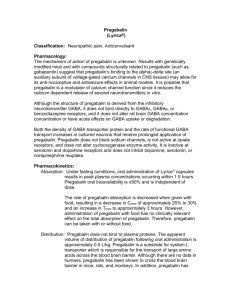
Clinical Trials of Pregabalin in Patients with Neuropathic Pain
advertisement

Analgesic clinical trials and their assay sensitivity Robert H. Dworkin, PhD Professor of Anesthesiology, Neurology, Oncology, and Psychiatry Professor, Center for Human Experimental Therapeutics University of Rochester School of Medicine and Dentistry Outline 1. Limitations of existing pain treatments 2. Negative trials and some possible explanations 3. An evidence-based approach to analgesic clinical trial design 4. Study-level analyses 5. Subject-level analyses 6. Novel clinical trial designs Limitations of existing pharmacologic treatments for pain • A substantial percentage of patients either fail to obtain satisfactory relief or cannot tolerate the side effects of treatment. • In patients who do improve, there is typically partial relief of pain, not complete relief. • In patients whose pain is relieved, there are often limited improvements in functioning and sleep. • Side effects of many pharmacologic treatments are a burden to patients. 20 recent negative neuropathic pain trials (and there are many others1) Gabapentin enacarbil in painful DPN Gabapentin extended-release in PHN Lacosamide in painful DPN (2 trials) Andinitpainful would be(2very Lamotrigine DPN trials)easy to do a Lamotrigine in mixed neuropathic pain conditions similar list for clinical trials of Levetiracetam in PHN Oxcarbazepine in painful DPN (2 trials) Oxcarbazepinechronic in lumbosacral radiculopathy low back pain, Pregabalin in painful DPN (3 trials) Pregabalin in painful HIV neuropathyetc. osteoarthritis, Pregabalin in lumbosacral radiculopathy Propentofylline in PHN Topiramate in painful DPN (3 trials) 1see Finnerup NB, et al. Pain 2010;150:573-581. Unfortunately, we often do not know which of these results are true negatives (i.e., examples of “drug failure”) • some of these drugs may not be efficacious in the specific pain conditions in which they were studied and which results are false negatives (i.e., examples of “study failure”) • some of these may be failed studies of truly efficacious drugs Treatment Trial results Positive Negative Efficacious Not efficacious True positive False positive False negative True negative 20 recent negative neuropathic pain trials (and there are many others1) Gabapentin enacarbil in painful DPN Gabapentin extended-release in PHN Lacosamide in painful DPN (2 trials) Lamotrigine in painful DPN (2 trials) Lamotrigine in mixed neuropathic pain conditions Levetiracetam in PHN Oxcarbazepine in painful DPN (2 trials) Oxcarbazepine in lumbosacral radiculopathy Pregabalin in painful DPN (3 trials) Pregabalin in painful HIV neuropathy Pregabalin in lumbosacral radiculopathy Propentofylline in PHN Topiramate in painful DPN (3 trials) 1see Finnerup NB, et al. Pain 2010;150:573-581. Why have so many recent analgesic trials been negative? 1. Preclinical animal models and methods are identifying some drugs that have limited or no efficacy. 2. Early proof-of-concept (i.e., Phase 2) trials are identifying some drugs or dosages that have limited or no efficacy. 3. Many of these recent results are actually false negatives. • ~ 50% of depression trials fail... 4. Placebo group patients improved “too much.” 5. The optimal pain conditions or pain patients were not studied. 6. Temporal changes in characteristics of patients enrolling in trials and in types of sites conducting trials. An evidence-based approach to analgesic clinical trial design 1. Investigate relationships between the methodologic features of clinical trials and their “assay sensitivity” (i.e., their ability to distinguish efficacious treatments from placebo or less efficacious treatments) • e.g., are certain patient, study design, or study site characteristics associated with greater assay sensitivity? 