Show me the Money - indianamedicaid.com

Show me the Money
Working together to provide quality care for MDwise members
P0607
Indiana Health Coverage Programs
OMPP
FSSA FSSA= Family & Social Services
Administration
OMPP= Office of Medicaid Policy and Planning
Maximus= Enrollment Broker
MAXIMUS
Traditional
Medicaid
HP
590 Program
Care Select
Healthy Indiana Plan
Hoosier Healthwise
Risk-Based Managed Care
MDwise
MDwise
(Care Select)
ADVANTAGE
(Care Select)
Anthem Blue Cross
Blue Shield
Enhanced Services Plan
(ESP)
MHS
P0607
MDwise
MHS
Anthem
2
Managed
Behavioral Health
Organizations
MDwise
Cenpatico
Behavioral Health
Magellan Health
Services
Who is MDwise?
MDwise
is a local, not-for-profit company serving Hoosier Healthwise,
Care Select and Healthy Indiana Plan (HIP) members.
MDwise
believes that everyone deserves to have health coverage.
MDwise
Hoosier Healthwise covers 270,000 children, pregnant women, and eligible families.
P0607 3
Who is MDwise?
P0607 4
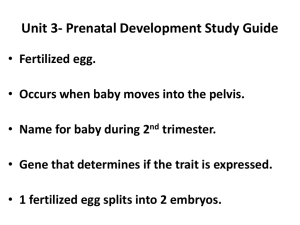
What is Risk-Based Medicaid?
MCE’s are paid a per member per month fee; this is called a capitated rate
The capitated premium covers the cost of the care for all covered services for the patients.
The MCE’s assume financial risk for services of members; thus the name “Risk-
Based” does not mean the patients are “high risk”.
P0607 5
Benefit Package Coverage
Package A – Standard Plan Full coverage for children, low-income families.
Package B – Pregnancy Coverage Only Pregnancy-related, postpartum care, family planning, pharmacy, transportation, urgent care services for some pregnant women.
Package C – Children’s Health Plan Preventive, primary, and acute care services for some children under 19 years old.
Package P – Presumptive Eligibility Presumptive eligibility for pregnant women.
(RID # starts with 550)
Package E – Emergency Only Limited to treatment for medical emergency conditions.
P0607 6
NCQA
National Committee for Quality Assurance is the organization that accredits Managed Care
Organizations (MCO’s).
Mission
To improve the quality of health care.
Vision
To transform health care quality through measurement, transparency and accountability.
Values
Our passion is improving the quality of health care.
We stand for accountability throughout the health care system.
7 P0607
NCQA
created
HEDIS
H
ealthcare
E
ffectiveness
D
ata &
I
nformation
S
et
A set of standardized performance measures
• Ensures that consumers have reliable information on the performance of
MCO’s.
• >90% of health plans use HEDIS to measure performance on important dimensions of care and service.
8 P0607
P
ay for
P
erformance or
P4P
are Incentivized
HEDIS Measures
A contractual activity of MCO’s
P4P is an incentive to meet quality measures for providers in the commercial, Medicaid and Medicare insured populations.
1.0% of the MDwise capitated payment is withheld, and paid to the MCO when quality goals are met.
P0607 9
Pay for Performance – P4P
• Supplemental payment based on measured performance against a target
• Incent high quality care by shifting greatest reimbursement to highest quality providers and plans
• Incent provider offices to increase visits or improve processes.
• Site contests or office contests to improve quality of care.
P0607 10
Pay for Performance – P4P
• Provider incentives based on claims submissions.
• Provider incentives based on meeting targeted measures.
• Site contests by increasing a measure or bringing in the most members requiring services in a given measure.
• Provider incentives adding provider staff or equipment that can help increase a quality measure or quality of care to members.
P0607 11
HEDIS contains 71 Quality Measures:
Asthma Medication Use
Persistence of Beta-Blocker Treatment after Heart Attack
Controlling High Blood Pressure
Comprehensive Diabetes Care
Breast Cancer Screening
Antidepressant Medication Management
Childhood and Adolescent Immunization Status
Advising Smokers to Quit & offering assistance to quit ….and others
P0607 12
OMPP Incentivized HEDIS Measures
•
Adolescent well-care
• Well-care for children ages 3-6 years
• Well-care for children, 0 – 15 months
• Timeliness of prenatal care
• Frequency of prenatal care
• Timeliness of postpartum care
• 7 day follow-up of a behavioral health stay
• LDL-C screenings for diabetic members
• Cervical cancer screenings
• Follow – up care for children prescribed ADHD meds
P0607 13
How do we Compare?
