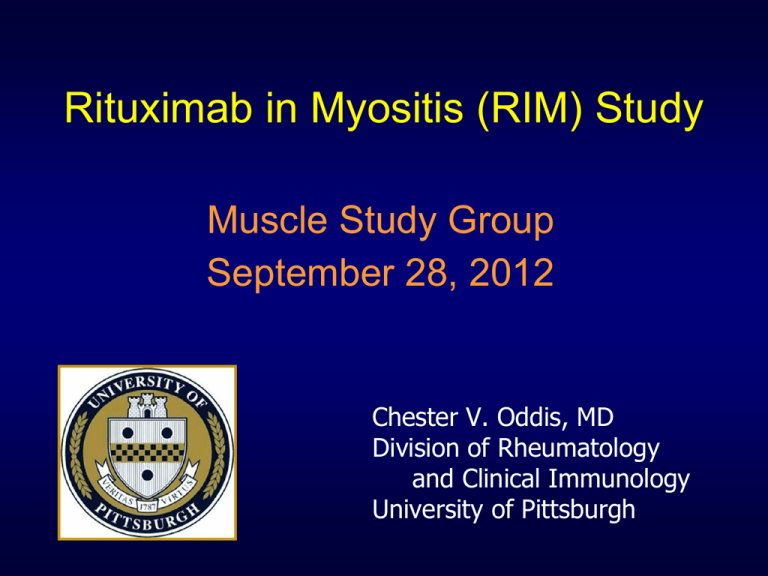
Rituximab in Myositis (RIM) Study
Muscle Study Group
September 28, 2012
Chester V. Oddis, MD
Division of Rheumatology
and Clinical Immunology
University of Pittsburgh
Disclosures
•
Genentech: Grant support and supply of
study drug; Advisory Board
Where Were We in 2000?
• Lack of consistent design in published trials
• 26 prospective myositis trials reviewed
14 adult PM-DM; 5 adult IBM; 5 JDM; 2 adult
PM/DM/IBM
• Problems with ‘current’ trials
different myositis classification criteria used
lack of uniformity with inclusion/exclusion criteria
variability in concomitant therapies
variability in trial durations and subsequent follow-up
different intervals of assessment
lack of uniformity in measures for outcome
assessments
Myositis Clinical Trials:
“Pieces of the Puzzle”
•
Establishment of IMACS
Adult/pediatric/multidisciplinary/international
•
Agreed upon outcome measures [Miller]
•
Definition(s) of improvement for myositis clinical
trials [Rider]
•
Consensus on conduct of adult and juvenile
myositis clinical trials [Oddis/Rider]
•
Assessment of disease activity and damage
[Sultan/Isenberg]
Preliminary DOI for IIM Clinical Trials
3 of any 6 CSM improved by ≥ 20%, with
no more than 2 CSM worsening by ≥ 25%
(cannot include MMT)
Rider, Arth Rheum, 2004
DOI not just a consensus definition, but
partially validated using previous adult trial
data (n=4) and pediatric natural history data
Rituximab in Myositis
Rituximab in the Treatment of Refractory Adult and
Juvenile Dermatomyositis and Adult Polymyositis
Chester V. Oddis, MD
Ann M. Reed, MD
and the RIM Study Group
RIM Study: Aim
To examine the efficacy of rituximab, a B
cell depleting agent, in refractory adult and
juvenile myositis patients in a multicenter
44-week clinical trial enrolling 76 adult PM,
76 adult DM and 50 JDM patients
Inclusion Criteria
Definite or probable PM or JDM/DM (by
Bohan and Peter criteria)
1.
