View Powerpoint

The Importance of Residual
Renal Function
Dr Paul Tam
June 11, 2010
RRF, an important predictor of survival in dialysis patients
Loss of RRF
Inflammation
Resting hypermetabolism
Cardiovascular
Disease
Malnutrition
Increased Mortality and Cardiovascular Death
Importance of RRF
• Average GFR at dialysis initiation : 6.6 to 8.0 ml/min (USRDS 99 Annual Data Report
• Each 1ml/min of residual renal GFR translate into CCr of 10 L/Week and Kt/v urea of 0.25 to
0.3/Week (70kg male)
• Improved clinical outcomes with better small solute clearences
Importance of RRF
• Reanalysis of CANUSA study: For each 5L/wk/1.7.73 m increment in GFR; there was 12% decrease in RR of death. (RR0.88; Cl 0.83-0.94)
• No association with peritoneal creatinine clearance (RR
1.0, Cl 0.9-1.10)
• Peritoneal and renal clearance not equivalent
• 24 h urine volume is even more important than GFR
(250ml/day 36% in RR of deaths)
Bargman et al. J am Soc Nephrol 12:2158-2158-2162, 2001
ADEquacy of Peritoneal Dialysis in
MEXico (ADEMEX) study
• Residual renal and peritoneal dialysis clearance are not equivalent and thus not simply additive.
• Increasing peritoneal solute clearence showed no beneficial effect on survival in PD patients.
• Residual renal function was predictive of outcome.
Paniagua et al. Am Soc Nephrol, 2002
Clearance effect on outcomes in PD
Maiorca et al. (1995)
Fung (1996)
Davies (1998)
Clearence effect on outcomes n Study Type Total Peritoneal Renal
68 Observational Yes, NE Yes
31 Observational Yes
210 Observational Yes, no
NE
NE
Yes
Yes
Diaz-Buxo et al. (1999) 673 Observational
Merkus (2000)
Jager et al. (1999)
Szeto et al. (1999)
Szeto et al. (2000)
Mak et al. (2000)
Rocco et al. (2000)
Szeto et al. (2001)
Bargman (2001)
106 Observational
118 Observational
168
270
82
873
140
601
Observational
Observational
Interventional
Observational
Observational
Observational
NE
NE
NE
Yes
Yes
Yes
NE
NE
NE
No
No
No
NE
No
NE
No
Yes
No
Yes
Yes
Yes
NE
Yes
NE
Yes
NE
Yes
Patient survival Termorshuizen et al. J Am Soc Nephrol 2004
Age at entry (yr)
RR
1.03
95% CI P Value
1.02 to 1.05
<0.0001
0.84
0.64 to 1.10
0.2098
Male gender
Davies’ comorbidity score at entry high 4.74
2.35
1.00 ref
3.04 to 7.40
1.63 to 3.39
<0.0001
intermediate low
Primary kidney disease diabetes glomerulonephritis renal vascular disease
1.43
0.67
1.18
0.98 to 2.09
0.38 to 1.20
0.86 to 1.62
0.0855
others
Albumin baseline (for each 0.1 g/dl increase) b
SGA (scale 1 –7) at baseline
BMI (kg/m 2 )
Dialysis sp- rKt/V urea
(L/wk))
1.00 ref
0.98
0.89
0.96
0.76
0.95 to 1.01
0.80 to 0.99
0.93 to 0.99
0.64 to 0.92
0.1355
0.0389
0.0252
0.0035
Residual rKt/V urea
(L/wk) 0.44
0.30 to 0.65
<0.0001
The residual renal function (rKt/V urea
) and dose of dialysis (sp-dKt/V urea
) werLe included as time-dependent variables. RR, relative risk; CI, confidence interval.
The effect of single-pool Kt/Vurea (sp-dKt/Vurea) on mortality by presence of residual renal function (rKt/Vurea = 0 ["anurics'" versus rKt/Vurea >0)
Termorshuizen, F. et al. J Am Soc Nephrol 2004
Potential mechanisms of benefit of RRF in dialysis
Effects of additional of dialysis clearences to a glomerular filtration rate of 5ml/min
Solute
Clearence
Urea
Renal HD and Renal-PD and renal renal
4 17 4 10
Creatinine
Para aminohippuric acid
Inulin
B2microglobulin
6 16
20 26
5 5.4
5 5.7
6
20
5
11
23
8
5 6
Krediet, KI 2006
100
80
60
Peritoneal
Renal
40
20
0
UN Cr P B2M p-cresol
Peritoneal, renal, and total clearances of urea nitrogen
(UN), creatinine (Cr), phosphate (P),
2
-microglobulin (
B2M), and p-cresol.