Cervical Cancer Screening
LDL-C
(Diabetes Care)
Follow-Up after Hospitalization for
Mental Illness (7 Days)
MDwise NCQA 90 th %tile
74.45%
68.61%
48.22%
79.5%
82.5%
64.2%
14 P0607
How do we Compare?
Timeliness of Prenatal Care
Timeliness of Postpartum Care
Frequency of Prenatal Care
P0607
MDwise
89.54%
75.67%
82.73%
NCQA 90 th %tile
92.2%
72.7%
81.0%
15
How do we Compare?
Six or More Well-Care Visits in the
First 15 Months of Life
Annual Well-Child Visit Ages 3-6
Annual Well-Child Visit Adolescents
MDwise
60.83%
72.99%
53.28%
P0607 16
NCQA 90 th %tile
73.9%
80.3%
56.7%
How we Promote Quality Care
Provider and staff education
Network Improvement Program (NIP) Team
Billing and process audits
ManagedCare.com
Member education
Reminder Calls about appointments to members
Member incentives:
Well Child (3 – 6 and 12 – 21)
Provider incentives
Disease/Health management services for members with diabetes
Disease/Health management for members with asthma
17 P0607
How NIPT Can Help…..
The Network Improvement Programs Team assists MDwise departments in the outreach and education of its providers and delivery systems.
NIP Team Responsibilities:
Created to take improvement efforts to a higher level
Educating providers on HEDIS and ROQ standards.
Providing physicians information about their quality performance
Diagnose office practices that may result in missed opportunities to provide care or cause services to not be billed correctly
Creating and distributing reference/educational materials and tools
P0607 18
NIP Reports
Measure
W34
AWC
Eligible
Members
2,996
Current
Numerator
Current %
Meets
90th
Percentile
1,380 46.1% 79%
Vol. Mbrs.
Missed Opp.
Potential %
Meets
Vol. Needed for 90th
1254 87.9% 987
% of Opportunity
Needed
79%
3,239 747 23.1% 57% 1308 63.4% 1099 84%
Note: Data is based on dates of service 1/1/09-12/31/09 with claims paid through 11/30/09 captured.
P0607 19
Measure
Cervical Cancer Screening
LDL-C Screening
F/U Care for Children Prescribed ADHD Meds
Initial Phase
Follow-up After Hospitalization for Mental Il
Follow-up Within 7 Days of Discharge
Timeliness of Prenatal Care
Timeliness of Postpartum Care
Frequency of Prenatal Care >81%
Well-Child Visits in First 15 Mths of Life
Six or More Visits
Well-Child Visits - Ages 3-6
Adolescent Well-Care Visits
Measure
Cervical Cancer Screening
LDL-C Screening
F/U Care for Children Prescribed ADHD Meds
Initial Phase
Follow-up After Hospitalization for Mental Il
Follow-up Within 7 Days of Discharge
Timeliness of Prenatal Care
Timeliness of Postpartum Care
Frequency of Prenatal Care >81%
Well-Child Visits in First 15 Mths of Life
Six or More Visits
Well-Child Visits - Ages 3-6
Adolescent Well-Care Visits
NIP Reports
DS Practice Doc1
Denom inator
0
Meet
Criteria
0
% Meet
Criteria
100.0%
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
#DIV/0!
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
Doc2 Doc3 Doc4
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
0 0 100.0% 0 0 #DIV/0!
0 0 0% 0 0 0% 0 0 0% 0 0 0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
#DIV/0!
#DIV/0!
#DIV/0!
#DIV/0!
#DIV/0!
#DIV/0!
#DIV/0!
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0 0 100.0%
DS
Denom inator
0
Meet
Criteria
0
% Meet
Criteria
100.0%
Meet
Criteria
0 0
Practice
Denom inator
#DIV/0!
% Meet
Criteria
0 0 0%
Doc5
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
0 0 0% 0 0 0% 0 0 0%
Doc6 Doc7 Doc8
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
Meet
Criteria
0
Denom inator
0
% Meet
Criteria
0%
0
0
0
0
0
0
0
0
0
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
100.0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0%
0%
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0%
0%
0%
0%
0%
0%
0%
0%
0%
20 P0607
NIP Reports
120%
100%
OMPP Target
80%
DS Totals
60%
Practice Totals
40%
20%
0%
CCS CDC ADD FUH PPC PPC FPC W15 W34 AWC
P0607 21
Disease/Health Management
RN’s identify & evaluate members with unique healthcare needs
Develop individualized plan of care
Assist in overcoming barriers to care
Risk assessment
Maintains contact with PMP and member
Implements interventions for identified needs.
