Migraine headaches
advertisement
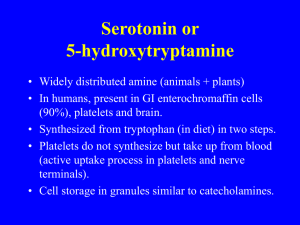
Vishal Sharma MIGRAINE HEADACHES Overview Migraine and Statistics History Classification and symptoms Etiology and Pathophysiology Treatment Migraine and statistics Migraine is a neurovascular disease caused by neurogenic inflammation and characterized by severe, recurring headaches It usually characterized by the severe pain on one side of the head as compare to the pain in rest of the head. It occurs more often in Women than in men. History History goes back to 9000 years. First mode of treatment: trepanation Medical intervention in which a hole is drilled or scraped into the human skull, exposing the dura mater in order to treat health problems related to intracranial diseases. History cont. In 2nd century AD, Pergamum a Greek physician used a term hemicrania. The brain and stomach were connected “Migraine” evolved from this term However, this idea was replaced by blood flow in 17th century In 80s, Dr. Harold G. Wolff said that dilation of blood vessels is the main cause of migraine. Classification of Migraine headache. 1) Migraine without Aura or common migraine Does not give any warning signs before the onset of headache. It occurs in about 70 to 80% of migraine patients 2) Migraine with Aura Give some warning signs “ called aura” before the actual headache begins. Approximate, 20 to 30% migraine sufferers experience aura. The most common aura is visual and may include both positive and negative (visual field defects) features. Zigzag structure Negative scotoma. Loss of local awareness of local structure Positive Scotoma. Additional structures One side loss of perception. Classification of Migraine headache cont. 3) Retinal migraine It involves attacks of monocular scotoma or even blindness of one eye for less than an hour and associated with headache. 4) Childhood periodic syndromes that involve cyclical vomiting (occasional intense periods of vomiting), abdominal migraine (abdominal pain, usually accompanied by nausea), and benign paroxysmal vertigo of childhood (occasional attacks of vertigo). They may be precursors or associated with migraine. Classification of Migraine headache cont. 5) Complications of migraine describe migraine headaches and/or auras that are unusually long or unusually frequent, or associated with a seizure or brain lesion. Etiology and Pathophysiology The precise etiology and pathophysiology of migraine is unknown. However, neuronal dysfunction theory is most acknowledged theory. Activity in trigeminovascular system. Abnormal Neuronal activity Cerebral cortex, thalamus or hypothalamus in response to stress, emotion. ‡ Activates nociceptive trigeminovascular system and causes prolong pain Instability in release of neuropeptides e.g., Substance P, neurokinin A, calcitonin gene-related polypeptide, serotonin Promote vasodilation and plasma protein extravasations. Initiate inflammatory response, sensitizes surrounding tissues and produce headache Activates trigeminovascular system, which in turn, stimulate pain stimulating neurons in brain stem and upper spinal cord Abnormal Neuronal activity Cerebral cortex, thalamus or hypothalamus in response to stress, emotion. ‡ Releases vasoactive neuropeptides e.g., Substance P, neurokinin A, calcitonin gene-related polypeptide, serotonin Promote vasodilation and plasma protein extravasations. Boss Initiate inflammatory response, sensitizes surrounding tissues and produce prolong headache Activates nociceptive trigeminovascular system and causes prolong pain Activates trigeminovascular system, which in turn, stimulate pain stimulating neurons in brain stem and upper spinal cord Serotonin Neurotransmittor Serotonin ( 5- hydroxytryptamine) is thought to be an important mediator of migraine. Unstable serotonergic neurotransmission , so has lower threshold for migraine. There are 7 classes of 5-HT receptors Out of 7, 2 involve in migraine pain. Serotonin cont. It is basic as amines and Ammonia Changes Ph of blood Serotonin causes Vasodilation Serotonin causes Vasoconstriction During migraine the level of serotonin