Bammens et al. Kidney International (2003) 64, 2238 –2243
Residual renal function
Resting energy expenditure
Removal of middle moleculer uremic toxins
Toxins, such as p-cresol
Inflammation
Clearence of urea and creatinine
Sodium and fluid removal
P removal
EPO production
Cardiac hyperthyrophy
Atherosclerosis and arteriosclerosis
malnutrition
Vascular and valvular calcification
Overall and cardiovascular mortality
Quality of life
Wang and Lai KI 2006
Fig. ECW in patients with rGFR <2 and >2 ml/min
ECW:extracellular volume determined by bromide dilution, corrected for height. the 25th–75th percentile range
(line across box=median).
Capped bars: minimum and maximal values
(with exception of outliers).
Konings, C. J. A. M. et al. Nephrol. Dial. Transplant. 2003 18:797-803;
Left Ventricular Mass in Chronic
Kidney Disease and ESRD
“A new paradigm of therapy for CKD and
ESRD that places prevention and reversal of LVH and cardiac fibrosis as a high priority is needed.”
Richard J. Glassock et al, CJASN 4: s79-91s
Mean arterial pressure and RRF over time from initiation of peritoneal dialysis
Menon, M. K. et al. Nephrol. Dial. Transplant. 2001 16:2207-2213;
Nutritional parameters in patients with and RRF
Suda, T. et al. Nephrol. Dial. Transplant. 2000 15:396-401
Is the rate of decline of RRF between HD and PD different?
CCr ml/min
5
4.5
4
3.5
3
2.5
2
1.5
1
0.5
0 start 6 mo 12 mo 18 mo
Residual renal function is preserved longer in peritoneal dialysis
(PD )
Rottembourg J. Perit Dial Bull 1986
PD n:25
HD n:25
PD
HD
HD
PD
A B
Figure:Unadjusted (A) and adjusted (B) residual glomerular filtration rate (rGFR) values SE at the start of dialysis treatment, and at 3, 6 and 12 months after the start of dialysis treatment.
Jansen et al KI 2002
Decline of residual renal function is faster on
HD than on PD
Study Type
Rottembourg Prospective
HD/PD patients (n)
25/25
Difference in rate of decline
80%
Lysaght et al Retrospective 57/58
Misra et al.
Retrospective 40/103
Lang Prospective 30/15
Jansen et al Prospective 279/243
50%
69%
69%
24%
Does PD have a protective effect on RRF?
• Less abrupt fluctuations in volume and osmotic load in PD
• Intradialytic hypotension and volume fluctations in HD
• Patients on PD are in slightly volume-expanded state
• Bioincompatible membranes in HD
• PD might delay the progression of advanced renal failure
Do biocompatible PD solutions or biocompatible dialyser membranes have any advantage in relation to RRF?
The Euro-Balance Trial
P Urea Cl L/day
Group 1
SPDF (n =
36)
8.1
U Urea Cl L/day 3.8
Kt/V
P Cr Cl L/day
2.23
6.1
U Cr Cl L/day
T Cr Cl
L/wk/1.73m
2
4.9
76.5)
UF 24 hours mL 1350
U Volume mL/day 875
D/PCr 4hrs
Weight kg
0.59
70.0
Systolic BP mm Hg 135
Diastolic BP mm Hg 80
Group 1 balance
(n = 36)
P
7.8
Group 2 balance
(n = 35)
NS 8.2
3.9
2.33
S
NS
3.7
2.31
6.2
5.2
78.6
NS
Ns
NS
6.1
4.5
75.4
Group
2 SPDF
(n = 35)
P
8.4
NS
2.7
S
2.22
S
5.9
3.5
67.1
S
NS
S
995
925
0.63
S 0.60
71.25
NS 78.0
130
81
S 1025
NS 919
1185
660
0.56
78.0
Ns 130 133
NS 80 81
Williams et al KI 2004
S
S
S
NS
NS
NS
Dialysis adequacy, residual renal function and nutritional indices
Control group
4 weeks 52 weeks
Balance group
4 weeks 52 weeks
6.08 ± 0.40
6.42 ± 0.83
6.08 ± 0.41
6.17 ± 0.57
PD exchange volume (l/day)
Glucose load
(g/day)
100.9 ± 17.7 106.7 ± 24.9 100.7 ± 14.6
106.2 ± 23.7
Total Kt/V 2.23 ± 0.62
2.12 ± 0.32
2.28 ± 0.35
2.16 ± 0.56
Ultrafiltration (l/day) 0.56 ± 0.69
0.77 ± 0.59
0.56 ± 0.60
0.83 ± 0.56
Urine output (l/day) 0.90 ± 0.71
0.69 ± 0.52
0.87 ± 0.62
0.80 ± 0.60
Residual GFR
(ml/min/1.73 m 2 )
3.67 ± 2.27
2.81 ± 2.87
3.91 ± 2.09
Serum albumin (g/l) 36.5 ± 4.1
35.7 ± 3.2
32.8 ± 4.4
2.72
34.3
±
±
2.08
4.2
Szeto et al. NDT 2007
Effect of biocompatible (B) vs standard (S) PD solutions on RRF (mean of urea and nCrCl)
Fan et al KI 2008
Effect of biocompatible (B) vs standard (S) PD solutions on 24-h Uvol (mean/s.e.m.).