2. Determine whether assay sensitivity can be increased by modifying these patient or study features • e.g., possibly by efforts to reduce placebo group improvement Patient factors Study design factors Study site factors • Minimum pain duration • Maximum pain duration • Baseline diary compliance • Minimum mean baseline pain intensity • Maximum mean baseline pain intensity • Baseline pain variability • Baseline pain consistency • History of treatment failure(s) • Sources of patient referrals • History of psychopathology • Research design (e.g., parallel group vs. cross-over) • Number of treatment arms • Study duration • Study quality • Baseline period duration • Titration period presence and duration • Dosing strategy (e.g., flexible vs. fixed) • Permitted use of rescue and/or concomitant analgesics • Presence of active comparator • Outcome measures • Methods of data collection (e.g., paper vs. electronic) • Sources of patient referrals • Number of sites • Site investigator and staff experience • Site investigator and staff training • Inclusion of patient training • Methods for accelerating enrollment • Geographic region Study-level analyses Some recent findings on placebo group responses in neuropathic pain trials 1. There is greater improvement in placebo groups of negative vs. positive neuropathic pain trials. • Katz J, Finnerup NB, Dworkin RH. Clinical trial outcome in neuropathic pain: relationship to study characteristics. Neurology 2008;70:263-272. 2. There is greater placebo group improvement in longer vs. shorter painful DPN trials. • Quessy SN, Rowbotham MC. Placebo response in neuropathic pain trials. Pain 2008;138:479-483. 3. Placebo group improvement—but not active treatment group improvement—is significantly less in PHN compared with painful DPN trials. • Dworkin RH, Turk DC, Peirce-Sandner S, et al. Placebo and treatment group responses in postherpetic neuralgia vs. painful diabetic peripheral neuropathy clinical trials in the REPORT database. Pain 2010;150:12-16. Subject-level analyses Can baseline pain diaries be used to identify patients who will provide increased assay sensitivity? 1. Minimum pain intensity 2. Maximum pain intensity 3. Variability 4. Consistency 5. Extreme ratings 6. Adherence “Individuals with a greater pain variability index at baseline were more likely to be responders ... to placebo ... suggesting that a high pain variability may be a predictor of a placebo response.” Harris RE, et al. Arthritis Rheum 2005;52:3670-3674. “Because of the larger placebo response for pain-related endpoints … in the high variability patients, the apparent treatment effect size of MLN was smaller in patients with higher pain variability.” Palmer RH, et al. International Conference on Accelerating the Development of Enhanced Pain Treatments, Bermuda, March 2011. “In duloxetine studies for 3 chronic pain conditions (DPNP, CLBP, OA), patients with higher baseline pain variation had a smaller effect size and/or lower treatment response (relative to placebo) compared with patients with lower baseline pain variation. Zhang S, et al. International Conference on Accelerating the Development of Enhanced Pain Treatments, Bermuda, March 2011. Novel clinical trial designs Sequential Parallel Comparison Design (SPCD) Efficacy analysis is based on results of the 8 groups in green boxes Randomize Treatment Phase 1 Results Active Treatment Responder Placebo NonResponder NonResponder Responder Randomize Treatment Phase 2 Active Treatment Active Treatment Active Treatment Active Treatment Placebo Results Res NonRes Res NonRes Res NonRes Res NonRes Res NonRes • The first treatment phase compares the active treatment with placebo, as in a conventional parallel-group design. • In addition, the first treatment phase identifies a group of placebo non-responders. • The second treatment phase compares the active treatment with placebo in the placebo non-responders from the first phase. • The active-treatment vs. placebo difference in the second phase is expected to be at least as large as in the first phase, and larger if placebo non-response in the first phase predicts placebo non-response in the second phase. “There is little doubt that reducing the attrition rate of drug candidates in clinical development represents the greatest challenge and opportunity for pharmaceutical research and development.” Paul SM, et al. Nature Rev Drug Disc 2010;9:203-214. There is little doubt that reducing the attrition rate of analgesic treatments in clinical development represents the greatest challenge and opportunity for the ACTION public-private partnership.