All patients with PM required verification of
diagnosis by a 3-member Adjudication
Committee
Included medical record review and muscle
biopsy review by a neuropathologist
Inclusion Criteria
2. Refractory myositis = Intolerance to or an
inadequate response to corticosteroids plus at
least one other immunosuppressive (IS) agent
3. Adult PM or DM required Manual Muscle
Testing-8 (MMT-8) score ≤ 125/150 and 2 other
abnormal Core Set Measures (CSM)
JDM could enter by the same criteria as adults
or if MMT-8 >125 then they required 3 other
abnormal CSM
Manual Muscle Testing-8 (MMT-8)
Muscle Groups
Right (0 – 10)
Left (0 – 10)
Axial (0 – 10)
Axial Muscles (0 – 10)
Neck Flexors
0-10
Proximal Muscles (0 – 100)
Deltoid
0-10
0-10
Biceps brachii
0-10
0-10
Gluteus maximus
0-10
0-10
Gluteus medius
0-10
0-10
Quadriceps
0-10
0-10
Distal Muscles (0 – 40)
Wrist Extensors
0-10
0-10
Ankle dorsiflexors
0-10
0-10
MMT-8 score (0 – 150)
0-70
0-70
0-10
Set of 8 muscle groups with a maximum score = 150
RIM Study: 5 Additional Core Set Measures
Domain
Core Set Measures
Physician global VAS ≥ 2.0 on 10cm scale
Global Activity
Patient/Parent global VAS ≥ 2.0 on 10cm scale
Physical Function
Laboratory
Assessment
Extramuscular
Disease
CHAQ/HAQ disability index ≥ 0.25
At least one muscle enzyme
(CK/AST/ALT/LDH/aldolase) ≥ 1.3x ULN
Global extramuscular disease activity VAS ≥ 1.0 on
the Myositis Disease Activity Assessment Tool
(MDAAT)
– constitutional, cutaneous, articular, GI, pulmonary,
cardiac
Inclusion Criteria
4. Stable prednisone dose for 4 weeks prior to
screening visit
5. Background therapy with at least 1 other IS
agent at stable dose for at least 6 weeks
prior to screening visit was encouraged
Randomized Placebo Phase Design
(RPPD)
Wk 0
Wk 1
Wk 8
Wk 9
Wk 4
Screen
Rtx Early
Rtx Late
Rituximab
Wk 44
Placebo
Wks 12 – 44
(8 additional visits)
Placebo-controlled
Double Blind Phase
Placebo
•
•
•
•
•
Wk 12
Rituximab
Subjects randomly assigned, double-blind, to ‘Rtx Early’ or ‘Rtx Late’
½ subjects receive drug early and ½ subjects receive drug 8 wks later
Week 8: reflects a ‘randomized placebo-controlled trial’
No corticosteroids at time of the 4 infusions
14 visits (specimens/CSM) over 44 weeks
Participant Flow Diagram
MMT>125
Low IgG/IgM
200 randomized and 195 included in final analysis
Rituximab Dosing
• Children received 575mg/m2 up to a
maximum dose of 1gm 1 week apart
• Adults received 750mg/m2 BSA up to a
maximum dose of 1gm 1 week apart
. Patient Baseline Demographic and Clinical Characteristics
Early Rituximab
(n=96)
Late Rituximab
(n=104)
p value
62 (65)
81 (78)
0.05
Mean age (SD)
43 (18.2)
40 (18.4)
0.36
Female sex (%)
68 (71)
78 (75)
0.61
37/36/23 (n=96)
39/40/25 (n=104)
0.99
Mean disease duration (SD)
5.2 yrs (6.5)
5.4 years (6.0)
0.78
Mean prednisone dose (SD)
19.7 (12.1)
21.4 (14.4)
0.39
Non-corticosteroid
immunosuppressive use (%)
84 (88)
89 (86)
0.85
Myositis autoantibody positivity (%)
Anti-synthetase
Anti-SRP
DM-associated*
Other autoantibody#
16 (17.8)
13 (14.4)
33 (36.7)
8 (8.9)
16 (15.8)
12 (11.9)
38 (37.6)
16 (15.8)
0.65
None of the above
20 (22.2)
19 (18.8)
6
3
Characteristic
Caucasian race (%)
IIM subset (PM/DM/JDM)
Undefined autoantibody+
Baseline Core Set Measures
(Mean/SD)
Early Rituximab
(n=96)
Late Rituximab
(n=104)
p value
71 (11.4)
71.7 (13.0)
0.70
MD Global VAS
(0-100 mm)
51.4 (17.6)
49.2 (17.4)
0.37
Patient/Parent Global VAS
(0-100mm)
65.4 (20.3)
65.6 (21.7)
0.94