Fan et al KI 2008
Coles et al. 1994
New multicompartmental PD fluids
Pts Study Type Month (PDF) RRF
46 CAPD-Prosp,Rand., paral..
2 (Physioneal) =
Tranaeus et al
1998
Fan et al 2008
Feriani et al
1998
Haas et al.2003
106 CAPD-Prosp.,Rand., paral.
30
28 ped.
CAPD-Prosp.,
Rand., crossover
APD-Prosp.,
Rand., crossover
6(Physioneal)
12 APD-Prosp.,Rand., paral.
12(Physioneal) =
Rippe et al. 2001 20 CAPD-Prosp.,Rand., paral.
24(Gambrosol trio)
Williamset al
2004
86 CAPD-Prosp.,Rand., crossover,paral.
6 (Balance)
Szeto et al. 2007 50 CAPD-Prosp.,Rand., paral.
12 (Balance)
6(BicaVera)
6(BicaVera)
=
=
=
=
=
Preserving residual renal function in peritoneal dialysis: volume or biocompatibility?
Davies, Simon NDT 23, June 2009
24, 2620-2622
Majority of studies indicate
RRF is relatively well preserved with PD in comparison to HD
Davies, Simon NDT 23, June 2009
24, 2620-2622
Studies Reviewed
Davies, Simon NDT 23, June 2009
24, 2620-2622
Hypothesis????
• Relative stability of volume in PD, where as HD fluctuations in volume are common
• Biocompatibility of the dialysis fluids
“The new biocompatible solutions may help preserve RRF, but the mechanisism is not certain and an inadvert effect on fluid status seems likely – at least in some of the studies.”
Davies, Simon NDT 23, June 2009
24, 2620-2622
Low-GDP Fluid (Gambrosol
Trio) Attenuates Decline of
Residual Renal Function
(RRF) in PD Patients: A
Prospective Randomized
Study
(DIUREST Study)
NDT March 2010
Background
• Clinical study in PD patients regarding content of GDP on PD fluid and its influence on the decline of RRF
• RRF impacts outcome & survival of PD patients
• Morbidity, poor nutrition & fluid overload associated with decline of RRF
• Glucose degradation products (GDPs):
– Affect cell system and tissues
– Act as precursors of advanced glycosylation endproducts
(AGEs) locally and systemically
Methods
• Study design
– A Multicentre, prospective, randomized, controlled, open, parallel, 18 month study
• 80 patients randomized
– through stratification for the presence of diabetes
Inclusion
Age: 18-80 with ESRD
GFR ≥ 3mL/min or CrCl ≥ 6mL/min
HBV, HCV, HIV negative
Exclusion
Pregnancy or lactating subjects
Several peritonitis episodes
Cancer
• Study centers in:
– Germany(15)
– France (7)
– Austria (1)
• Solutions
– Treatment solution
• Gambrosol trio
– Control (Standard) solution:
• Gambrosol (50% of patients)
• Stay-safe (31% of patients)
• Dianeal (19% of patients)
• Follow-up
– 4 - 6 weeks
• Serum U & Cr, CRP, T. Protein, albumin, lytes, phosphate
• 24 Hr. Urine: CrCl & UrCl
• BP & Wt
• UF
– At 1, 6, 12, 18 months
• CA125
• Personal Dialysis Capacity (PDC)
Medications:
• ACE & ARBs
• Diuretics
• Phosphate binders
Results
• Subjects
44 (Treatment: 1 was intend-to-treat)
– Recruited: 80
36 (Standard)
– Median exposure time: Treatment solution 17.8 m
Standard solution 16.3 m
– Dropout: 11 before first RRF measurement
– N=69 with 2.4% /month dropout rate
