Crying babies
Katie Lazenby
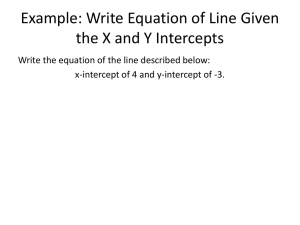
Introduction
• Normal attachment behaviour
• Peaks 6-8 wks – 2.6 hrs crying/day
• Problematic in 20% babies “colic” - >3hrs/day,
3 days/wk, >3 wks.
• 5% organic cause
• Many caused by inability to self-soothe
History
• Parents’ views, experience, support
• Crying patterns
• Other Sx – blocked nose, vomiting,
constipation, diarrhoea, eczema
• Sleeping & feeding patterns
• Family stress, maternal depression
Examination
• Head to toe, explaining to parents
• Exclude potential cause discomfort eg. Nappy
rash/eczema
• Orifices – phimosis, anal fissure, oral thrush,
otitis media
• Plot weight growth chart
Causes
• Medical
– GORD
– Lactose intolerance
– Cow/soya milk protein allergy
• Non-medical
– Tired
– Hungry
– Will not settle
– Family psychosocial difficulties
GORD
• Increased prevalance preterm, GI obstruction,
neurological problems eg. CP
• Features – frequent vomiting shortly after feed,
difficulty feeding, crying, failure to thrive, apnoeic
episodes, wheeze/cough.
• Mx
–
–
–
–
Upright posture post feed, tilt cot, avoid overfeeding
Food thickener
Infant Gaviscon
Hospital Rx – domperidone, ranitidine, omeprazole
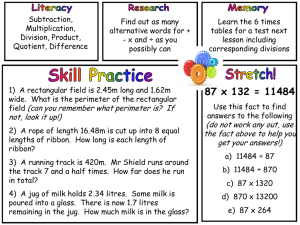
Lactose intolerance
• Controversial theory
• Low lactase levels – lactose build up - lactic
acid
• 1 wk trial lactase drops (Colief – can buy or Rx
ACBS)
• Use behaviour diary to monitor effect, if
response continue to 3-6 months.
• Low lactose feed not recommended
Cow/soya milk allergy
• 50% crossover with soya
• Vomiting, diarrhoea (blood/mucus), poor
weight gain, atopy, FHx.
• Trial diet modification
– Breastfed – mother avoid all dairy, caesin & whey.
Use soya milk, take calcium supplement
– Bottlefed – hydrolysed cow’s milk/soya milk
(Nutramigen 1, Pregestimil, Pepti-junior)
– 1 wk trial, behaviour diary
Tired baby
• Average sleep
– Newborn - 16 hrs
– 2-3 months – 14 hrs
• Time before tiring
– 6 wks – 1.5 hrs
– 3 months – 2 hrs
• Signs tiredness – frowning, clenching fists,
jerking limbs
• Sleep hygiene – consistent place, soothe
without picking up, background white noise.
Hungry baby
• Frequet feeding, not settling post feed, poor
weight gain
• Mother may c/o poor milk supply –
HV/breastfeeding counsellor advice
• Top ups with formula in evening
Will not settle
• ?delayed neuromaturation – reduced ability to
self soothe
• Distractions
– Carry in sling
– Minimise separation
– Walk in pram/push over uneven surface
– Warm bath
– White noise
Psychosocial problems
• Factors affecting baby’s behaviour/parent’s
response to crying:
– Infant-parent relationship
– social and cultural beliefs of family
– problems in pregnancy
– Post natal depression (can aso be triggered by
irritable baby)
Management
•
•
•
•
•
•
•
•
Exclude medical cause
Reassurance
Explain normal crying and sleeping patterns
Behaviour diary
Follow up and ongoing support
Websites/helplines
HV
Assess for post natal depression
Websites
• CRY-SIS
– Charity running telephone helpline and offering
useful checklist
– www.cry-sis.org.uk
• Parentline
– www.parentlineplus.org.uk
• Home-Start UK
– Volunteers providing home visiting scheme
– www.home-start.org.uk
Medication
• Anticholinergics effective but not suitable due
to S/Es.
• Simethicone (Infacol) licensed for colic but no
benefit over placebo in trials. 1 wk trial may
be helpful.
• Trials of diet modification - cow’s milk
exclusion/lactase drops.
When to refer
• Paediatrics:
– Parents not coping despite intervention
– Suspected medical cause / uncertain diagnosis
– Unable to wean off treatment after 6 months
• Perinatal mental health service if concerns re
severe postnatal depression
AKT question
A 3-month-old baby girl is brought to see you
by her mother. She reports a 1 month constant
crying, which is worse at night. She is bottlefed and is feeding well. There is no
vomiting. Her weight has remained steady on
the 25th centile since birth. On examination,
she has a well-circumscribed discoid red lesion
approximately 8 mm diameter on the top of
her thigh. There is an identical lesion on her
lower back.
• Which is the SINGLE MOST appropriate initial
management option for this patient? Select
ONE option only.
• A. Advice and reassurance
B. Refer to community paediatrician
C. Refer to dermatologist
D. Refer to health visitor
E. Refer to social services
Answer E.
This describes a case of non-accidental injury
(NAI)—the discoid red lesions representing old
cigarette burns. This would require an
immediate referral to social services. This
highlights the importance of considering the
family and social situation when faced with a
crying baby.