HAQ/CHAQ Disability Index
(0-3)
1.55 (.7)
1.53 (0.8)
0.84
Muscle enzyme x ULN
9.5 (14.9)
5.5 (9.0)
0.03
Extramuscular Score VAS
(0-100 mm)
27.4 (20.4)
30.7 (19.5)
0.25
Characteristic
MMT-8 ratio
MMT-8 ratio refers to recorded MMT-8/total possible score for muscles tested
Data Quality
• Very low patient dropout
– 5 pts with baseline visit and no subsequent
measurements
– 195 randomized pts included in analysis
• Excellent quality of data
• Very little missing data
– Percentage of missing values = 1.2%
B cell Numbers Before and After Rituximab
Early Rtx
LateRtx
DOI for RIM Study
≥ 20% improvement in 3 of any 6 CSM,
no more than 2 CSM worsening by ≥ 25%
(excluding MMT)
To meet DOI subjects had to satisfy
criteria on 2 consecutive visits
Primary Endpoint and Hypothesis
•
Primary Endpoint: Compare the time to DOI
between the ‘Rtx Early’ and ‘Rtx Late’ groups
•
Hypothesis: The time to DOI will be statistically
less (shorter) in early vs. late treatment groups
Primary Outcome: Entire Cohort
Median time to DOI:
Early Rtx = 20.0 weeks
Late Rtx = 20.2 weeks
p = 0.74 (log rank)
Primary Outcome:
Adult PM
Median time to DOI:
Early Rtx = 21.8 weeks
Late Rtx = 24.0 weeks
p = 0.43 (log rank)
Primary Outcome:
Adult DM
Median time to DOI:
Early Rtx = 20.4 weeks
Late Rtx = 20.3 weeks
p = 0.70 (log rank)
Primary Outcome: JDM
Median time to DOI:
Early Rtx = 11.7 weeks
Late Rtx = 19.6 weeks
p = 0.32 (log rank)
Secondary Endpoints and Hypotheses
•
Secondary Endpoint II: Compare the response rates
(proportion of patients achieving DOI) at week 8 in early
vs. late groups
Hypothesis: The response rate will be significantly
higher in the early group at week 8
Secondary Endpoint II
Proportions of Patients Meeting DOI at Week 8
25%
Early Rtx
Late Rtx
20%
20.6%
15%
10%
5%
0%
15%
Patients Meeting DOI During Trial
100%
80%
60%
40%
20%
0%
Early Rtx
Late Rtx
80%
85%
Overall, 83% (161/195) of subjects met the DOI
during the course of the 44-week clinical trial
Corticosteroid Sparing Effect
Mean Total Daily Dose (mg)
25
p < 0.001
20
21
15
13.8
10
5
0
wk 0
wk 44
Timepoint
There was a significant difference in the mean
corticosteroid dose at baseline compared to the final visit
Retreatment With Rituximab
• 10 subjects (9 evaluable) met criteria for
re-treatment with Rtx
• 4 were in ‘Early’ and 5 in ‘Late’ Rtx groups
Weeks to Initial DOI
(mean, n=9)
Weeks from DOI to
DOW
(mean, n=9)
Weeks to Re-treatment
DOI
(mean, n=8)
12.4
16.5
19.9
Adverse Events
• 52/200 (26%) subjects had 68 serious adverse
events (SAE)
– 40% of those were reported as related to treatment
• Most common SAEs included:
– infection (25%)
– musculoskeletal (18%)
– GI (12%)
– cardiac (7%)
• 1 death (unrelated to drug)
• No cases of PML
Summary
• The primary and secondary endpoints were not
achieved in the RIM Study
• 83% of refractory adult and juvenile myositis
patients met the DOI in this trial
• There was a significant corticosteroid sparing
effect noted in this trial between the baseline dose
and the dose at study conclusion
• Rituximab was generally well tolerated
RIM Study Conclusions
• Overestimate of the rituximab effect
– SC postulated >50% would meet DOI by 8 weeks
One-half responded by 20 weeks (lower potency)
• Underestimate of placebo effect
• Short placebo phase of 8 weeks
• Heterogeneity of myositis
– Increased variance around time to DOI in both arms
• Subjective CSM (partially validated)
What about more stringent
criteria for improvement?
