • 3-4 Medical Providers (F-NP , MD, and DO) • 3 Residents • 1 Behavioral Health Provider • 1 RN • 3 Medical Assistants • Part-time Patient Navigator • 2 Clerks • Diabetes as designated clinically important condition Our “Diabetes Clinic” • ½ day per month • Patients = identified as uncontrolled (from registry and intra-clinic referrals) • Medical Provider = initially attending with most diabetic patients, later expanded to resident • Behavioral health (psychologist) and diabetes education (RN) follow medical provider • Lab work completed ahead of time • Emphasis on patient self-management Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Our Stakeholders • Lowry Family Health Center – – – – Support Staff Clinical Providers Residents Patients • Community Health Services – Leadership Team Who are your stakeholders? Development Opportunities • HealthTeamWorks training • How to run an effective meeting • Group facilitation skills • QI processes & tools • Motivational interviewing training for all staff and providers • RN joined multidisciplinary Denver Health Diabetes Collaborative What community/institutional programs might you access? Fostering New Leaders • Medical Director and Practice Manager supported RN in becoming leader of Green Team Who in your practice has untapped leadership potential? Sharing the Vision • Clinically important conditions identified through survey of all staff and providers • Clinical and QI teams responsible for own plans • All team members have a role in accomplishing the most important goals – Patient self-management – Integrated behavioral healthcare – Clinical outcomes How can you promote universal ownership? Individual Perks • RN involvement allowed for promotion up her professional ladder and diversification of job duties • Resident involvement fit with self-identified learning objectives What individual rewards exist in your organization? Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Alignment with Residency • P4 Program (Preparing the Personal Physician for Practice) • Long-standing behavioral science curriculum What programs within your system could be leveraged? Capitalizing on Culture • Denver Health’s commitment to Lean Systems Improvement made QI process intuitive • Minimal external behavioral health resources made the clinic “hungry” for integration How can you join instead of change the culture? Balancing Costs and Benefits • Absence of reimbursement for team-based care offset by institutional benefit • Collaborative care helpful for Magnet designation • Staff and provider time justified by institutional initiative • Denver Health was seeking PCMH National Committee for Quality Assurance (NCQA) recognition How could your institution benefit from your project? Creation of Work-Arounds • Registry limitations were supplemented by development of a spreadsheet • Job duty re-allocation allowed for staff to practice “at top of license” on project components • Turn-over of and time restrictions on patient navigator position addressed by RN vigilance How could your system flex around its limitations? Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Start Small • Diabetes clinic began with only eight patients per month • Anecdotal clinical improvement celebrated • Patient feedback highly valued • “I don’t know what it was, but something clicked in me after you all were askin’ me how I was gonna take care of myself. I’ve totally changed how I eat, and my daughter’s helpin’ me!” Around what small changes could your system build momentum? Be Flexible • Regular meetings and huddles allowed for timely problem-solving • Resident allowed to participate in diabetes QI processes and clinical initiatives What areas of rigidity in your system could be re-considered? Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Onward! • Applying diabetes clinic principles to standard patient care • Broadening care focus (e.g., vision and podiatry) • Making diabetes education more interactive • Increasing resident involvement • Impacting future generations of providers What’s in your future? Session Agenda • Introduction/Orientation • What Stretched our Rubber Band? – Engaging Stakeholders – Re-visioning of Systemic Opportunities – “One Step at a Time” Approach • Future Directions • Questions/Discussion Questions/Discussion Session Evaluation Please complete and return the evaluation form to the classroom monitor before leaving this session. Thank you!