Management of Alzheimer`s Disease
advertisement
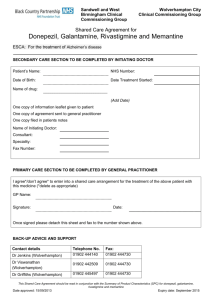
The Management of Alzheimer’s Disease Laurel Coleman, MD Maine Medical Center Portland, Maine Management of Alzheimer’s Disease Manage cognitive symptoms Manage BPSD Support patient/family Increased quality of life for patient and family Pharmacologic Options for AD • Cognitive enhancers ─ 2 classes • Cholinesterase inhibitors (ChEIs) • NMDA-receptor antagonist ─ Do not cure the disease or reverse cognitive impairment ─ Can improve cognition and functional ability ─ Reduce the rate of decline 9-12 months (ChEIs) ─ Delay in nursing home placement was 17-21 months (ChEIs) Management of Alzheimer’s Disease: Cognitive Enhancers *Available in generic Drug Name Dosage form Dosage range Donepezil (Aricept) Tablet*, orally 5 mg – 23 mg QD disintegrating tablet* Minimum Indication titration interval (as tolerated) 4 weeks 5 mg 10 mg 3 months Mild to severe 10 mg 23 mg Galantamine (Razadyne®) Tablet/oral solution* 4 mg – 12 mg BID Extended-release capsule* 8 mg – 24 mg ER QD 4 weeks Rivastigmine (Exelon®) Capsule* 1.5 mg – 6 mg BID 2 weeks Patch Tablet*, oral solution* 4.6 mg – 9.5 mg QD 5 mg – 10 mg QD 4 weeks 1 week Memantine (Namenda®) 4 weeks Aricept® package insert. Razadyne® package insert. Exelon® package insert. Mild to moderate Mild to moderate Mod to severe Pharmacologic Options for AD Common Side Effects NMDA-receptor antagonist Cholinesterase inhibitors (Donepezil, galantamine, rivastigmine) • • • • • • • Nausea Vomiting Diarrhea Weight loss Loss of appetite Muscle weakness Vivid dreams/nightmares (donepezil) (Memantine) • • • • Dizziness Headache Constipation Confusion Aricept® package insert. Razadyne® package insert. Exelon® package insert. Switching ChEIs Lack or loss of therapeutic benefit Immediate switch No washout needed Tolerability issues Washout period of 1-2 weeks before starting another agent Noncompliance Try an alternate dosage form before switching Discontinuation of Therapy • Data for optimal duration of treatment as disease progresses is limited ─ ─ • Consider discontinuation in the following situations: ─ ─ ─ 1. 2. Modest cognitive and functional benefits associated with continued therapy with (donepezil) in moderate to severe AD1 Discontinuation associated with adverse behavioral changes and reduced participation in activites2 Inability to tolerate multiple ChEIs No improvement or greater than expected decline after one or more therapeutic trials End-stage dementia Howard et al. New Engl J Med. 2012;366:893-903. Daiello et al. Am J Geriatr Pharmacother. 2009;7:74-83. Impact of Coexisting Medical Conditions 2.4 conditions/pt HTN 82% DM 39% CAD 21% CHF 14% Stroke 10% Cognitive Impairment Prevalence of coexisting conditions in PWD Schubert CC, et al. J Am Geriatr Soc. 2006;54(1):104–109. Impact of Coexisting Medical Conditions • PWD in primary care average 5.1 medications/pt1 ─ 50% take ≥1 anticholinergic medications • Medications with anticholinergic activity ─ Impairs cognition acutely (delerium) and chronically2 • Anticholinergic burden ─ Interfere with the therapeutic effect of ChEIs3 1. Schubert CC, et al. J Am Geriatr Soc. 2006;54(1):104–109. 2. Campbell N, et al. Clin Interv Aging. 2009;4:225–233. 3. Lu C, Tune LE. Am J Geriatr Psychiatry. 2003;11(4):458–461. Behavioral and Psychological Symptoms of Dementia (BPSD) • • • • Apathy Depressive symptoms Anxiety Agitation/irritability/ aggression • Psychotic symptoms ─ ─ Delusions Hallucinations Tampi et al. Clinical Geriatrics. 2011;19:41-46. • • • • • Disinhibition Euphoria Loss of appetite Sleep disturbances Stereotyped behaviors (eg, pacing, wandering, rummaging, picking Managing BPSD • Identify triggers ─ ─ ─ Observe symptom timing and frequency Look for environmental triggers, eg noise, lighting Investigate potentially treatable causes, eg pain • Make adjustments ─ ─ ─ Address medical causes Adapt environment Adapt caregiving • Modify as needed Managing BPSD Nonpharmacological Interventions • • • • Use the “3 Rs”—repeat, reassure, redirect Simplify the environment, task, routine Anticipate unmet needs Allow adequate rest between stimulating events • Use cues • Encourage physical activity • Other interventions Managing BPSD: Pharmacologic Interventions Drug