MUR Presentation
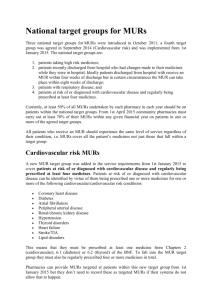
advertisement

Medicines Use Review [MUR] Liz Stafford LPC/PCT liaison Outline Context Understanding potential benefits of MURs Identifying potential barriers & how to overcome them Good practice examples Key Success Factors Context NHS Community Pharmacy contract 2004. - Advanced tier - Requires accreditation of pharmacist & premises Nationally agreed fee funded by budgetary savings as a result of changes to the national medicines reimbursement scheme for community pharmacists. Aimed at helping patients manage their medicines more effectively and should be integrated with GP practice systems and the Primary Care team. Differences Medicines Use Review : Help people use their medicines more effectively Clinical Medication Review: Repeat prescription list & patient interview Mostly technical issues that can be actioned by pharmacist/patient Some patients referred for more detailed clinical review Enable patients to get the most effective & appropriate treatment for them Full medical history and patient interview Mostly clinical MUR A concordance based review to which the patient is asked to bring all their medication (including purchased medicines) : What the patient thinks each medicine is for and how to take it How compliant they are with the prescriber’s instructions How and when they take medication “prn” or “mdu” Advice on tolerability and perceived side effects Practical issues e.g. ordering, obtaining/taking/using medicines Identification of unwanted medicines; no longer taking it Identification of potential cost savings e.g. dose/ strength optimisation (if no impact on patient’s clinical management plan). Compliance & Concordance (= Time Factor to Understand & Negotiate) Patient related factors - misunderstanding the treatment (or condition) - forgetting - patients’ beliefs - denial - embarassment - lack of social support Treatment related factors - fear, or experience of, side-effects - complex regimen ; frequent dosing; method of administration Condition related factors - no, or mild, symptoms ; sever symptoms What an MUR is not ! A full clinical review An agreement about changes to medication A discussion about the medical condition beyond that which is needed to obtain the MUR objectives A discussion on the effectiveness of treatment based on test results. Facts Around 50% of patients do not comply with some element of prescribed treatment; a large proportion of GP appointments are taken by patients with long term conditions; and a high proportion of hospital readmissions in the elderly are a direct result of poor compliance with prescribed medication. Potential benefits Patients : - improved health outcomes & quality of life - encourages self care ; ownership of condition & treatment GPs, Commissioners, Primary Care team: - reduction in secondary care admissions - cost savings from prescribing budget i.e. waste, efficiencies. - can save time and can improve quality of QOF reviews and clinical reviews if MUR is done first. - opportunity to integrate care pathways as part of service redesign - opportunity to support “long term conditions” closer to home Potential Barriers New service for community pharmacists, GPs and patients - not well communicated, nor understood, nor designed. Confusion about level of review and purpose. Increase in GPs’ workload in many cases. Not meaningful nor useful to GPs if not integrated as part of practice systems. Format not user friendly ; cannot be easily entered on practice I.T. systems (- will change and be electronic) Potential Barriers Although part of the community pharmacy contract since 2004, it was underestimated how long it would take for community pharmacists to be able to deliver the service : - development of new patient facilities/ consultation rooms pharmacist accreditation with HEI pharmacist workload / delivery of new contract development of support staff re-engineering of community pharmacy practice. confidence communications From barriers to benefits Pharmacists - discuss with GPs patient selection e.g. respiratory patients, elderly on more than 4 items or those that the practice does not usually see ? Some MURs will be opportunistic. Agree local arrangements for sending MURs to GP practice : to whom & how e.g. “no action” forms in a bundle monthly; what about those needing attention? Summary form ? Practices - identify patients (coloured dot on script?); integrate MURs e.g attach to patient notes before QOF or clinical review. GPs - review MURs with pharmacists – give feedback MURs – going forward Increase patient awareness with support from GPs, PCT team - terminology “ Medicines Check Up” Referrals - Prior to annual medical reviews - From “fallers” units in hospitals - Via community matrons, district nurses, social services, etc. - For care home and housebound patients Share good practice and benefits Some typical MUR outcomes Ormskirk – patient with frequent scripts for salbutamol was invited for MUR.Poor control of asthma (according to indicators) When MUR was sent to GP practice it was discovered that the patient was not flagged as an asthmatic. Patient taking lorazepam routinely at night did not know why. He had been prescribed it “prn” in hospital and when he came out it continued to be prescribed, so he just took it every night. Patient using Avesco (steroid) inhaler was using it ad.hoc. not as prescribed Patient using steroid inhaler had oral thrush. He was referred to get treatment and advised to rinse mouth after each inhalation During checking of inhaler technique it was found that one patient was double dosing by activating two puffs instead of one Key learnings Average time spent face to face with a patient was 15.2 minutes. Total average time on recruitment, preparation, form filling, patient contact and follow up was 45 minutes Over 40% of patients were receiving medicines from 2 BNF categories 30% were receiving medicines from 3 or more BNF categories 70% of customers were over 55 years old 45% male, 55% female 87% thought that pharmacists should offer such a service 95% of customers were satisfied with the service Integrated Service –examples As agreed with one GP practice, stable hypertensives (normally seen annually) are sent for a MUR at 6 months when they have their B.P. taken by the pharmacy (commissioned via PBC). This enables GPs to gain QOF payment. In Poole PCT, MUR is the starting point to involve community pharmacists in a new care pathway for COPD. The next level of service involves providing the pharmacist with more information from the GP practice so they can assess symptom control, provide specific health promotion & referrals. Integrated Service – example Patients may be selected for the repeat dispensing service, for example, after their annual medical review e.g for 6 months or 12 months, etc. - Pharmacist carries out MUR just before referring patient back to the GP for their next annual review, so that GP has MUR information at this point. - Pharmacist could also remind patient when blood tests, etc. are required (if GP attaches this information to RD request) Estimated that 80% of repeat prescriptions could be handled by community pharmacy. Key Success Factors The WILL to make it happen and realise the benefits! Excellent local communication between community pharmacists, GPs, practice managers, nurses, community matrons, PCT personnel and patients /patient groups. Mutual understanding of protocols, parameters & preferred target patient groups. Repeat dispensing will help to align the process.