is low in blood. (Low Ph) Drug target 5- HT1 Presynaptic receptor Serotonin binds to 5-HT1 and 5-HT2 5- HT2 Postsynaptic receptor How bad could migraine be… It could distrub the normal life activities. Could lead to brain damage Recently, a woman in London had a migraine Lost her accent Treatment Identification and elimination of factors. For example, Tobacco smoke, loud noise, stress, caffeine, emotions, contrasty light etc. If they don’t work then move on to medicines 1) Prophylactic therapy 2) Abortive therapy Prophylactic therapy Used in case of frequent migraines Used when abortive therapy has failed Medicines have to taken everyday to be effective On the other hand, abortive medicine are taken during actual migraine pain. Medicines used in this therapy 1) Medicines that block beta-adrenergic. For example, Propranolol, nadodol, timolol, atenolol, and metoprolol. Reduce the frequency of attacks by 50% in 60 to 80% patients. Side effects- fatugue, sleep disturbance, depression, hypotension etc Cont. 2) Tricyclic antidepressants For example, amitryptiline, nortryptiline, doxepin, imipramine etc Independent of antidepressant activity. Antagonist of 5-HT2, thus stabelize serotonin neurotransmission 3) Methysergide:Semisynthetic ergot alkaloid and is 5-HT2 antagonist. Gives best result when taken with meals Side effects- gastrointestinal intolerence, insomnia, and muscle cramps. Prophylactic therapy cont. Calcium channel Blockers Verapmil Takes up to 8 weeks to show any good effect Side effects- Hypotension, constipation etc Abortive therapy 1) simple analgesics:- For mild and infrequent migraine- Aspirin and acetaminophen Aspirin+acetaminophen+barbiturate butabital = To induce sleep aspirin+acetaminophen+narcotics = Fiorinal Aspirin+ acetaminophen+caffiene = Esgic Drawback- Continuous use fails to provide pain relief. Abortive Therapy cont. 2) NSAIDs: Inhibit prostaglandin synthesis. So may prevent inflammation in trigeminovascular system and alleviate migraine pain They are effective for reducing the frequency, severity, and duration of migraine attacks. e,g. Aspirin, Ibuprofen, Naproxen etc. Corticosteroids mediate glucose metabolism and inflammation Inflammation, Asthma Plasma Membrane phospholipids Arachidonic Acid (AA) Annexin Prostaglandins, leukotrienes Aspirin Phospholipase A2 Steroidal (corticosteroid) Anti-inflammatory Cyclooxygenase (COX) Non-steroidal Anti-inflammatory Abortive therapy cont. 3) Ergot family ErgotamineIt is secondary metabolite obtained from ergot fungus Dihydroergotamine- available in inject able form. The structure shares some similarit with neurotransmittor serotonin. Acts as agonist, bind to 5-HT1, More effective when given during early migraine attacks Abortive therapy 5) Triptan Family 5-HT1 receptor agonists Examples- Sumatriptan – Imitrex Zolmitriptan – Zomig Rizatriptan – Maxalt Eletriptan – Relpax Naratriptan - Amerge Elitriptan Sumatriptan Rizatriptan Zolmitriptan Side Effects nausea, vomiting, dizziness, fatigue, and vertigo. Not good for hypertensive patients at all. Ergot and Triptan comparison The rates of ergotamine and sumatriptan overuse were 14.2% and 3.5%, respectively Drug-induced headache could be found more frequently in cases of ergotamine overuse then drugs of triptan family. Miscellaneous agent Midrin = Isometheptane+ dichlorophenazene+ acetaminophen Used in patients who do not respond to ergot and triptan Less effective then ergot and triptan family’s drugs Most frequent side effects are nausea, dizziness, insomnia, and vomiting. References "Etymology of migraine". Online Etymological Dictionary. http://www.etymonline.com/index.php?term=migraine. Retrieved 27 May 2009 http://en.wikipedia.org/wiki/Migraine Headache Classification Subcommittee of the International Headache Society (2004). "The International Classification of Headache Disorders: 2nd edition". Cephalalgia 24 Suppl 1: 9–160. doi:10.1111/j.1468-2982.2004.00653.x. PMID 14979299. Questions Name the major neurotransmitter that mediate the migraine pain. Name major medicines that act as 5-HT1 agonist and 5-HT antagonist. How does NSAIDs work?