feedback reports
advertisement

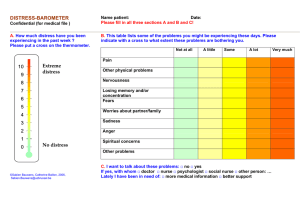
POPULATION RESEARCH SEMINAR SERIES Sponsored by the Statistics and Survey Methods Core of the U54 Partnership Child-Reported Outcomes in Pediatric Advanced Cancer: Are They Helpful? Joanne Wolfe, MD, MPH Division Chief, Pediatric Palliative Care Department of Psychosocial Oncology and Palliative Care Dana-Farber Cancer Institute Director, Pediatric Palliative Care Boston Children’s Hospital POPULATION RESEARCH SEMINAR SERIES Sponsored by the Statistics and Survey Methods Core of the U54 Partnership Questions? Comments? Send us an email! u54.ssmc@gmail.com This study is dedicated to Dr. Jane C. Weeks who served as my primary research mentor. Her wisdom and insightfulness will have a lasting impact on numerous investigators, patients and families for many generations to come. Questions 1. Are children capable of reporting on their own symptoms and quality of life? 2. How do children’s reports vary with developmental stage? 3. What are the effects of feeding back children’s reports to clinicians and parents in children with advanced cancer? Results of the PediQUEST Randomized Controlled Trial Background • Thousands of children are living with advanced cancer, 1400 die annually. (ACS 2012) • Several studies among adults with advanced cancer suggest that presenting providers and patients/families with PROs may improve patient’s HRQoL (Velikova et al JCO 2004, Berry et al JCO 2011) • One study evaluating a web-based PRO feedback intervention (KLIK PROfile) in children with rheumatological illness using a sequential cohort design. (Engelen V et al, Patient Educ Couns 2010) Pediatric Palliative Care Current Research Focus Early Research Focus Hope for cure, life extension, a miracle… Individualized blending of care directed at underlying illness and physical, emotional, social, and spiritual End-oflife care needs of child and family with continuous reevaluation and adjustment Hope for comfort, meaning… Bereavement care Examples of Earlier Studies Percent of Children 100 Symptom Prevalence Suffering Timing of Understanding That Child Had No Realistic Chance for Cure 80 60 40 Duration of disease - 32 months Physician - 7months Parent - 3.5 months 20 0 Wolfe et al. NEJM 2000. Wolfe et al JCO 2008 Wolfe et al. JAMA 2000 PediQUEST Study Pediatric Quality of Life and Evaluation of Symptoms Technology: Computer-based data collection system that collects child (or parent) reported symptoms and QoL and has the ability of generating printed feedback reports and email alerts. The PediQUEST Study Hypothesis Increasing awareness of providers and parents about child’s symptoms and quality of life will decrease the child’s experience of suffering The PediQUEST Study Study Goals 1. To assess the feasibility of performing a randomized controlled supportive care study in a population of children with advanced cancer using child-reported outcomes (Feasibility Study) 2. To describe child-reported symptom distress and quality of life in pediatric advanced cancer (Descriptive Study) 3. Preliminarily assess if routine feedback of symptom and QoL data to providers and families has any effect on child’s symptoms and QOL (Evaluation Study) Enrollment Baseline measurement Individual Randomization (block randomization by site) Control Intervention = control + PedsQL, MSAS and FPS-R At least once a month at most once a week X 3 Months (w/re-enrollment) Descriptive Study + @-mails Satisfaction assessed at 4th and 8th PQ survey The PediQUEST Study Study Population • Inclusion criteria – Children 2 years old – 2 weeks of progressive, recurrent, or non-responsive cancer or decision to not pursue cancer-directed therapy – 1 parent with command of English and able to complete paper and pencil and/or computerized questionnaires • Overall Follow-up – Individual patient follow-up: every 3 month reenrollment, or until death • Target Sample Size – 120 consecutive patients (between the 3 study sites BCH, CHOP, Seattle Children’s) The PediQUEST Study Methods Study Instruments • PediQUEST (children or parents) • At most once a week • Clinic, inpatient ward, home (by phone) • Survey about Caring for Children with Cancer-SCCC (Parents and physicians) • 0-3-6-9 months • Post-death Survey • Satisfaction Surveys (children, parents and physicians) PediQUEST Instruments • MSAS – Adult oncology symptom assessment tool adapted for use in children (Collins et al, JPSM 2000, 2002) – MSAS 7-12, 10-18 and nurse proxy version adapted to PQ-MSAS Proxy full, PQ-MSAS 7-12) and PQ-MSAS proxy-supplemental, PQ-MSAS 13-18 • PedsQL 4.0 TM – Standardized patient self-report and parent-report instrument designed to systematically assess pediatric patient’s HRQoL outcomes. (Varni et al Med Care, 2001) – Consists of a 22-item core measure of HRQoL – Four proxy and three self-report age-adapted versions are available (age groups are 2-4, proxy only; 5-7, 8-12 and 13 and over, each