Low GDP Standard P- value
RRF
24 Hr. Urine Decline
Phosphate Level
Albumin
CRP
CA125
PDC
Peritonitis Episode
1.5 % 4.3 %
12mL/month 38mL/month
Difference: 26mL/month (0.86mL/day)
Increased by 0.0135mg/dL/month
( 0.004 mmol/L )
Increased by 0.0607mg/dL/month
( 0.02 mmol/L )
Difference: 0.016 mmol/L per month
3.74 g/dL
(37.4 g/L)
3.72 g/dL
(37.2 g/L)
0.78 mg/dL
(7.8 mg/L)
61.2U/mL
1.28 mg/dL
(12.8 mg/L)
18.7U/mL
21699± 5485 cm/1.73m
2 20028±6685cm/1.73m
2 p=0.0437
p= 0.0241
p=0.0381
P=0.90
P=0.42
p<0.001
No important changes
1 per 36.4 patient months
11 of 43 (25.6%)
1 per 39.7 patient months
6 of 26 (23.7%)
P= 0.815
SIG
NS
NS
SIG
NS
NS
Clinical
Signifi cance
SIG
SIG
Clinical Significance
• RRF: Treatment group higher by 2.3 ml/min/1.73 m 2
• 24 H Urine volume: less decline in Treatment group by three-fold
• Phosphate control: better in Treatment group by five-fold
• CA125: higher levels in Treatment group
• UF volumes not conclusive due to unreliability of data
• D/P & PDC parameters no significant changes, possibly due to patient dropout & missing data
Limitations
• Inconsistency in control group (?)
• Patients’ selection: incident & prevalent patients
• Large dropout rate
• Unreliability of data on UF & D/P properties
• Consistency issue with testing of CA125
• Effects of different antihypertensive use with their potential effect on RRF
Strategies for preservation of RRF
• Avoidance of hypovolemia
• Avoidance of potentially nephrotoxic drugs
• The use of high dose of loop diuretics
• The use of an ACE inhibitor or A-II reseptor antogonist
• Starting dialysis with PD
In HD patients
• Prevention of intradialytic hypotensive episodes
• Developing a highly biocompatible
HD system including a synthetic membrane and ultrapure dialysis fluid.
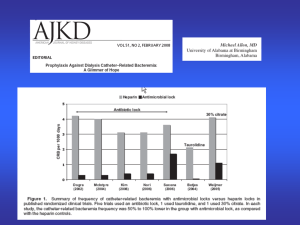
Biocompability of dialyser membranes n Study Type Predictor Decline in RRF
Caramelo et al.
1994
22 Prosp.Rand.
CPvsPAN/PS NS
Van Stone. 1995
Hakim et al
1996
Hartmann et al.
1997
McCarthy et al 1997
Mois et al.2000
Lang et al.2001
Jansen et al.
2002
334 Retrosp.
CPvsPS/PMMA/C
A
159 Prosp.,Rand
.
UC vs PMMA
CA vs PS 20 Prosp.,Rand
.
100 Retrosp.
814
30
270
Retrosp.
Prosp.,Rand
.
Prosp.
CA vs PS
A faster rate with CP
NS
A faster rate with CA
A faster rate with CA
UC vsMC/synthetic
CP vs PS
NS
A faster rate with PS
MC vs synthetic NS at 3 months
In PD patients
• Prevention of hypotension and fluid volume depletion
• Optimization of blood pressure control
• Usage of biocompatible and smoother ultrafiltration profile
• Preservation of peritoneal permeability capacity
• Prevention of peritoneal dialysis-related peritonitis
Conclusion
The potential benefits of RRF
• Better clearence of middle and larger molecular weights toxins,
• Better volume and blood pressure control
• Improved appetite and nutritional status
• Relative preservation of renal endocrine functions
• Improved phosphate control
• Improved quality of life