class Chemical name Dosage range (mg) Side effects of class Antipsychotics Aripiprazole* Haloperidol Risperidone* Quetiapine* Olanzapine* 2.5-15 0.5-5 0.25-2 25-200 2.5-15 Sedation, EPS, NMS, metabolic syndrome, QTc prolongations, increased risk of CVE and mortality Antidepressants Fluoxetine Citalopram Paroxetine Sertraline Trazadone 10-80 10-60 10-50 25-200 25-200 Anxiety, headaches, sedation, GI symptoms, sexual dysfunction Mood stabilizers Carbamazepine Divalproex sodium Oxcarbazepine 100-400 250-1000 300-600 Sedation, gait and balance issues, falls, liver dysfunction, hyperammonemia, thrombocytopenia *2nd-generation antipsychotics Adapted from Tampi et al. Clin Geriatr. 2011;19:31-32. Alzheimer’s Disease Education of Patient and Family Education of Patient and Family • Safety issues: ─ ─ ─ ─ ─ Home environment Driving Medication adherence Financial exploitation Elder abuse • Address future needs: financial planning, advanced directives, power of attorney Education of Patient and Family Medications • Define treatment success ─ Symptomatic benefit in • Cognition • Physical function and ADLs • Behavior ─ Increases time to nursing home placement • Discuss length of therapy ─ Adequate trial is 6 months Cummings JL. Am J Geriatr Psychiatry. 2003;11(2):131–145. Doody RS, et al. Arch Neurol. 2001;58(3):427–433. Impact on Caregivers Tasks Change Over Time Early stage Mid stage • • • Help with IADLS, eg, paying bills and preparing meals Cope with mood swings and reluctance to engage • Help with ADLS, eg, dressing and toileting Cope with increased memory loss, sleep disturbances, wandering, loss of driving Late stage • • Help with all personal care Cope with unresponsiveness and end-of-life issues Education of Patient and Family Alzheimer’s Association • 24/7 Nationwide Helpline ─ ─ • www.alz.org ─ • 800.272.3900 Information and referral in 170 languages Current reliable information for healthcare professionals, people with dementia, family members and caregivers 300 local offices ─ ─ ─ ─ ─ Information and referral Support groups Care consultation Safety services Education, local conferences Clinical Trials • >120 clinical studies in the US are recruiting participants ─ • Slow recruitment is a barrier to discovering new treatments Alzheimer’s Association TrialMatch™ ─ ─ ─ ─ Connect potential participants with appropriate clinical studies Access via phone or online Confidential Free Understanding prevention research • Much evidence comes from large epidemiological studies that show associations, not proof • Study results apply to populations, not individuals • Large randomized studies for many prevention strategies unlikely ─ Cost prohibitive Prevention Factors with a consistent association • • • • • • • Heart-head connection Preventative drug treatments Physical exercise Diet Social connections Intellectual activity Head trauma prevention Prevention Factors with a consistent association Increased risk of AD • Conjugated equine estrogen with progesterone* • Diabetes • Depression • Smoking *Moderate evidence, all other factors had low evidence Decreased risk of AD • Physical activity • Mediterranean diet • Cognitive engagement The Future of Alzheimer’s Disease • Earlier recognition ─ Dependent on reliable biomarkers • New medications ─ Current medications only address symptoms ─ New medications in development • Disease-modifying therapy • Combination disease-modifying and symptomatic therapy • Prevention Alzheimer's Disease Progression Beta-amyloid and neurofibrillary tangle formation begins in pre-clinical phase Pre-Clinical Cell death MCI Probable AD TIME Asymptomatic Aβ=Beta-amyloid AD=Alzheimer’s disease MCI=Mild cognitive impairment Clear cognitive deficits Mild cognitive deficits Adapted from Shaw et al. Nature Reviews Drug Discovery. 2007;6:295-303. Targets for Future Therapies • A ─ -secretase inhibitors ─ -secretase inhibitors ─ Monoclonal antibodies • Tau protein • Inflammation • Insulin resistance Emerging Treatments for AD A production A aggregation A clearance tau aggregation or phosphorylation Cholinergic drugs Other Clinical Trials Failed Phase 2 Moving to Phase III Phase III AN-1792 ACC-01 Lu AE58054 Solanezumab Bapineuzumab Crenezumab EVP-6124 IVIg Dimebon Rosiglitazone Semagacestat Tarenflurbil Tramiprosate