with a selfreport and proxy version available) • Sickness Question – Overall, how have you/your child been feeling during the past week? – Two response scales: 3 point faces scale (5-6 yo), VAS (7 and above), “not sick at all”, “very sick” Instruments, response options, age group and respondent Baseline PQ survey Control arm completed PediQUEST surveys at clinic, hospital or home Feedback intervention same as control + printed reports to providers and families + emails when thresholds reached Feedback report Feedback report Feedback report Results 1. Are children capable of reporting on their own symptoms and quality of life? Willingness to complete PediQUEST • Total PediQUEST surveys administered: 1126 • Surveys answered by children: 96% (of 965 potential child administrations) Proportion of Child Response by Age Child Response by age group 100% 100 29 14 4 0.5 80% 60% Parent Child/Teen 40% 20% 0% 2-4yo 5-6yo 7 yo 8-12 yo 13 yo and above Self-reported symptoms 20 weeks of follow up Prevalence and proportion with moderate to severe distress (n=704 surveys) 0.0% 10.0% 20.0% 30.0% Pain Fatigue Drowsy Irritability Nausea Anorexia Sleep Diarrhea Vomiting Nervousness Sadness Cough Worrying Concentration Itching Skin issues Constipation Dyspnea Image Dry mouth Numbness Sweating Dysphagia Dysuria Mod-Sev distress 40.0% 50.0% 60.0% PediQUEST Symptom Burden during the first twenty weeks of follow-up High symptom burden • 88% of children experienced at least one episode of moderate to high distress in 20 weeks of follow-up (regardless of study arm). • On average, patients reported moderate to high distress from approximately 4.2 symptoms 2. How do children’s reports vary with developmental stage? Consistency increases with age • MSAS and QoL scores correlation increases with age Child 7-12 yo MSAS, mean score (SD) PedsQL, mean score(SD) Spearman correlation 13.1 (13.5) 75.2 (15) -0.35 Teens >=13 yo 10.7 (9.02) 71.9 (15.1) -0.59 Consistency increases with age • Comparison of similar MSAS and QoL items further supports hypothesis Correlation between MSAS and PedsQL comparable items Child 7-12 yo Teens >=13 yo Spearman Correlation Spearman Correlation Symptom Pain Fatigue Sadness Worry Sleep Problems -0.51 -0.20 -0.36 -0.37 -0.57 -0.71 -0.71 -0.57 -0.45 -0.76 Differences in child report by age • Teens report higher prevalence on all (comparable) symptoms assessed Symptom Prevalence (%) 60.00 50.00 40.00 30.00 7-12 yo 20.00 13 yo and up 10.00 0.00 8 MSAS Symptoms Differences in child report by age • Teens report higher scores (>distress) on all (comparable) symptoms assessed* 30 MSAS Symptom Score 25 20 15 7-12 yo 10 13 yo and up 5 0 *scales would favor higher scores among younger children 8 MSAS Symptoms 3. Effects of feeding back children’s reports to clinicians and parents in children with advanced cancer: Results of the PediQUEST Randomized Controlled Trial Satisfaction with Feedback Satisfaction with Feedback Intervention Effect • Main Outcomes: – MSAS total scores and subscores – PedsQL total scores and subscores • Covariates: – Time in study • Analysis strategy: – Multivariate linear mixed effects models (to account for having repeated measures on the same subjects, i.e. observations that are correlated). Strengths and Limitations Strengths • Prospective – longitudinal PRO data Limitations • Validity of tool scores/measurement tools • Selection bias (relatively healthy cohort) PediQUEST Conclusions • Child-reported outcomes are feasible • RCT supportive care trial is feasible in children with advanced cancer • Children with advanced cancer experience many distressing symptoms • Feedback alone has some effect on child suffering but can be strengthened Question Why was feedback alone insufficient to significantly improve symptom distress and quality of life outcomes? Possible Explanations • PediQUEST feedback had a limited effect in activating physicians to attend to symptom distress, as suggested by satisfaction results • Physician attitudes/beliefs may play a strong role in symptom assessment and management Next Steps Next Steps – PediQUEST Champion Intervention • Hypothesis: compared to an enhanced feedback system alone, combining feedback with intensive follow-up by an pediatric nurse practitioner champion will more effectively reduce child symptom distress. • Rationale: embedding symptom management support within oncology will – – provide more targeted and timely telephone and/or face-to-face response to a child’s distress experience. Web platform PediQUEST: A Peppercorn Collaboration DFCI/CHB Team Veronica Dussel, MD,MPH, Christina Ullrich, MD, MPH, Bridget Neville, MPH, Kun Chen PhD, Liliana Orellana PhD CHOP Team Karen Carroll, Tammy Kang MD, Chris Feudtner MD PhD MPH Seattle Team Abby Rosenberg, MD, Karina Schmidt, Russ Geyer MD MPH, DFHCC Collaborators Fran Cook ScD, Jane Weeks MD MSc Collaborating Services DFCI Research Information Services Communication Core DFHCC Thank you!