P0607 22
Disease Management Goals
• Empower member with self-management tools, education and awareness
• Promote the Asthma/Diabetes action plan in the home, school, and provider office
• Encourage adherence to the physician’s treatment plan
• Reinforce self-management goals: problem-solving techniques, overcoming barriers, and establishing goals
• Provide physicians with member specific utilization information including pharmacy, emergency room, and outpatient visits
• Promote relationship between the member and his/her physician(s)
• Promote healthy lifestyle choices
P0607 23
Opportunities for Improvement
• Maximize every member interaction to provide preventive and well-care.
• Well care visits for children when they are in for acute care
• Schedule the 15 th month EPSDT (Early Periodic Screening, Diagnosis, and Treatment) visit prior to the 15 th month of life
• LDL-C screens for diabetics when in for acute care
• Document all components of prenatal and postpartum care and submit for well-care visits.
• Staff who does scheduling can identify members who need services to schedule in a timely fashion
• Ensure proper billing for services rendered.
• Be sure that the documentation is complete
24 P0607
Converting Acute Visits to Well Visits
P0607 25
P0607 26
Documentation for Well Child Visits
Developmental milestones
Review diet and nutrition
Previous problems addressed?
Address obesity and other chronic problems
Ask about smoking, starting at age 10 yrs.
Mental and physical assessment
BMI – record & discuss
Unclothed exam
Provide anticipatory guidance & counseling
Do routine testing (lead, vision, hearing)
P0607 27
HealthWatch/EPSDT/Bright Futures
Preventive healthcare program
Emphasis is given to early detection
For members from birth to 21 years old
Required care for Medicaid members
Assures availability and accessibility of required health care resources
These components of care are a required part of the well-child assessment
P0607 28
Opportunities
If a member contacts the primary medical provider’s (PMP’s) office for a sore throat (sick visit) the office should take the opportunity to provide preventive care and schedule a well child visit if the member is due for services.
If the PMP office receives a list of non – compliant members, the office should reach out to the members and schedule preventive services.
P0607 29
Opportunities
A PMP office could take the opportunity to convert a sick visit into a well
– child visit when the member is in the office for acute care.
If the PMP office has electronic medical records (EMR), implement alerts to reflect the non – complaint members in the quality measures.
P0607 30
Opportunities
If a member is being seen for an initial prenatal visit or post partum visit, all the components of a preventive well – child exam are provided. The appropriate V20.2 or V70.0 can be submitted as a secondary diagnosis code and count towards the AWC measure.
If all components of Early and Periodic Screening, Diagnosis, and Treatment
(EPSDT) services were provided, remember to submit the appropriate
99381 – 99385 or 99391 – 99395 with the V20.2.
P0607 31
Opportunities
If all components of EPSDT were not provided, remember to submit the appropriate E&M code along with V20.2, V70.0, or V70.3 to ensure the services count towards the HEDIS measure.
If EPSDT services were provided along with acute care, be sure to submit the appropriate EPSDT code along with the E&M code and the 25 modifier to ensure the services are counted towards the HEDIS measure.
P0607 32
Quiz……..
1.
If the PMP office provides immunizations and well care at the same visit, can I bill for both?
2.
How do I bill for both services and how do they count towards the
HEDIS measure?
3.
When can I bill for the following combination 99381 and V20.2 as primary?
4.
If a pregnant adolescent member is seen for prenatal care, how is the claim coded to count towards the HEDIS measure?
5.
Can a sick visit and a preventive visit be billed and reimbursed n the same date of service (DOS)?
33 P0607
Quiz……..
1.
Is MDwise currently at the NCQA 90 th percentile for the well – child 3
– 6 measure?
2.
Name 2 examples of provider incentives?
3.
Name 2 examples to promote quality of care within the MDwise network.
4.
Give an example of a disease management goal?
5.
Give an example for an opportunity for improvement?
6.
What is a goal of the EPSDT program?
P0607 34
Resources
MDwise website : www.MDwise.org
My Wellness Zone: http://mdws.staywellsolutionsonline.com/
American Academy of Pediatrics http://www.aap.org/
P0607 35
American Academy of Pediatrics
P0607 36
P0607 37
Thanks for your hard work!
Questions?
P0607 38
Handouts
HEDIS poster
Well – Child Mini Poster
Quality PDF
http://www.mdwise.org/about/mdwisequalityprogram09.pdf
EPSDT grid
Network Improvement Program Charts
P0607 39