• At least 4 CSM improving by 40%
Entire Cohort: Time to Stringent DOI
Early Rtx
Late Rtx
p=0.13 (Peto-Peto test)
p=0.18 (log rank)
RIM Study Autoantibodies
Autoantibody
Synthetase
SRP
DM-associated
Number (%)
32 (16%)
- 28 Jo-1
25 (13%)
71 (35%)
- 26 Mi-2
- 23 TIF1-gamma
- 22 MJ
Overlap/other autoAb
No MAA
24 (12%)
40 (20%)
Undefined
Total
9 (4%)
200
Survival distribution function
Baseline Autoantibodies Predict Outcome
Autoantibody subsets
• anti-SynAb
- HR 2.3 (1.3 – 4.2), p value = 0.01
• DM Abs: TIF-1/MJ/Mi-2
- HR 1.9 (1.2 – 3.1), p value = 0.01
no autoAb (21%)
anti-SRP (13%)
other autoAb (14%)
DM:TIF-1/MJ/Mi-2 (33%)
anti-syn Ab (14%)
Time in weeks
Anti-syn & DM Abs predicted a better outcome, but anti-SRP and those
without MAAs had a worse outcome
Median Time to Stringent DOI: Jo-1 vs non-Jo-1
Median time to stringent DOI
in Early = 27.9 weeks
Early vs Late
p=0.12 (log rank)
Other Univariate Predictors
• Caucasians showed a better response (p=0.04)
• Higher baseline VAS for extramuscular activity
was only CSM predictive of better response
(p=0.02)
• Higher baseline VAS muscle damage score
predicted a poor response (p=0.05)
Aggarwal, Arth Rheum 62: S385, 2010
Future Directions
• Study the ‘immunology’ of the response in
the specimens obtained from RIM and
correlate this to the clinical outcomes
• Assess other biomarkers from the
specimen repository
• Re-examination of the DOI and the
response criteria
Participating Centers
Foreign Centers
Participating Centers
Adult Sites
Alabama (Fessler)
Boston (Narayanaswami)
Czechoslovakia (Vencovsky)
Dallas (Olsen)
Kansas City (Barohn/Latinis)
Kentucky (Crofford)
London (Isenberg)
Mayo Clinic (Ytterberg)
Miami (Sharma)
Michigan (Seibold/Schiopu)
Michigan State (Martin/Eggebeen)
Milwaukee (Cronin)
New York: North Shore (Marder)
New York: HSS (DiMartino)
NIH (Miller)
Philadelphia (Kolasinski)
Phoenix (Levine)
Pittsburgh (Oddis/Ascherman)
Stanford (Chung/Fiorentino)
Sweden (Lundberg)
UCLA (Weisman/Venuturupalli)
Pediatric Sites
Boston (Kim)
Cincinnati (Lovell)
Duke (Rabinovich)
Mayo Clinic (Reed)
Miami (Rivas-Chacon)
Michigan State (Martin/Eggebeen)
NIH (Rider)
Nova Scotia (Huber)
Philadelphia (Sherry)
Pittsburgh (Kietz)
Stanford (Sandborg)
Toronto (Feldman)
Our Patients!!!
Acknowledgements
Coordinating Center
Dana Ascherman, MD
Rohit Aggarwal, MD
Sherrie Pryber, Project Manager
Diane Koontz, Project Manager
Noreen Fertig, BS
Kelly Reckley, BS
Maureen Laffoon, BS
Xinyan Gu
IDS Pharmacy
David Lacomis, MD
Jonette Werley, BA, HT, HTL
Christopher Bise, MS, PT
Supported by:
Study Partners
Steering Committee
Ann Reed, MD
Steve Ytterberg, MD
Dana Ascherman, MD
David Lacomis, MD
Brian Feldman, MD
Fred Miller, MD, PhD
Lisa Rider, MD
Todd Levine, MD
Steve Belle, PhD
Howard Rockette, PhD
Michael Harris-Love,MPT
Data Center
Howard Rockette, PhD
Steven Belle, PhD
Sharon Lawlor, MBA
Stephanie Kelley, MS
Other Collaborators
The RIM Study Group
RIM Study Coordinators
David Isenberg, MD, FRCP
Myositis Working Group
The Myositis Association
RIM Publication Committee
IMACS