Powerpoint Presentation - California State Association of
advertisement
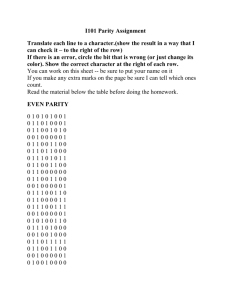
Parity 101: What does it Mean for Behavioral Health Services? Sandra Naylor Goodwin, PhD, MSW California Institute for Mental Health June 2, 2011 Prevalence • 1 in 5 CA adults experiences a mental disorder; 1 in 25 symptoms of a serious mental illness • 1 in 10 CA adults abuses or is dependent on alcohol or drugs • 9-13% of CA children and youth between ages 9-17 have a serious emotional disturbance (SED) accompanied by a substantial functional impairment Faces of Medicaid III: Refining the Portrait of People with Multiple Chronic Conditions • Fewer than 5% of beneficiaries account for more than 50% of overall Medicaid costs • 49% of Medicaid beneficiaries w disabilities have a psychiatric illness • 36% of Medicaid beneficiaries who are seniors have a psychiatric illness – October 2009 Center for Healthcare Strategies Faces of Medicaid III (cont) • 75% of Medicaid costs = 3 or more chronic conditions • Psychiatric illness is represented in 3 of the top 5 most prevalent pairs of diseases among the highest-cost 5% of Medicaid-only beneficiaries with disabilities Faces of Medicaid III Basics of Parity • Mental health and substance use benefits in health insurance have historically been less generous than other physical illnesses. • Parity is a response to this disparity, refers to the concept that MH & SU coverage is to be offered on par with covered medical and surgical benefits. Federal Parity Law • Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) Public Law 110-343 – Law: Mental Health and Substance Use Services must be provided at parity with general healthcare services • no discrimination – No mandate to cover MH or SU – However, if any MH or SU benefit is provided, all must be provided at parity 7 Requirements/Limitations • Financial requirements – e.g., deductibles, copayments, coinsurance, out-of-pocket maximums • Treatment limitations – limit benefits based on frequency of treatment, number of visits, days of coverage, days in a waiting period, and “other similar limits on the scope and duration of treatment”. – Quantitative treatment limitation – expressed numerically, e.g., annual limit of 50 outpatient visits – Non-quantitative treatment limitation – not expressed numerically but otherwise limits the scope or duration of benefits Requirements/Limitations • All comparisons of benefits must be within the six categories: – Inpatient, in-network – Inpatient, out-of-network – Outpatient, in-network – Outpatient out-of-network – Emergency care – Prescription drugs Federal Parity Law • Interim Final Regs issued February 2, 2010 (75 Fed. Reg. 5410) – Applies to group health plans for plan years beginning on or after July 1, 2010 – Does not apply to plans insuring small businesses (less than 50) – Medi-Cal: applies to Managed Health Care, PrePaid Inpatient Health Plans, CHIP (Healthy Families) • Regulations governing the rest of Medi-Cal to be out this year Patient Protection & Affordable Care Act Healthcare & Ed Reconciliation Act • Expands the reach of the applicability of federal parity law in 2014 – To qualified health plans established by PPACA – Medicaid non-managed care benchmark and benchmark equivalent plans – Plans offered thru the individual market • Creates a mandate to provide certain MH & SU services – To be created thru rulemaking California • Benchmark health plans – CA Health Insurance Exchange Board must define scope of MH & SU benefits within federal guidelines and parity • Indigent Adults without Disabilities or Children: – Must define scope of MH & SU within federal guidelines California • Definition of substance use disorders: – CA must define at what point SU becomes a medical issue that requires treatment and what services will be offered • Mental Health Services: – CA counties provide mental health services thru a Medi-Cal Pre Paid Inpatient Plan – Does this equate to parity for county sponsored Medi-Cal Managed Care? CA 1115 Waiver Conditions Behavioral Health Services Assessment - By March 1, 2012, the State will submit to CMS for approval an assessment that shall include information on available mental health and substance use service delivery infrastructure, information system infrastructure/capacity, provider capacity, utilization patterns and requirements (i.e., prior authorization), current levels of behavioral health and physical health integration and other information necessary to determine the current state of behavioral service delivery in California. Behavioral Health Services Plan - By October 1, 2012, the State will submit to CMS for approval a detailed plan, including how the State will coordinate with the Department of Mental Health and Alcohol and Drug Programs outlining the steps and infrastructure necessary to meet requirements of a benchmark plan no later than 2014. 14